Rapidly progressive glomerulonephritis pathophysiology
|
Rapidly progressive glomerulonephritis Microchapters |
|
Differentiating Rapidly progressive glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Rapidly progressive glomerulonephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Rapidly progressive glomerulonephritis pathophysiology |
|
FDA on Rapidly progressive glomerulonephritis pathophysiology |
|
CDC on Rapidly progressive glomerulonephritis pathophysiology |
|
Rapidly progressive glomerulonephritis pathophysiology in the news |
|
Blogs on Rapidly progressive glomerulonephritis pathophysiology |
|
Directions to Hospitals Treating Rapidly progressive glomerulonephritis |
|
Risk calculators and risk factors for Rapidly progressive glomerulonephritis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
Anatomy
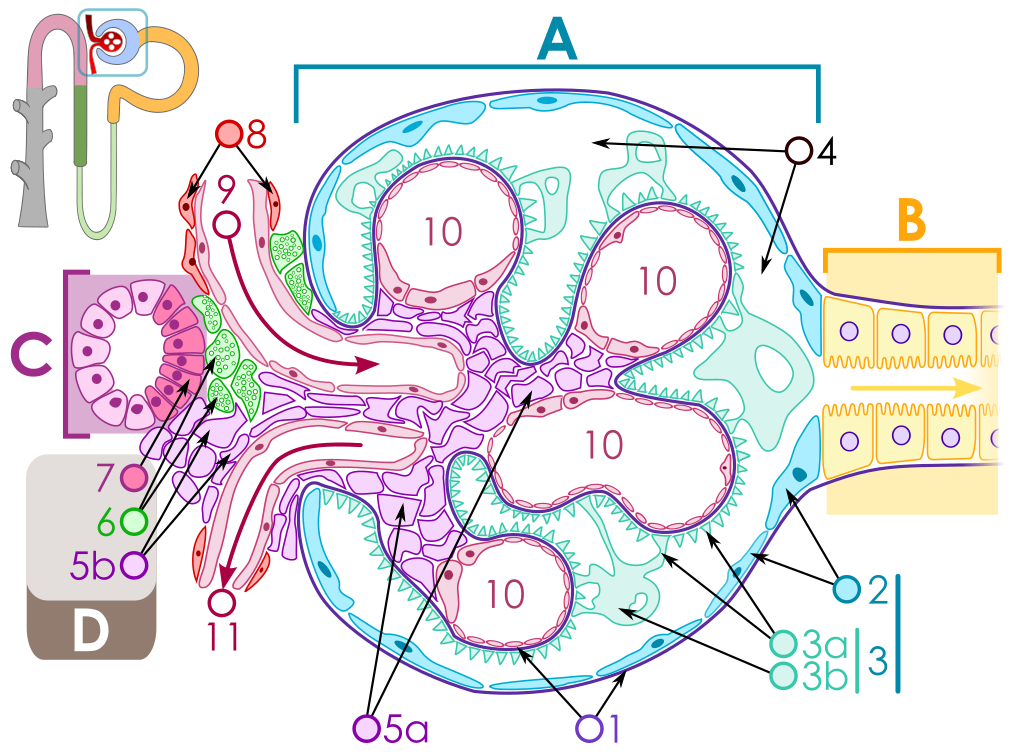
The key for the renal corpuscle figure is: A – Renal corpuscle, B – Proximal tubule, C – Distal convoluted tubule, D – Juxtaglomerular apparatus, 1. Basement membrane (Basal lamina), 2. Bowman's capsule – parietal layer, 3. Bowman's capsule – visceral layer, 3a. Pedicels (Foot processes from podocytes), 3b. Podocyte, 4. Bowman's space (urinary space), 5a. Mesangium – Intraglomerular cell, 5b. Mesangium – Extraglomerular cell, 6. Granular cells (Juxtaglomerular cells), 7. Macula densa, 8. Myocytes (smooth muscle), 9. Afferent arteriole, 10. Glomerulus Capillaries, 11. Efferent arteriole.
Rapidly progressive glomerulonephritis is a disease of the kidney in which the renal function deteriorates very quickly in a matter of days.
Atleast 50% reduction in GFR occurs in RPGN in a few days to weeks.
RPGN occurs from severe and fast damage to the GBM which results in crescent formation,the main pathological finding in RPGN.
Pathogenesis
- RPGN is characterized by severe and fast damage to the GBM that results in atleast 50% reduction in GFR in a few days.
- The injury to GBM can be caused by multiple factors.
- Crescent formation is the major pathological finding.
- In some cases crescents might be absent.
Cresent formation
- Crescents are defined as 2 or more layers of proliferating cells in the Bowman's space.
- The crescents are made up of epithelial cells and macrophages which undergo fibrosis.response t
- Crescents are formed after a severe injury to the glomerulus.in depos
- Injury to the glomerulus causes leakage of cells(epithelia, macrophages, coagulation proteins and fibroblasts) and cytokines(IL-12, TNF-alpha) into the Bowmans space.
- The presence of cytokines and coagulation proteins initiates fibrosis around the epithelial cells.
- The fibrosis blocks the glomerulus and filteration is hindered.
- This results in renal failure.
Glomerular injury
- Injury to the glomerulus is the initiating factor for crescent formation.
- Injury can occur by the following
- Anti GBM antibodies-Type I RPGN
- These are autoantibodies that cross react with type IV collagen of the GBM.
- These can be produced due to genetic causes such as in Goodpasture diseases or they can be produced after viral URTI or cigarette smoking.
- These autoantibodies react with the GBM resulting in IgG deposition over the GBM.
- The IgG activates helper T cells that attract the inflammatory mediators to the GBM damaging the glomeruli.
- This damage causes leakage of cells and inflammatory mediators resulting in crescent formation.
- The anti GBM antibodies can affect the lungs as well as in Goodpasture syndrome resulting in glomerular necrosis and pulmonary haemorrhages.
- Anti GBM antibodies-Type I RPGN
2. Immune complex- Type II RPGN
- Immune complexes are formed in certain infections, connective tissue diseases, side effects of some drugs and in some myeloproliferative disorders.
- These immune complexes are deposited over the GBM.
- The immune complexes activate the complement system which sets off the inflammatory process.
- The complement cascade is activated, attracting inflammatory cells and mediators to the GBM.
- The serum levels of c3 and c4 fall down and is an indicator of immune complex mediated glomerular injury.
- This damages the glomeruli and causes leakage of cells and inflammatory mediators resulting in crescent formation.
- Examples include:
- Postinfectious (staphylococci/streptococci)
- Connective tissue disorders
- Lupus nephritis
- Henoch-Schönlein purpural)
- Immunoglobulin A nephropathy
- Mixed cryoglobulinemia
- Membranoproliferative glomerulonephritis
3. Pauci immune RPGN-Type III RPGN
- No circulating immune complexes or antibodies.
- Glomerular damage is caused by circulating ANCAs(anti nuclear cytoplasmic antibodies) or it can be idiopathic(non ANCA).
- ANCAs cause glomerular damage by releasing lytic enzymes from white blood cells such as neutrophils.
- These lytic enzymes damage the GBM and cause leakage of circulating cells and initiate crescent formationin the Bowmans space.
- ANCAs are associated with systemic vasculitis.
- Examples include
- Granulomatosis with polyangiitis (Wegener granulomatosis)
- Microscopic polyangiitis (MPA)
- Renal-limited necrotizing crescentic glomerulonephritis (NCGN)
- Eosinophilic granulomatosis with polyangiitis (EGPA; Churg-Strauss syndrome)
- Drugs- hydralazine, allopurinol and rifampin.
Gross pathology
- The kidneys appear to be having having haemorrhages and necrosed tissue.
- Pulmonary haemorrhages may also be present in Goodpasture syndrome and type III RPGN.
- Type III RPGN may present with petechiae,rashes and purpuras.
Microscopic pathology
Histopathology
- Glomerular inflammation with signs of necrosis are present.
- .Glomerular caplillary wall rupture and damage to GBM.
- Crescents are present in the Bowmans space.
- Crescents are formed by proliferating epithelial cells and monocytes
- Fibroblasts migrate to the Bowman’s space and synthesize collagen.
- When cellular components are mixed with collagen the lesion is called fibroepithelial crescent.
- Renal vessels can show transmural vasculitis, with necrosis and lymphocyte infiltrates.
- Tubular necrosis may also be present.
- Interstitial granulomas in the glomeruli indicate Wegener’s granulomatosis.
Immunoflourescence
- In type I RPGN- diffuse and linear deposition of IgG along the GBM.
- In ttype II RPGN- diffuse and irregular deposition of IgG and C3 in the mesangial matrix.
- In type III RPGN- no finding.
Electron microscopy
- In type I and type III, no electron dense deposits are seen.
- In type II RPGN, subepithelial electron dense deposits indiacting the presence of immune complexes are seen.
Genetics
People with HLA DP1,DQ and DRB4 are more susceptible to develop RPGN.
{{#ev:youtube|CqSyj4cVZPE}}