Retinoblastoma differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
Retinoblastoma must be differentiated from other diseases that cause [[leukocoria]]. Differential diagnosis of leukocoria in children include: | Retinoblastoma must be differentiated from other diseases that cause [[leukocoria]]. Differential diagnosis of leukocoria in children include: | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | | | A01 | | | | | |A01=Leukocoria}} | {{familytree | | | | | | | | | | | | | A01 | | | | | |A01=[[Leukocoria]]}} | ||
{{familytree | | | | | | | | | | | | | |!| | | }} | {{familytree | | | | | | | | | | | | | |!| | | }} | ||
{{familytree | |,|-|-|-|-|-|v|-|-|-|-|-|+|-|-|-|-|-|v|-|-|-|-|-|.| | }} | {{familytree | |,|-|-|-|-|-|v|-|-|-|-|-|+|-|-|-|-|-|v|-|-|-|-|-|.| | }} | ||
| Line 14: | Line 14: | ||
{{familytree | D01 | | | | D02 | | | | D03 | | | | D04 | | | | D05 | |D01=[[Tumors]]|D02=[[Congenital malformations]]|D03=[[Vascular]] [[diseases]]|D04=[[Inflammatory]] [[diseases]]|D05=[[Trauma]]}} | {{familytree | D01 | | | | D02 | | | | D03 | | | | D04 | | | | D05 | |D01=[[Tumors]]|D02=[[Congenital malformations]]|D03=[[Vascular]] [[diseases]]|D04=[[Inflammatory]] [[diseases]]|D05=[[Trauma]]}} | ||
{{familytree | |!| | | | | |!| | | | | |!| | | | | |!| | | | | |!| | }} | {{familytree | |!| | | | | |!| | | | | |!| | | | | |!| | | | | |!| | }} | ||
{{familytree | E01 | | | | E02 | | | | E03 | | | | E04 | | | | E05 | |E01=[[Retinoblastoma]]<br>[[Medulloepithelioma]]<br>[[Leukemia]]<br>Combined retinal [[hamartoma]]<br>[[Astrocytic hamartoma]] (Bourneville’s tuberous sclerosis)|E02=[[Persistent fetal vasculature]] (PFV)<br>Posterior [[coloboma]]<br>Retinal fold<br>Myelinated nerve fibers<br>Morning glory syndrome<br>[[Retinal dysplasia]]<br>[[Norrie’s disease]]<br>Incontinentia pigmenti<br>[[Cataract]]|E03=[[Retinopathy of prematurity]] (ROP)<br>[[Coats’ disease]]<br>Familial exudative vitreoretinopathy (FEVR)|E04=Ocular toxocariasis<br>Congenital toxoplasmosis<br>Congenital cytomegalovirus retinitis<br>Herpes simplex retinitis<br>Other types of fetal iridochoroiditis<br>[[Endophthalmitis]]|E05=Intraocular [[foreign body]]<br>[[Vitreous hemorrhage]]<br>[[Retinal detachment]]}} | {{familytree | E01 | | | | E02 | | | | E03 | | | | E04 | | | | E05 | |E01=[[Retinoblastoma]]<br>[[Medulloepithelioma]]<br>[[Leukemia]]<br>Combined retinal [[hamartoma]]<br>[[Astrocytic hamartoma]] (Bourneville’s tuberous sclerosis)|E02=[[Persistent fetal vasculature]] (PFV)<br>Posterior [[coloboma]]<br>[[Retinal fold]]<br>Myelinated nerve fibers<br>Morning glory syndrome<br>[[Retinal dysplasia]]<br>[[Norrie’s disease]]<br>Incontinentia pigmenti<br>[[Cataract]]|E03=[[Retinopathy of prematurity]] (ROP)<br>[[Coats’ disease]]<br>Familial exudative vitreoretinopathy (FEVR)|E04=[[Ocular toxocariasis]]<br>[[Congenital toxoplasmosis]]<br>Congenital cytomegalovirus retinitis<br>Herpes simplex retinitis<br>Other types of fetal iridochoroiditis<br>[[Endophthalmitis]]|E05=Intraocular [[foreign body]]<br>[[Vitreous hemorrhage]]<br>[[Retinal detachment]]}} | ||
Differential diagnosis of leukocoria | Differential diagnosis of leukocoria | ||
Revision as of 15:05, 8 May 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Simrat Sarai, M.D. [2] Sahar Memar Montazerin, M.D.[3]
Overview
Retinoblastoma must be differentiated from other diseases that cause leukocoria such as congenital cataract, persistent fetal vasculature, Coats disease, coloboma of choroid or optic disc, toxocariasis, astrocytic hamartoma, retinopathy of prematurity, vitreous hemorrhage, uveitis, retinal dysplasia, and medulloepithelioma.[1]
Differential diagnosis
Retinoblastoma must be differentiated from other diseases that cause leukocoria. Differential diagnosis of leukocoria in children include:
Differential diagnosis of leukocoria
| Leukocoria | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tumors | Congenital malformations | Vascular diseases | Inflammatory diseases | Trauma | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Retinoblastoma Medulloepithelioma Leukemia Combined retinal hamartoma Astrocytic hamartoma (Bourneville’s tuberous sclerosis) | Persistent fetal vasculature (PFV) Posterior coloboma Retinal fold Myelinated nerve fibers Morning glory syndrome Retinal dysplasia Norrie’s disease Incontinentia pigmenti Cataract | Retinopathy of prematurity (ROP) Coats’ disease Familial exudative vitreoretinopathy (FEVR) | Ocular toxocariasis Congenital toxoplasmosis Congenital cytomegalovirus retinitis Herpes simplex retinitis Other types of fetal iridochoroiditis Endophthalmitis | Intraocular foreign body Vitreous hemorrhage Retinal detachment | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Disease/Condition | Clinical presentation | Demographics/History | Diagnosis | Other notes |
|---|---|---|---|---|
| Retinoblastoma[2][3] |
|
|
| |
| Coats'disease[4][5] |
|
|
|
|
| Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous)[5] |
|
|
|
|
| Astrocytic hamartoma[6] |
|
|
|
|
| Retinopathy of prematurity (ROP)[6] |
|
|
|
|
| Ocular toxocariasis [6] |
|
|
|
|
| Hereditary retinal syndrome |
|
|
|
Differentiating features of some common and less common differential diagnosis are:
| Disease/Condition | Age of presentation | Risk factors | Unilateral/bilateral | Differentiating Signs/Symptoms | Axial length | Imaging findings |
|---|---|---|---|---|---|---|
| Retinoblastoma |
|
|
|
|
|
|
| Congenital Cataract |
|
| ||||
| Coats disease (exudative retinitis or retinal telangiectasis) |
|
| ||||
| Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous) |
|
| ||||
| Retinopathy of prematurity (ROP) |
|
| ||||
| Ocular toxocariasis |
|
|
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Ocular cysticercosis |
|
|
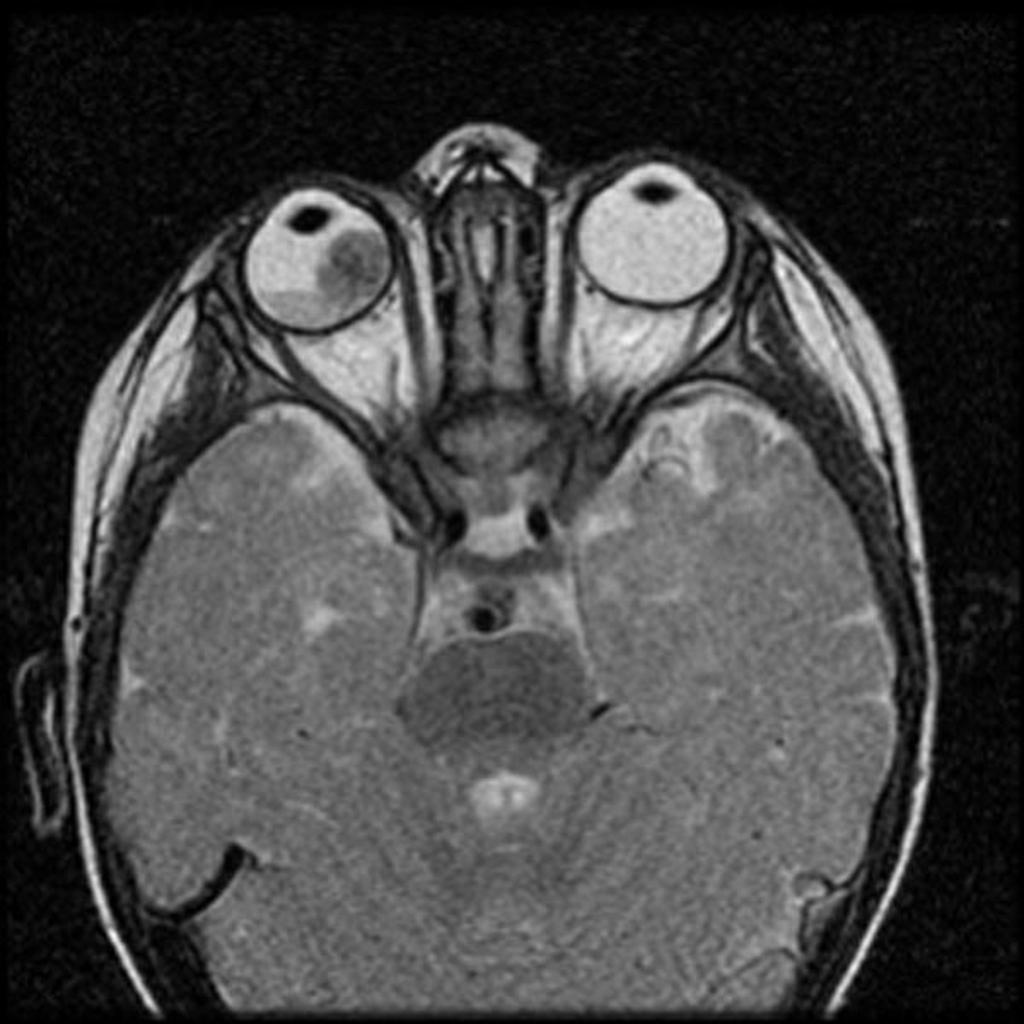
| Retinal detachment |
|
|
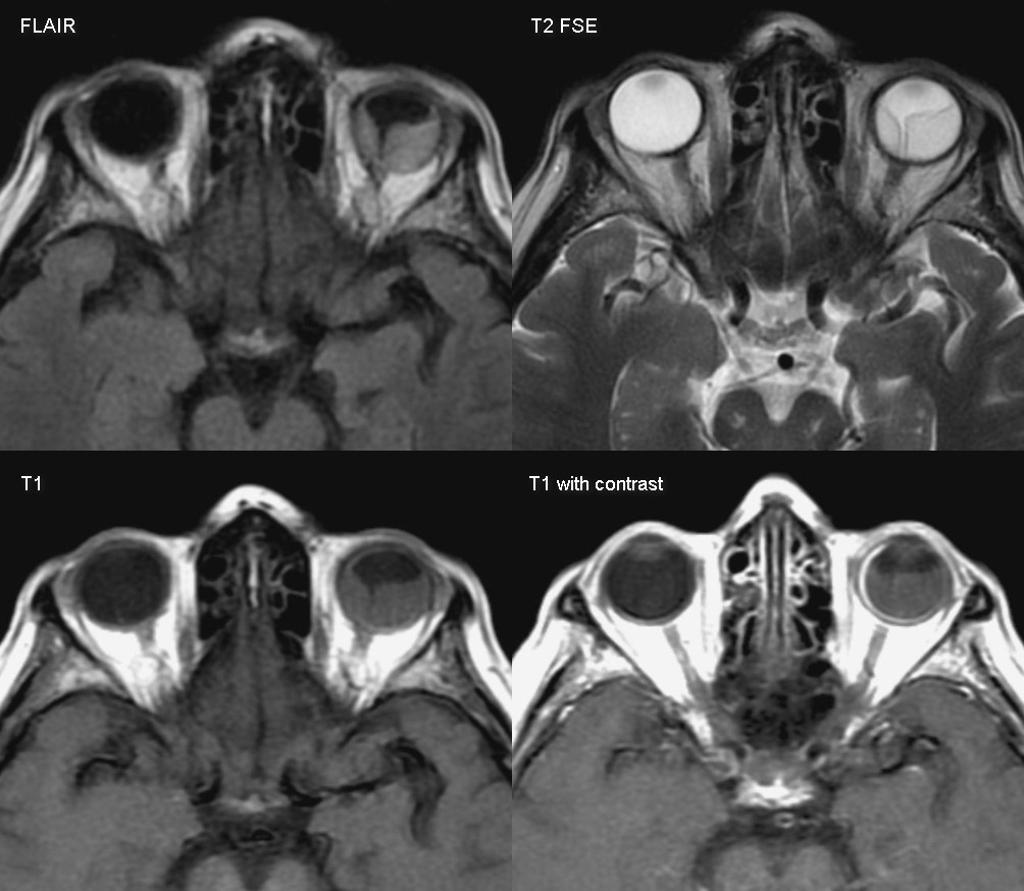
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
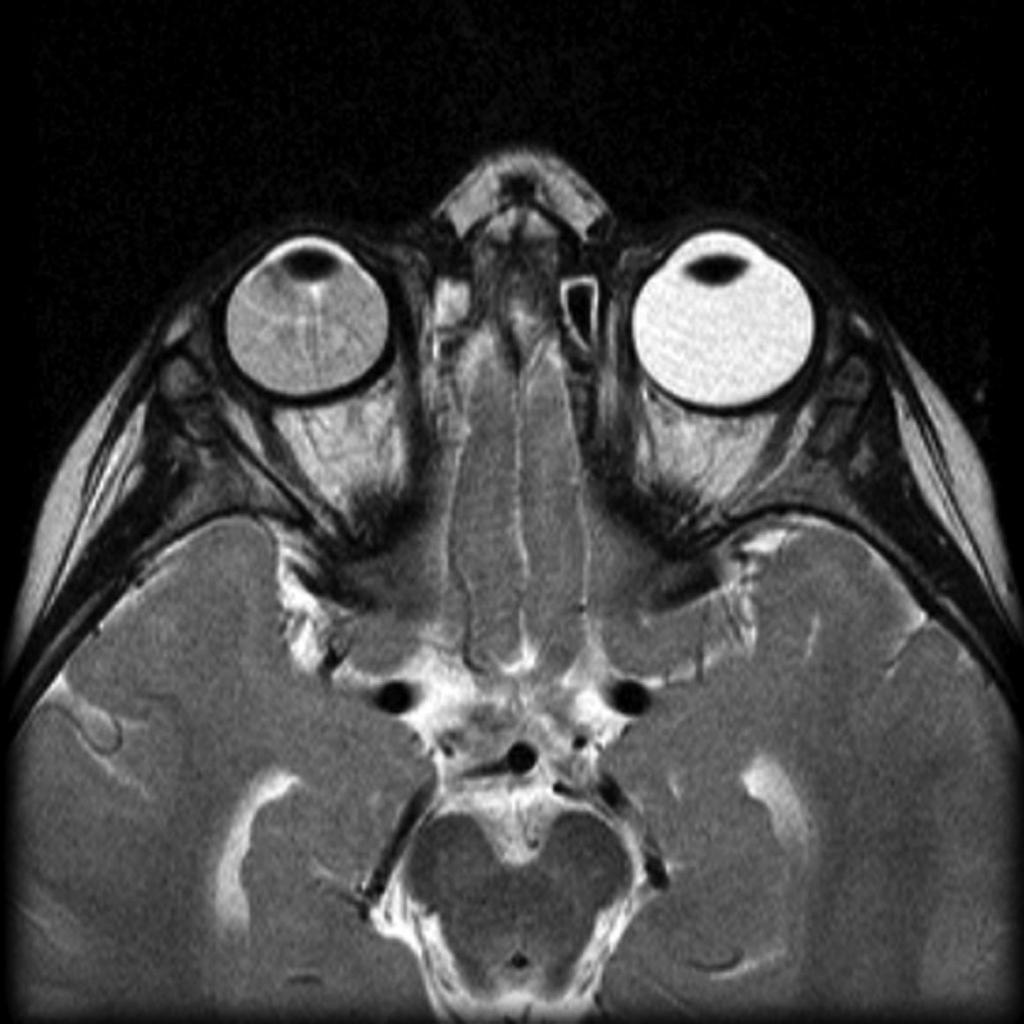 |
 |
 |
 |
|---|
References
- ↑ Retinoblastoma. Wikipedia(2015) https://en.wikipedia.org/wiki/Retinoblastoma#cite_note-30 Accessed on October 2, 2015
- ↑ Butros LJ, Abramson DH, Dunkel IJ (March 2002). "Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences". Pediatrics. 109 (3): E45. PMID 11875173.
- ↑ Sachdeva R, Schoenfield L, Marcotty A, Singh AD (June 2011). "Retinoblastoma with autoinfarction presenting as orbital cellulitis". J AAPOS. 15 (3): 302–4. doi:10.1016/j.jaapos.2011.02.013. PMID 21680213.
- ↑ Silva RA, Dubovy SR, Fernandes CE, Hess DJ, Murray TG (December 2011). "Retinoblastoma with Coats' response". Ophthalmic Surg Lasers Imaging. 42 Online: e139–43. doi:10.3928/15428877-20111208-04. PMID 22165951.
- ↑ 5.0 5.1 Gupta N, Beri S, D'souza P (June 2009). "Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease". J Pediatr Ophthalmol Strabismus. doi:10.3928/01913913-20090616-04. PMID 19645389.
- ↑ 6.0 6.1 6.2 Singh, Arun (2015). Clinical ophthalmic oncology : retinoblastoma. Heidelberg: Springer. ISBN 978-3-662-43451-2.
- ↑ 7.0 7.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 8.0 8.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 9.0 9.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 10.0 10.1 "c.ymcdn.com".