Retinoblastoma differential diagnosis: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
Ahmed Younes (talk | contribs) |
||
| Line 68: | Line 68: | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Fundus examination reveals the characteristic signs | *Fundus examination reveals the characteristic signs | ||
|} | |||
{| class="wikitable" | |||
|+Differentiating ocular cysticercosis from other ocular lesions | |||
!Disease | |||
!Prominent clinical feature | |||
!Radiological findings | |||
|- | |||
|Ocular cysticercosis | |||
| | |||
* Diagnosis made usually between 8-16 years (rarely in adulthood) | |||
* Wide range of symptoms from being [[asymptomatic]] to [[Decreased visual acuity|decreased vision]] and [[strabismus]]. | |||
* [[Decreased visual acuity]] at initial presentation has a poor prognosis. <ref name="urlHow to Diagnose and Manage Coats’ Disease">{{cite web |url=https://www.reviewofophthalmology.com/article/how-to-diagnose-and-manage-coatsand8217-disease-42782 |title=How to Diagnose and Manage Coats’ Disease |format= |work= |accessdate=}}</ref> | |||
| | |||
* [[Fundus (eye)|Fundus examination]] reveals vascular lesions and [[Exudate|exudates]]. | |||
* [[Fluorescein angiography]] is the best method to visualize the lesions. | |||
* [[CT]] and [[MRI]] are reserved for atypical cases.<ref name="urlHow to Diagnose and Manage Coats’ Disease">{{cite web |url=https://www.reviewofophthalmology.com/article/how-to-diagnose-and-manage-coatsand8217-disease-42782 |title=How to Diagnose and Manage Coats’ Disease |format= |work= |accessdate=}}</ref> | |||
|- | |||
|[[Retinal detachment]] | |||
| | |||
* Most common presenting symptoms are [[photophobia]] and [[floaters]] | |||
* [[Visual field defect|Visual field defects]] (described as curtain falling from periphery to the center)<ref name="urlManagement of retinal detachment: a guide for non-ophthalmologists">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2405853/ |title=Management of retinal detachment: a guide for non-ophthalmologists |format= |work= |accessdate=}}</ref> | |||
| | |||
* [[Ophthalmoscope]] is not reliable in detecting retinal detachment as there might be associated [[hemorrhage]] | |||
* [[Ultrasound]] can be used to identify and localize the detachment.<ref name="urlManagement of retinal detachment: a guide for non-ophthalmologists">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2405853/ |title=Management of retinal detachment: a guide for non-ophthalmologists |format= |work= |accessdate=}}</ref> | |||
|- | |||
|Hyperthyroid Ophthalmopathy | |||
| | |||
* The hallmark is [[Exophthalmos|Eye protrusion]], [[photophobia]], [[lacrimation]] and later in the disease, diminished eye motility.<ref name="urlThyroid Ophthalmopathy - EyeWiki">{{cite web |url=http://eyewiki.aao.org/Thyroid_Ophthalmopathy |title=Thyroid Ophthalmopathy - EyeWiki |format= |work= |accessdate=}}</ref> | |||
| | |||
* [[Ultrasonography]]: inflamed thickened [[extraocular muscles]]. | |||
* [[CT]]: shows [[inflamed]] muscle and free tendon from [[inflammation]] | |||
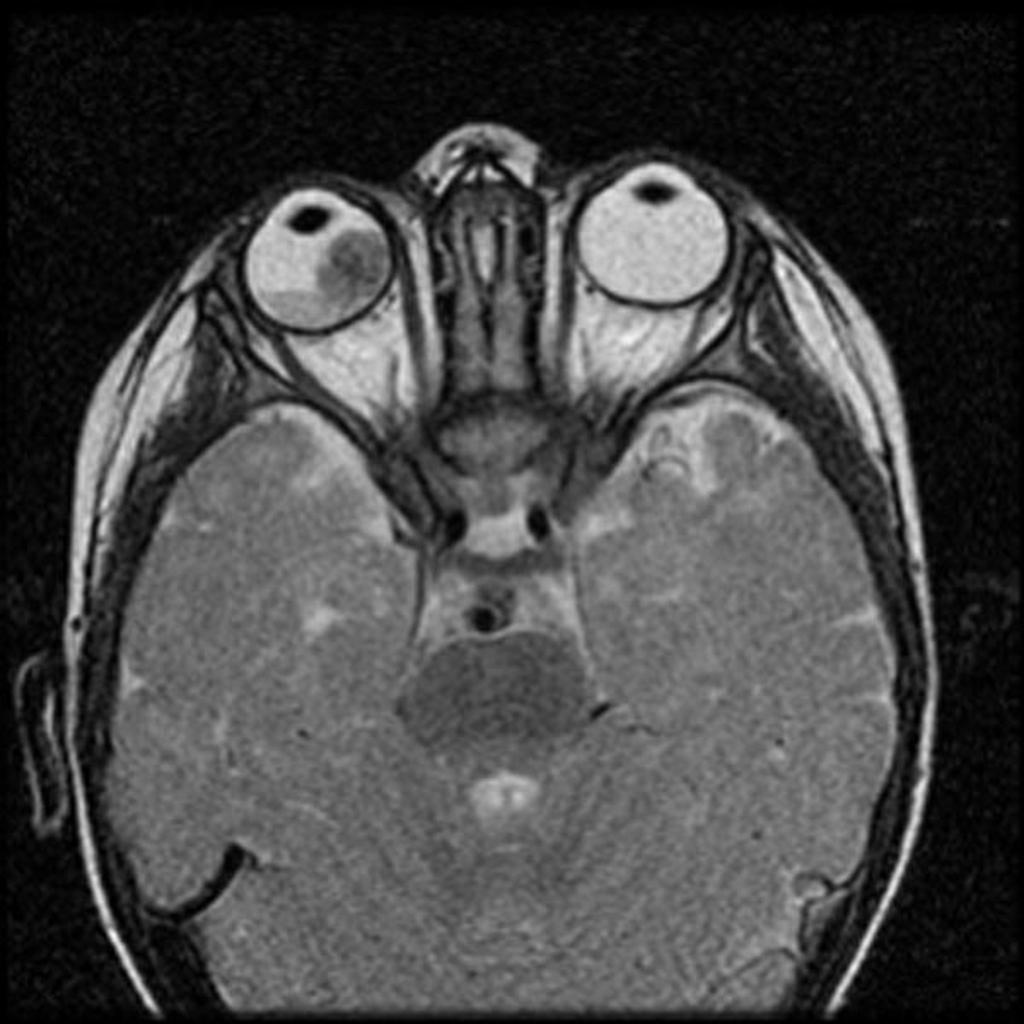
* [[MRI]]: shows periorbital fat expansion, increased water content of the muscles as a result of the [[inflammation]].<ref name="urlThyroid Ophthalmopathy - EyeWiki">{{cite web |url=http://eyewiki.aao.org/Thyroid_Ophthalmopathy |title=Thyroid Ophthalmopathy - EyeWiki |format= |work= |accessdate=}}</ref> | |||
|- | |||
|[[Retinoblastoma]] | |||
| | |||
* The most prominent sign is [[leukocoria]], followed by [[strabismus]] | |||
* The patient also may present with [[buphthalmos]], [[Cloudy cornea (patient information)|corneal clouding]] and eye tearing.<ref name="urlc.ymcdn.com">{{cite web |url=https://c.ymcdn.com/sites/www.covd.org/resource/resmgr/VDR_1-1/VDR1-1_article_Kollodge_Web.pdf+ |title=c.ymcdn.com |format= |work= |accessdate=}}</ref> | |||
| | |||
* [[Ultrasound]]: can detect the [[tumor]] as a result of the [[Calcification|calcifications]] inside. | |||
* [[MRI|MRI:]] assess [[Sella turcica|sellar]] and [[Parasellar and suprasellar disorders|parasellar]] regions .. it can also detect extraocular spread of the [[tumor]].<ref name="urlc.ymcdn.com">{{cite web |url=https://c.ymcdn.com/sites/www.covd.org/resource/resmgr/VDR_1-1/VDR1-1_article_Kollodge_Web.pdf+ |title=c.ymcdn.com |format= |work= |accessdate=}}</ref> | |||
|} | |||
{| class="wikitable" | |||
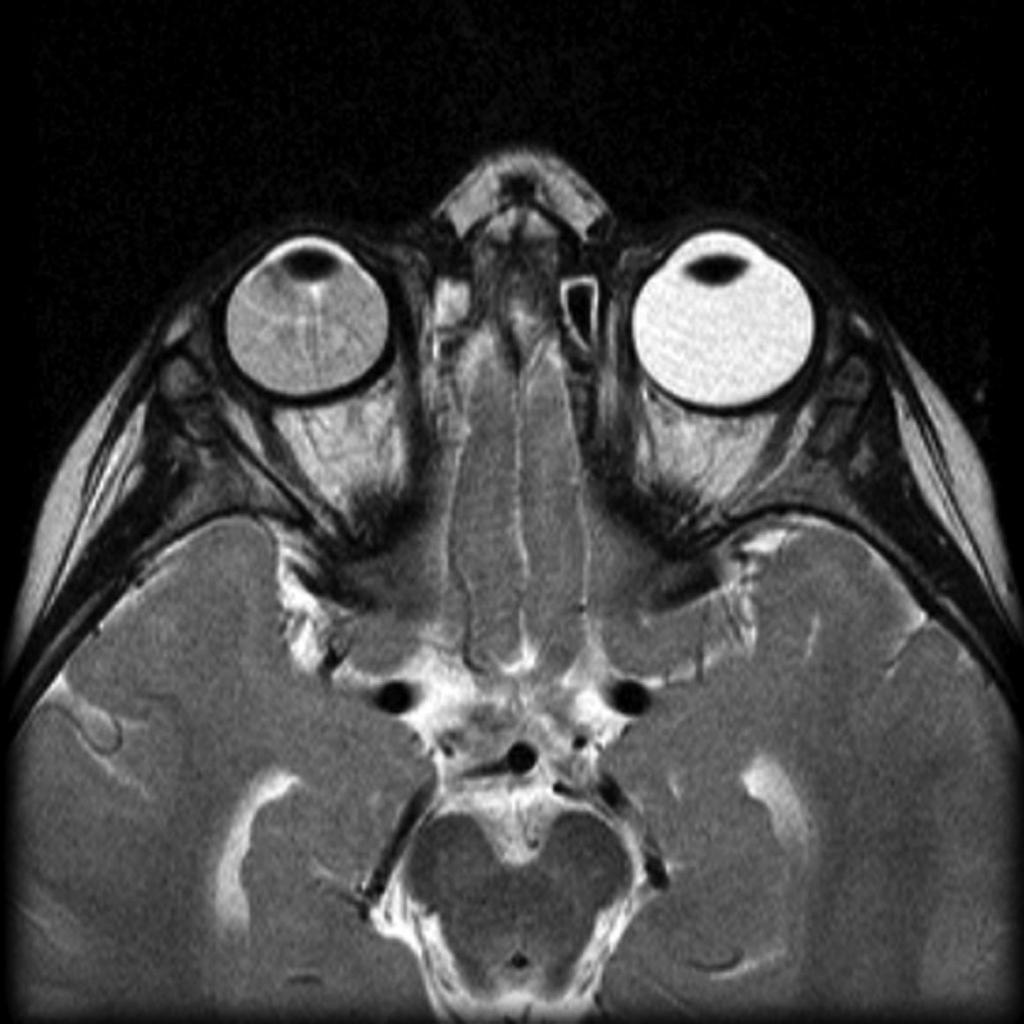
![[Image:Coats-disease-of-the-eye.jpg|center|300px|thumb|MRI of the orbit showing Coats disease - Case courtesy of Dr Michael Sargent, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/6089]] | |||
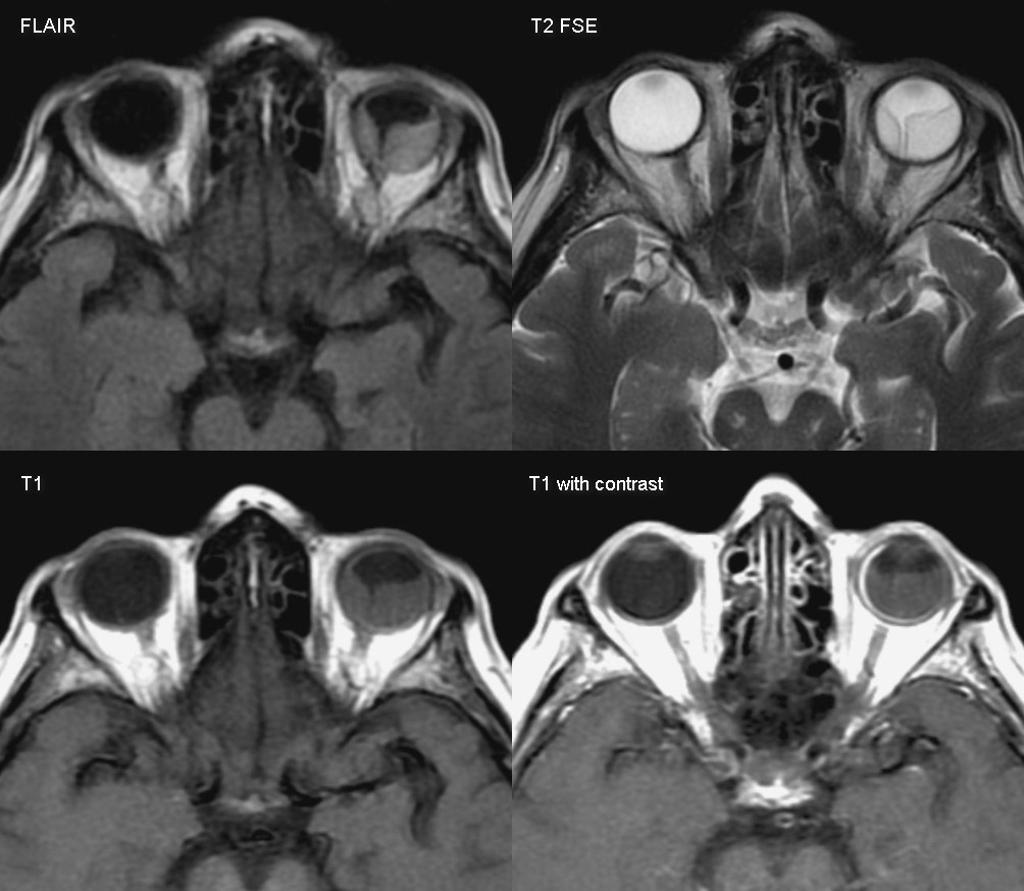
![[Image:Retinal-detachment-1.jpg|center|300px|thumb|MRI of the orbit showing retinal detachment - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/3134]] | |||
![[Image:Retinoblastoma-3.jpg|center|300px|thumb|MRI of the orbit showing retinoblastoma - Case courtesy of https://radiopaedia.org/. From the case https://radiopaedia.org/cases/11877]] | |||
![[Image:Thyroid-orbitopathy-severe-2.jpg|center|300px|thumb|CT head showing hyperthyroid-induced orbitopathy - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/4854]] | |||
|} | |} | ||
Revision as of 20:50, 22 August 2017
|
Retinoblastoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Retinoblastoma differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Retinoblastoma differential diagnosis |
|
Risk calculators and risk factors for Retinoblastoma differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1],Associate Editor(s)-in-Chief: Simrat Sarai, M.D. [2]
Overview
Retinoblastoma must be differentiated from other diseases that cause leukocoria such as congenital cataract, persistent fetal vasculature, Coats disease, coloboma of choroid or optic disc, toxocariasis, astrocytic hamartoma, retinopathy of prematurity, vitreous hemorrhage, uveitis, retinal dysplasia, and medulloepithelioma.[1]
Differential diagnosis
Retinoblastoma must be differentiated from other diseases that cause leukocoria. The common causes of leukocoria in children include:[1]
- Congenital cataract
- Persistent fetal vasculature
- Coats disease
Less common causes of leukocoria include:
- Coloboma of choroid or optic disc
- Toxocariasis
- Astrocytic hamartoma
- Retinopathy of prematurity (stage 4, 5)
- Vitreous hemorrhage
- Uveitis
- Retinal dysplasia
- Medulloepithelioma
Differentiating features of some common and less common differential diagnosis are:
| Disease/Condition | Differentiating Signs/Symptoms | Differentiating Tests |
|---|---|---|
| Congenital Cataract |
|
|
| Coats disease (exudative retinitis or retinal telangiectasis) |
|
|
| Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous) |
|
|
| Retinopathy of prematurity (ROP) |
|
|
| Ocular toxocariasis |
|
|
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Ocular cysticercosis |
|
|
| Retinal detachment |
|
|
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
 |
 |
 |
 |
|---|
References
- ↑ 1.0 1.1 Retinoblastoma. Wikipedia(2015) https://en.wikipedia.org/wiki/Retinoblastoma#cite_note-30 Accessed on October 2, 2015
- ↑ 2.0 2.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 3.0 3.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 4.0 4.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 5.0 5.1 "c.ymcdn.com".