Spontaneous coronary artery dissection angiography: Difference between revisions
Arzu Kalayci (talk | contribs) No edit summary |
|||
| (17 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Spontaneous coronary artery dissection}} | {{Spontaneous coronary artery dissection}} | ||
{{CMG}}; {{AE}}{{NRM}} | {{CMG}}; {{AE}} {{NRM}}; {{AKK}} | ||
{{SK}} SCAD | {{SK}} SCAD | ||
| Line 7: | Line 7: | ||
==Overview== | ==Overview== | ||
The current [[gold standard]] for diagnosing [[spontaneous coronary artery dissection ]] ([[SCAD]]) is [[coronary angiography]], as it is widely available and the first-line [[imaging]] modality for [[patients]] presenting with the [[acute coronary syndrome]]. The predominant [[angiographic]] feature of [[SCAD]] consists of diffuse smooth narrowing of varying severity involving mid-to-distal [[coronary]] segments, secondary to compression of the true [[lumen]] and/or expansion of the false [[lumen]] by the development of an intramural [[hematoma]]. The typical appearance of extraluminal contrast staining, multiple radiolucent [[lumens]], spiral [[dissection]], or [[intraluminal]] filling defects is less commonly observed. Other [[angiographic]] findings associated with [[SCAD]] include [[coronary tortuosity]], [[myocardial bridging]], and [[fibromuscular dysplasia|coronary fibromuscular dysplasia]]. | |||
==Angiography== | ==Angiography== | ||
[[Angiographic]] findings include:<ref name="KimLongo2020">{{cite journal|last1=Kim|first1=Esther S.H.|last2=Longo|first2=Dan L.|title=Spontaneous Coronary-Artery Dissection|journal=New England Journal of Medicine|volume=383|issue=24|year=2020|pages=2358–2370|issn=0028-4793|doi=10.1056/NEJMra2001524}}</ref> | |||
* '''Type 1:''' appearance on an angiography involves the presence of two intraluminal streams/lumens separated by a | * '''Type 1:''' appearance on an [[angiography]] involves the presence of two [[intraluminal]] streams/lumens separated by a [[radiolucent flap]] of the [[intima]]. | ||
* '''Type 2:''' when the dissection plane is deeper in the vessel wall between the media and adventitial layers, formation of a [[hematoma]] can result in luminal narrowing which is seen as | * '''Type 2:''' when the [[dissection]] plane is deeper in the [[vessel]] wall between the media and [[adventitial]] layers, the formation of a [[hematoma]] can result in [[luminal]] narrowing which is seen as [[stenosis]] on [[angiography]]. | ||
* '''Type 3:''' appearance mimics [[atherosclerosis]]. The dissection is typically shorter than that of type 2 (< 20 mm) and may have a hazy appearance. | * '''Type 3:''' appearance mimics [[atherosclerosis]]. The [[dissection]] is typically shorter than that of type 2 (< 20 mm) and may have a hazy appearance. To confirm this type, [[intracoronary]] [[imaging]] is required. The [[angiographic]] findings include linear and long [[lesion]] or [[coronary]] [[tortuosity]]. Another important distinguishing factor from [[atherosclerosis]] is the absence of [[atherosclerosis]] in the reminder of [[coronary]] [[vessels]]. | ||
* '''Type 4:''' [[angiographic]] finding of this type include an occluded [[artery]]. The repeat [[angiography]] is required to visualize the healed [[coronary artery]] and confirm the [[diagnosis]]. | |||
===Image=== | |||
[[Image:SCAD_çizim.png|800 px|thumb|center|'''Angiographic Classification of SCAD''']] | [[Image:SCAD_çizim.png|800 px|thumb|center|'''Angiographic Classification of SCAD''']] | ||
{{See also|Spontaneous coronary artery dissection classification}} | |||
==References== | ==References== | ||
Latest revision as of 09:49, 4 March 2021
|
Spontaneous Coronary Artery Dissection Microchapters |
|
Differentiating Spontaneous coronary artery dissection from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Type 1 Type 2A Type 2B Type 3 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Nate Michalak, B.A.; Arzu Kalayci, M.D. [2]
Synonyms and keywords: SCAD
Overview
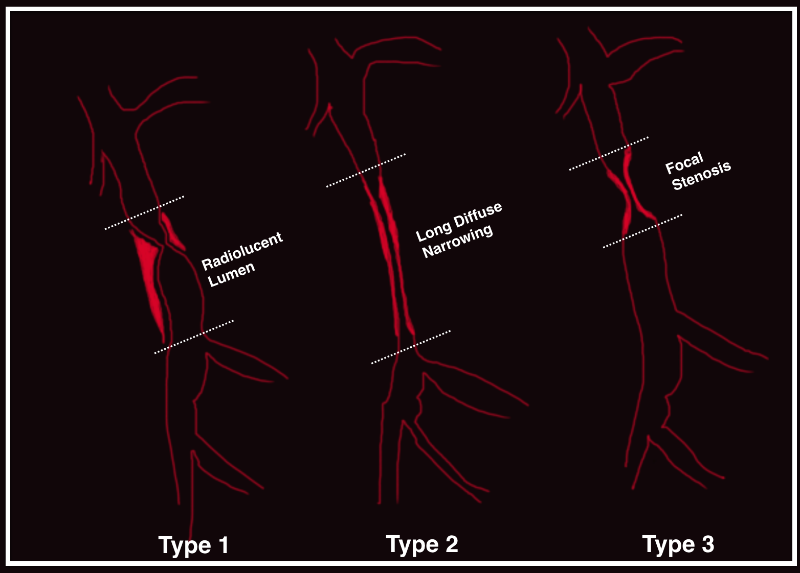
The current gold standard for diagnosing spontaneous coronary artery dissection (SCAD) is coronary angiography, as it is widely available and the first-line imaging modality for patients presenting with the acute coronary syndrome. The predominant angiographic feature of SCAD consists of diffuse smooth narrowing of varying severity involving mid-to-distal coronary segments, secondary to compression of the true lumen and/or expansion of the false lumen by the development of an intramural hematoma. The typical appearance of extraluminal contrast staining, multiple radiolucent lumens, spiral dissection, or intraluminal filling defects is less commonly observed. Other angiographic findings associated with SCAD include coronary tortuosity, myocardial bridging, and coronary fibromuscular dysplasia.
Angiography
Angiographic findings include:[1]
- Type 1: appearance on an angiography involves the presence of two intraluminal streams/lumens separated by a radiolucent flap of the intima.
- Type 2: when the dissection plane is deeper in the vessel wall between the media and adventitial layers, the formation of a hematoma can result in luminal narrowing which is seen as stenosis on angiography.
- Type 3: appearance mimics atherosclerosis. The dissection is typically shorter than that of type 2 (< 20 mm) and may have a hazy appearance. To confirm this type, intracoronary imaging is required. The angiographic findings include linear and long lesion or coronary tortuosity. Another important distinguishing factor from atherosclerosis is the absence of atherosclerosis in the reminder of coronary vessels.
- Type 4: angiographic finding of this type include an occluded artery. The repeat angiography is required to visualize the healed coronary artery and confirm the diagnosis.
Image
References
- ↑ Kim, Esther S.H.; Longo, Dan L. (2020). "Spontaneous Coronary-Artery Dissection". New England Journal of Medicine. 383 (24): 2358–2370. doi:10.1056/NEJMra2001524. ISSN 0028-4793.