Scleroderma
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Scleroderma |
|
Articles |
|---|
|
Most recent articles on Scleroderma Most cited articles on Scleroderma |
|
Media |
|
Powerpoint slides on Scleroderma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Scleroderma at Clinical Trials.gov Clinical Trials on Scleroderma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Scleroderma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Scleroderma Discussion groups on Scleroderma Patient Handouts on Scleroderma Directions to Hospitals Treating Scleroderma Risk calculators and risk factors for Scleroderma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Scleroderma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
for the heart in Scleroderma click here
Overview
Scleroderma is a rare, chronic disease characterized by excessive deposits of collagen in the skin or other organs. The localized type of the disease, while disabling, tends not to be fatal. Diffuse scleroderma or systemic sclerosis, the generalized type of the disease, can be fatal as a result of heart, kidney, lung or intestinal damage.[1]
Epidemiology
- Scleroderma affects approximately 300.000 people in the United States.
- It is four times as common in women than in men.
- Incidence rates are estimated at 2-20 per million per year in the United States.
- Juvenile scleroderma affects approximately 7.000 children in the United States.
- The most common form of Juvenile Scleroderma is Localized Scleroderma - Morphea and/or Linear.
Pathophysiology
The overproduction of collagen is thought to result from an autoimmune dysfunction, in which the immune system would start to attack the kinetochore of the chromosomes. This would lead to genetic malfunction of nearby genes. T cells accumulate in the skin; these are thought to secrete cytokines and other proteins that stimulate collagen deposition. Stimulation of the fibroblast, in particular, seems to be crucial to the disease process, and studies have converged on the potential factors that produce this effect.[2]
A significant player in the process is transforming growth factor (TGFβ). This protein appears to be overproduced, and the fibroblast (possibly in response to other stimuli) also overexpresses the receptor for this mediator. An intracellular pathway (consisting of SMAD2/SMAD3, SMAD4 and the inhibitor SMAD7) is responsible for the secondary messenger system that induces transcription of the proteins and enzymes responsible for collagen deposition. Sp1 is a transcription factor most closely studied in this context. Apart from TGFβ, connective tissue growth factor (CTGF) has a possible role.[2]
Damage to endothelium is an early abnormality in the development of scleroderma, and this too seems to be due to collagen accumulation by fibroblasts, although direct alterations by cytokines, platelet adhesion and a type II hypersensitivity reaction have similarly been implicated. Increased endothelin and decreased vasodilation has been documented.[2]
Jimenez & Derk[2] describe three theories about the development of scleroderma:
- The abnormalities are primarily due to a physical agent, and all other changes are secondary or reactive to this direct insult.
- The initial event is fetomaternal cell transfer causing microchimerism, with a second summative cause (e.g. environmental) leading to the actual development of the disease.
- Physical causes lead to phenotypic alterations in susceptible cells (e.g. due to genetic makeup), which then effectuate DNA changes which alter the cell's behavior.
Etiology
There is no clear obvious cause for scleroderma and systemic sclerosis. Genetic predisposition appears to be limited: genetic concordance is small; still, there often is a familial predisposition for autoimmune disease. Polymorphisms in COL1A2 and TGF-β1 may influence severity and development of the disease. There is limited evidence implicating cytomegalovirus (CMV) as the original epitope of the immune reaction, and organic solvents and other chemical agents have been linked with scleroderma.[2]
One of the suspected mechanisms behind the autoimmune phenomenon is the existence of microchimerism, i.e. fetal cells circulating in maternal blood, triggering an immune reaction to what is perceived as "foreign" material.[3][2]
A distinct form of scleroderma and systemic sclerosis may develop in patients with chronic renal failure. This entity, nephrogenic fibrosing dermopathy or nephrogenic systemic fibrosis,[4] has been linked to the exposure to gadolinium-containing radiocontrast.[5]
Bleomycin[6] (a chemotherapeutic agent) and possibly taxane chemotherapy[7] may cause scleroderma, and occupational exposure to solvents has been linked with an increased risk of systemic sclerosis.[8]
Types of Scleroderma
There are three major forms of scleroderma: diffuse, limited (CREST syndrome) and morphea/linear. Diffuse and limited scleroderma are both a systemic disease, whereas the linear/morphea form is localized to the skin. (Some physicians consider CREST and limited scleroderma one and the same, others treat them as two separate forms of scleroderma.) There is also a subset of the systemic form known as "systemic scleroderma sine scleroderma", meaning the usual skin involvement is not present.
Diffuse scleroderma
Diffuse scleroderma (progressive systemic sclerosis) is the most severe form - it has a rapid onset, involves more widespread skin hardening, will generally cause much internal organ damage (specifically the lungs and gastrointestinal tract), and is generally more life threatening.
Limited scleroderma/CREST syndrome
The limited form is much milder: it has a slow onset and progression, skin hardening is usually confined to the hands and face, internal organ involvement is less severe, and a much better prognosis is expected.
In typical cases of limited scleroderma, Raynaud's phenomenon may precede scleroderma by several years. Raynaud's phenomenon is due to vasoconstriction of the small arteries of exposed peripheries - particularly the hands and feet - in the cold. It is classically characterised by a triphasic colour change - first white, then blue and finally red on rewarming. The scleroderma may be limited to the fingers - known as sclerodactyly.
The limited form is often referred to as CREST syndrome.[9] "CREST" is an acronym for the five main features:
Morphea/linear scleroderma
Morphea/linear scleroderma involves isolated patches of hardened skin - there generally is no internal organ involvement.[10]
Diagnosis
Diagnosis is by clinical suspicion, presence of autoantibodies (specifically anti-centromere and anti-scl70/anti-topoisomerase antibodies) and occasionally by biopsy. Of the antibodies, 90% have a detectable anti-nuclear antibody. Anti-centromere antibody is more common in the limited form (80-90%) than in the systemic form (10%), and anti-scl70 is more common in the diffuse form (30-40%) and in African-American patients (who are more susceptible to the systemic form).[2]
In 1980 the American College of Rheumatology agreed upon diagnostic criteria for scleroderma.[11]
Diffuse scleroderma can cause musculoskeletal, pulmonary, gastrointestinal, renal and other complications.[1]Patients with larger amounts of cutaneous involvement are more likely to have involvement of the internal tissues and organs.
Skin Symptoms
- Scleroderma affects the skin, and in more serious cases it can affect the blood vessels and internal organs. The most evident symptom is the hardening of the skin and associated scarring. Typically, the skin appears reddish or scaly. Blood vessels may also be more visible. Where large areas are affected, fat and muscle wastage will weaken limbs and affect appearance.
- The seriousness of the disease varies hugely between cases. The two most important factors to consider are the level of internal involvement (beneath the skin) and the total area covered by the disease. For example, there have been cases where the patient has no more than one or two lesions, perhaps covering a few inches. Less serious cases tend not to involve the internal bodily functions.
- There is discoloration of the hands and feet in response to cold. Most patients (over 80%) have Raynaud's phenomenon, a vascular symptom that can affect the fingers and toes.
- Systemic scleroderma and Raynaud's phenomenon can cause painful ulcers on the fingers or toes which are known as digital ulcers.
- Calcinosis is also common in systemic scleroderma, and is often seen near the elbows, knees or other joints.
Musculoskeletal System Related Symptoms
The first joint symptoms that patients with scleroderma have are typically non specific joint pains, which can lead to arthritis, or cause discomfort in tendons or muscles.[1] Joint mobility, especially of the small joints of the hand, may be restricted by calcinosis or skin thickening.[12] Patients who have progressed later in their disease may develop muscle weakness, or myopathy, either from the disease, or its treatments.[13]
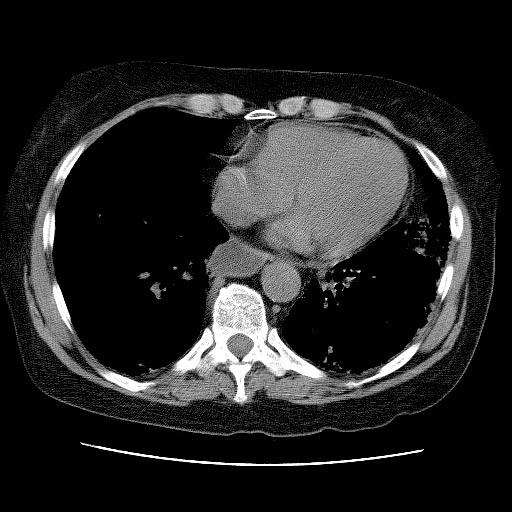
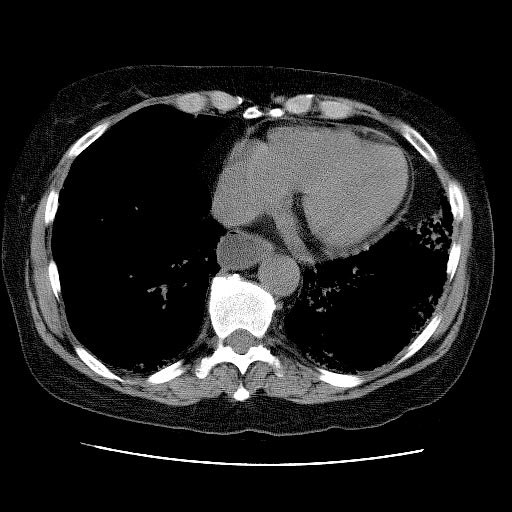
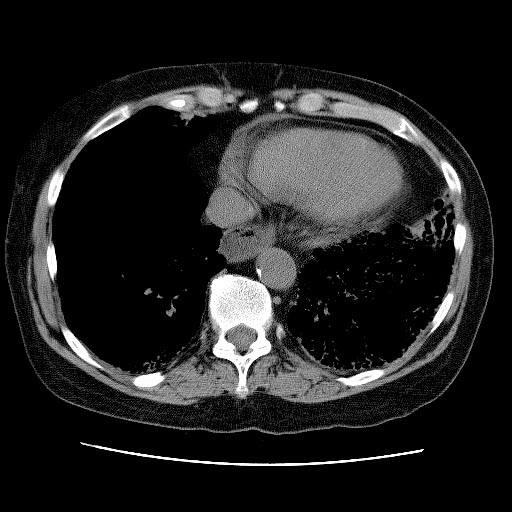
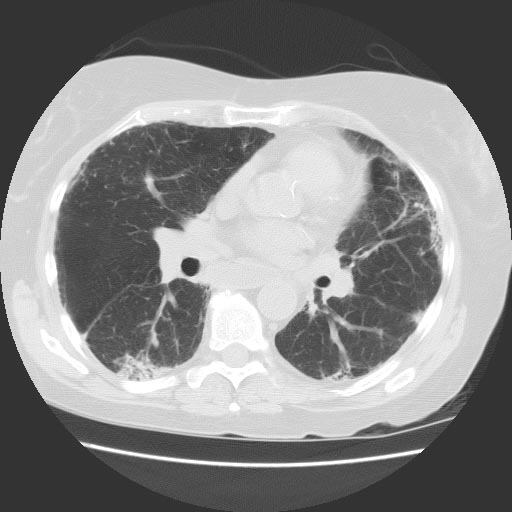
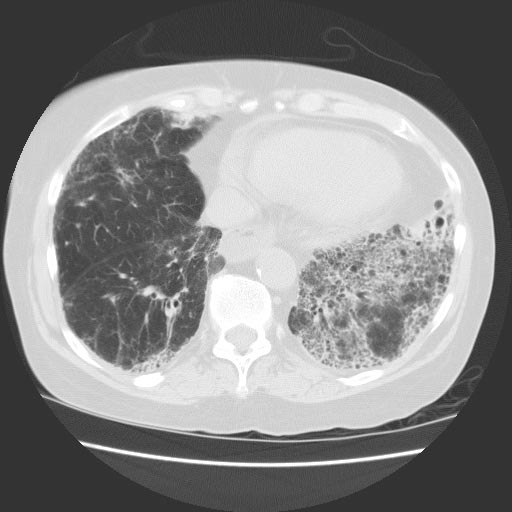
Images shown below are courtesy of RadsWiki and copylefted
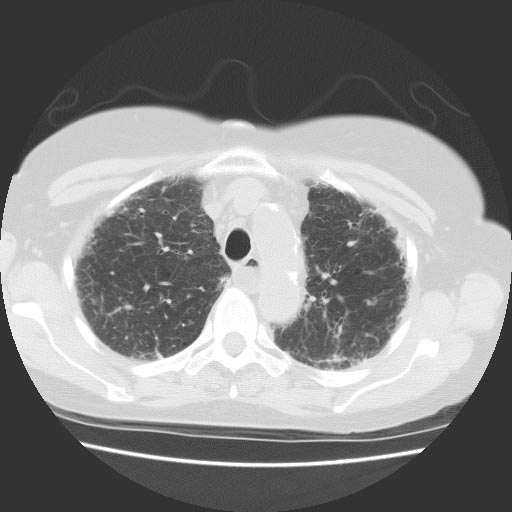
Respiratory System Symptoms
Some impairment in lung function is almost universally seen in patients with diffuse scleroderma on pulmonary function testing;[14] however, it does not necessarily cause symptoms, such as shortness of breath. Some patients can develop pulmonary hypertension, or elevation in the pressures of the pulmonary arteries. This can be progressive, and lead to right sided heart failure. The earliest manifestation of this may be a decreased diffusion capacity on pulmonary function testing.
Other pulmonary complications in more advanced disease include aspiration pneumonia, pulmonary hemorrhage and pneumothorax.[1]
Images shown below are courtesy of RadsWiki and copylefted
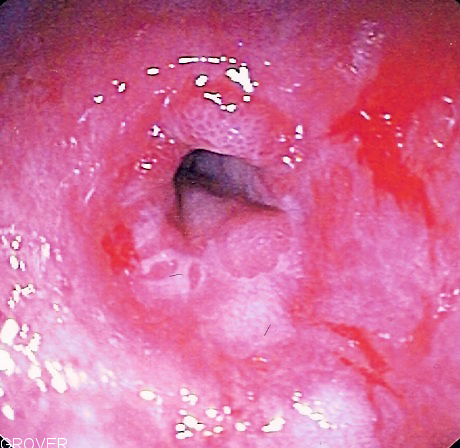
Gastrointestinal System Related Symptoms
Diffuse scleroderma can affect any part of the gastrointestinal tract.[15] The most common manifestation in the esophagus is reflux esophagitis, which may be complicated by peptic stricturing, or benign narrowing of the esophagus.[16] This is best initially treated with proton pump inhibitors for acid suppression,[17] but may require bougie dilatation in the case of stricture.[15]
Scleroderma can decrease motility anywhere in the gastrointestinal tract.[15] The most common source of decreased motility involvement is the esophagus and the lower esophageal sphincter, leading to dysphagia and chest pain. As Scleroderma progresses, esophageal involvement from abnormalities in decreased motility may worsen due to progressive fibrosis (scarring). If this is left untreated, acid from the stomach can back up into the esophagus causing esophagitis, and GERD. Further scarring from acid damage to the lower esophagus many times leads to the development of fibrotic narrowing, also known as strictures which can be treated by dilatation, and Barrett's esophagus. The small intestine can also become involved, leading to bacterial overgrowth and malabsorption, of bile salts, fats, carbohydrates, proteins, and vitamins. The colon can be involved, and can cause pseudo-obstruction or ischemic colitis.[1]
Rarer complications include pneumatosis cystoides intestinalis, or gas pockets in the bowel wall, wide mouthed diverticula in the colon and esophagus, and liver fibrosis. Patients with severe gastrointestinal involvement can become profoundly malnourished.[16]
Scleroderma may also be associated with gastric antral vascular ectasia (GAVE), also known as watermelon stomach. This is a condition where atypical blood vessels proliferate usually in a radially symmetric pattern around the pylorus of the stomach. GAVE can be a cause of upper gastrointestinal bleeding or iron deficiency anemia in patients with scleroderma.[16]
-
Endoscopic image of peptic stricture, or narrowing of the esophagus near the junction with the stomach due to chronic gastroesophageal reflux. This is the most common cause of dysphagia, or difficulty swallowing, in scleroderma.
-
Barium graphy: Lower esophageal sphincter involvement. (Image courtesy of RadsWiki and copylefted)
-
Barium graphy: Small intestine and colon involvements. (Image courtesy of RadsWiki and copylefted)
Renal Symptoms
Renal involvement, in scleroderma, is considered a poor prognostic factor and not infrequently a cause of death in patients with scleroderma.[18]
The most important clinical complication of scleroderma involving the kidney is scleroderma renal crisis. Symptoms of scleroderma renal crisis are malignant hypertension (high blood pressure with evidence of acute organ damage), hyperreninemia (high renin levels), azotemia (kidney failure with accumulation of waste products in the blood) and microangiopathic hemolytic anemia (destruction of red blood cells).[19] Apart from the high blood pressure, hematuria (blood in the urine) and proteinuria (protein loss in the urine) may be indicative.[20]
In the past scleroderma renal crisis was almost uniformily fatal.[21] While outcomes have improved significantly with the use of ACE inhibitors[22][23] the prognosis is often guarded, as a significant number of patients are refractory to treatment and develop renal failure. Approximately 10% of all scleroderma patients develop renal crisis at some point in the course of their disease.[24] Patients that have rapid skin involvement have the highest risk of renal complications.[24]
Therapy
There is no cure for every patient with scleroderma, though there is treatment for some of the symptoms, including drugs that soften the skin and reduce inflammation. Some patients may benefit from exposure to heat.[25]
A range of NSAIDs (nonsteroidal anti-inflammatory drugs) can be used to ease symptoms, such as naproxen. If there is esophageal dysmotility (in CREST or systemic sclerosis), care must be taken with NSAIDs as they are gastric irritants, and so a proton pump inhibitor (PPI) such as omeprazole can be given in conjunction.
Immunosuppressant drugs, such as mycophenolate mofetil (Cellcept®) or cyclophosphamide are sometimes used to slow the progress. Digital ulcerations and pulmonary hypertension can be helped by prostacyclin (iloprost) infusion. Iloprost being a drug which increases blood flow by relaxing the arterial wall.[26]
Treatments for scleroderma renal crisis include ACE inhibitors, which are also used for prophylaxis,[24][23] and renal transplantation. Transplanted kidneys are known to be affected by scleroderma and patients with early onset renal disease (within one year of the scleroderma diagnosis) are thought to have the highest risk for recurrence.[27]
While still experimental (given its high rate of complications), hematopoietic stem cell transplantation is being studied in patients with severe systemic sclerosis; improvement in life expectancy and severity of skin changes has been noted.[28]
Case Examples
Clinical Summary
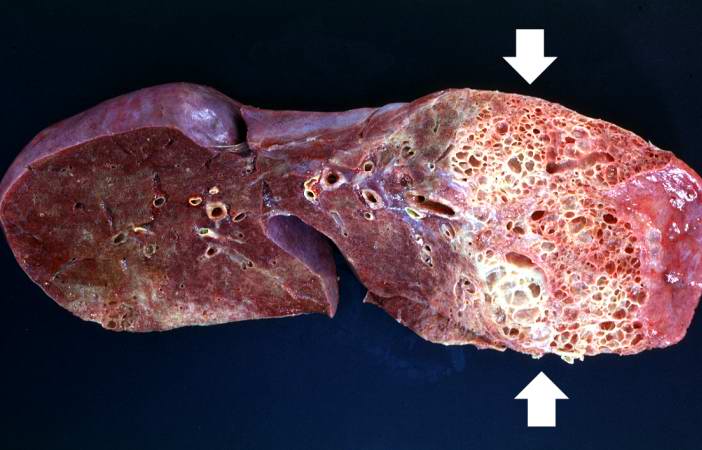
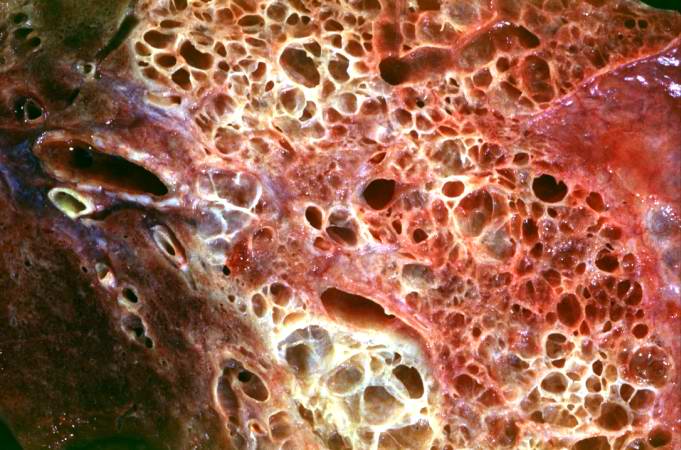
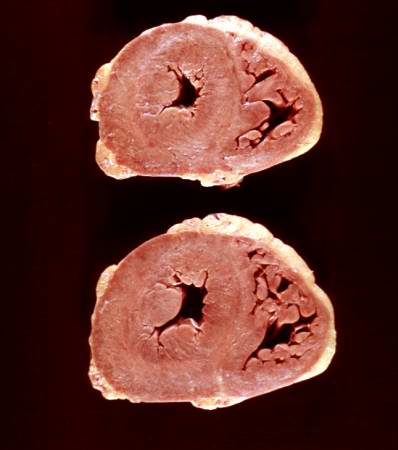
A 29-year-old black female had a history of scleroderma involving the lung, kidney, heart, and skin. Her main clinical problems centered on her restrictive lung disease. She was able to live at home with supplemental oxygen but recently she had developed edema, chest pain, weakness, light-headedness, and a loss of appetite. The patient was admitted to the hospital with a working diagnosis of congestive heart failure brought on by her lung disease. Echocardiographic evaluation revealed a pericardial effusion that was tapped. Soon after this procedure her respiratory status degenerated and she required intubation. Despite aggressive supportive treatment for her cardiac and pulmonary problems, she could not be weaned from the ventilator. Two weeks after admission she became febrile and Gram positive cocci were isolated from sputum culture. She was placed on antibiotics but her condition deteriorated and she developed bradycardia followed by electromechanical dissociation (EMD).
Autopsy Findings
Upon opening the thorax there was 600 cc of cloudy serous fluid in each hemithorax and 100 cc of similar fluid in the pericardial sac. The heart weighed 530 grams and there was thickening of both the left and right ventricular walls. The liver weighed 1880 grams and was congested. The spleen weighed 200 grams and was also congested. The combined lung weight was 1875 grams; the lungs were markedly fibrotic with severe emphysema. In addition, dermal thickening was evident throughout the body and the wall of the esophagus was thickened and firm.
Histopathological Findings


References
- ↑ 1.0 1.1 1.2 1.3 1.4 Klippel J (ed). Systemic sclerosis and related syndromes. Primer on the rheumatic diseases, 11th edition. The Arthritis Society. 1997;269. ISBN 1-91242-316-2.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Jimenez SA, Derk CT (2004). "Following the molecular pathways toward an understanding of the pathogenesis of systemic sclerosis". Ann. Intern. Med. 140 (1): 37–50. PMID 14706971.
- ↑ Bianchi DW (2000). "Fetomaternal cell trafficking: a new cause of disease?". Am. J. Med. Genet. 91 (1): 22–8. PMID 10751084.
- ↑ Galan A, Cowper SE, Bucala R (2006). "Nephrogenic systemic fibrosis (nephrogenic fibrosing dermopathy)". Current opinion in rheumatology. 18 (6): 614–7. doi:10.1097/01.bor.0000245725.94887.8d. PMID 17053507.
- ↑ Boyd AS, Zic JA, Abraham JL (2007). "Gadolinium deposition in nephrogenic fibrosing dermopathy". J. Am. Acad. Dermatol. 56 (1): 27–30. doi:10.1016/j.jaad.2006.10.048. PMID 17109993.
- ↑ Sharma SK, Handa R, Sood R; et al. (2004). "Bleomycin-induced scleroderma". The Journal of the Association of Physicians of India. 52: 76–7. PMID 15633728.
- ↑ Farrant PB, Mortimer PS, Gore M (2004). "Scleroderma and the taxanes. Is there really a link?". Clin. Exp. Dermatol. 29 (4): 360–2. doi:10.1111/j.1365-2230.2004.01519.x. PMID 15245529.
- ↑ Kettaneh A, Al Moufti O, Tiev KP; et al. (2007). "Occupational exposure to solvents and gender-related risk of systemic sclerosis: a metaanalysis of case-control studies". J. Rheumatol. 34 (1): 97–103. PMID 17117485.
- ↑ Winterbauer RH (1964). "Multiple telangiectasia, Raynaud'S phenomenon, sclerodactyly, and subcutanious calcinosis: a syndrome mimicking hereditary hemorrhagic telangiectasia". Bulletin of the Johns Hopkins Hospital. 114: 361–83. PMID 14171636.
- ↑ Morpea CNN.com, (May 05, 2006).
- ↑ "Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee". Arthritis Rheum. 23 (5): 581–90. PMID 7378088. Text "year:1980 " ignored (help) Available online at "Criteria for the Classification of Systemic Sclerosis 1980". Text " accessdate:5 August 2007" ignored (help)
- ↑ Valentini G, Black C (2002). "Systemic sclerosis". Best practice & research. Clinical rheumatology. 16 (5): 807–16. PMID 12473275.
- ↑ Olsen NJ, King LE, Park JH (1996). "Muscle abnormalities in scleroderma". Rheum. Dis. Clin. North Am. 22 (4): 783–96. PMID 8923596.
- ↑ Steen VD (2005). "The lung in systemic sclerosis". Journal of clinical rheumatology. 11 (1): 40–6. PMID 16357695.
- ↑ 15.0 15.1 15.2 Sallam H, McNearney TA, Chen JD (2006). "Systematic review: pathophysiology and management of gastrointestinal dysmotility in systemic sclerosis (scleroderma)". Aliment. Pharmacol. Ther. 23 (6): 691–712. doi:10.1111/j.1365-2036.2006.02804.x. PMID 16556171.
- ↑ 16.0 16.1 16.2 Rose S, Young MA, Reynolds JC (1998). "Gastrointestinal manifestations of scleroderma". Gastroenterol. Clin. North Am. 27 (3): 563–94. PMID 9891698.
- ↑ Hendel L, Hage E, Hendel J, Stentoft P (1992). "Omeprazole in the long-term treatment of severe gastro-oesophageal reflux disease in patients with systemic sclerosis". Aliment. Pharmacol. Ther. 6 (5): 565–77. PMID 1420748.
- ↑ Ruangjutipopan S, Kasitanon N, Louthrenoo W, Sukitawut W, Wichainun R (2002). "Causes of death and poor survival prognostic factors in thai patients with systemic sclerosis". Journal of the Medical Association of Thailand. 85 (11): 1204–9. PMID 12546318.
- ↑ Steen VD, Mayes MD, Merkel PA (2003). "Assessment of kidney involvement". Clin. Exp. Rheumatol. 21 (3 Suppl 29): S29–31. PMID 12889219.
- ↑ Steen VD (1994). "Renal involvement in systemic sclerosis". Clin. Dermatol. 12 (2): 253–8. PMID 8076263.
- ↑ Steen VD (2003). "Scleroderma renal crisis". Rheum. Dis. Clin. North Am. 29 (2): 315–33. PMID 12841297.
- ↑ Rhew EY, Barr WG (2004). "Scleroderma renal crisis: new insights and developments". Current rheumatology reports. 6 (2): 129–36. PMID 15016343.
- ↑ 23.0 23.1 Steen VD, Medsger TA (2000). "Long-term outcomes of scleroderma renal crisis". Ann. Intern. Med. 133 (8): 600–3. PMID 11033587.
- ↑ 24.0 24.1 24.2 Jimenez S, Koenig AS. Scleroderma. eMedicine.com. Accessed: May 22, 2006.
- ↑ Oliver GF, Winkelmann RK (1989). "The current treatment of scleroderma". Drugs. 37 (1): 87–96. PMID 2651089.
- ↑ Zandman-Goddard G, Tweezer-Zaks N, Shoenfeld Y (2005). "New therapeutic strategies for systemic sclerosis--a critical analysis of the literature". Clin. Dev. Immunol. 12 (3): 165–73. PMID 16295521.
- ↑ Pham PT, Pham PC, Danovitch GM, Gritsch HA, Singer J, Wallace WD, Hayashi R, Wilkinson AH. Predictors and risk factors for recurrent scleroderma renal crisis in the kidney allograft: case report and review of the literature. Am J Transplant. 2005 Oct;5(10):2565-9. PMID 16162209.
- ↑ Nash RA, McSweeney PA, Crofford LJ; et al. (2007). "High-dose immunosuppressive therapy and autologous hematopoietic cell transplantation for severe systemic sclerosis: long-term follow-up of the U.S. multicenter pilot study". Blood. 110 (4): 1388–96. doi:10.1182/blood-2007-02-072389. PMID 17452515.
External links
- Goldminer: Scleroderma
- DermnetNZ: Systemic sclerosis
- Juvenile Scleroderma Network
- Juvenile Systemic Sclerosis
- Scleroderma Foundation
- Scleroderma Society of Ontario
- International Scleroderma Network
- The Scleroderma Research Foundation
- UK Scleroderma Society
- Scleroderma Information from Johns Hopkins University
Template:Diseases of the musculoskeletal system and connective tissue Template:SIB
de:Sklerodermie
it:Sclerodermia
he:סקלרודרמה
nl:Sclerodermie
sk:Sklerodermia
sv:Sklerodermi