Thymoma overview: Difference between revisions
Amr Marawan (talk | contribs) No edit summary |
Amr Marawan (talk | contribs) No edit summary |
||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Thymoma]] is the | [[Thymoma]] is the most common tumor of the anterior mediastinum, originating from the [[epithelial cells]] of the [[thymus]]. The thymus gland is located behind the sternum in front of the great vessels; it reaches its maximum weight at puberty and undergoes involution thereafter. | ||
[[Thymoma]] consists of any type of thymic [[epithelial cell]] as well as [[lymphocyte]]s that are usually abundant and probably not [[neoplastic]]. Thymoma usually is [[benign]], and frequently encapsulated uncommon tumor, best known for its association with the neuromuscular disorder [[myasthenia gravis]]. Thymoma is found in 15% of patients with [[myasthenia gravis]]. Once diagnosed, thymomas may be removed surgically. When occasionally [[malignant]], then it is [[invasive]]: [[metastasis]] is extremely rare. In the rare case of a malignant tumor, chemotherapy may be used. | [[Thymoma]] consists of any type of thymic [[epithelial cell]] as well as [[lymphocyte]]s that are usually abundant and probably not [[neoplastic]]. Thymoma usually is [[benign]], and frequently encapsulated uncommon tumor, best known for its association with the neuromuscular disorder [[myasthenia gravis]]. Thymoma is found in 15% of patients with [[myasthenia gravis]]. Once diagnosed, thymomas may be removed surgically. When occasionally [[malignant]], then it is [[invasive]]: [[metastasis]] is extremely rare. In the rare case of a malignant tumor, chemotherapy may be used. | ||
Revision as of 19:59, 19 February 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Amr Marawan, M.D. [2]
|
Thymoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Thymoma overview On the Web |
|
American Roentgen Ray Society Images of Thymoma overview |
Overview
Thymoma is the most common tumor of the anterior mediastinum, originating from the epithelial cells of the thymus. The thymus gland is located behind the sternum in front of the great vessels; it reaches its maximum weight at puberty and undergoes involution thereafter.
Thymoma consists of any type of thymic epithelial cell as well as lymphocytes that are usually abundant and probably not neoplastic. Thymoma usually is benign, and frequently encapsulated uncommon tumor, best known for its association with the neuromuscular disorder myasthenia gravis. Thymoma is found in 15% of patients with myasthenia gravis. Once diagnosed, thymomas may be removed surgically. When occasionally malignant, then it is invasive: metastasis is extremely rare. In the rare case of a malignant tumor, chemotherapy may be used.
Malignant lymphomas that involve the thymus, e.g., lymphosarcoma, Hodgkin's disease (termed "granulomatous thymoma" in the past), should not be regarded as thymoma.[1]
Thymomas associated with autoimmune disorders usually are benign. Malignant thymomas can metastasize, generally to pleura, kidney, bone, liver or brain.[2]
-
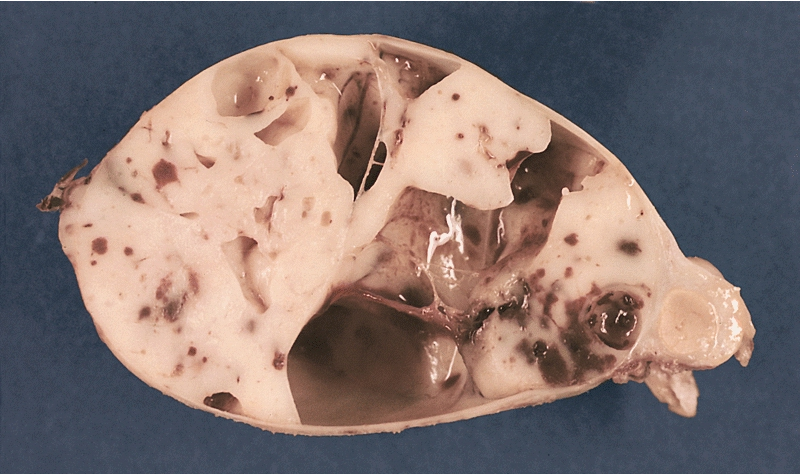
MEDIASTINUM: ENCAPSULATED CYSTIC THYMOMA. Post-formalin-fixed cut surface reveals an ivory-colored tumor with multiple cystic spaces varying from pin-head sized to a few centimeters in diameter. Small hemorrhages are also noted
References
- ↑ Thomas CR, Wright CD, Loehrer PJ (1999). "Thymoma: state of the art". J. Clin. Oncol. 17 (7): 2280–9. PMID 10561285.
- ↑ Thomas CR, Wright CD, Loehrer PJ (1999). "Thymoma: state of the art". Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 17 (7): 2280–9. PMID 10561285. Retrieved 2012-01-18. Unknown parameter
|month=ignored (help)