Pharyngitis overview: Difference between revisions
(→Causes) |
No edit summary |
||
| (45 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Pharyngitis}} | {{Pharyngitis}} | ||
{{CMG}}; {{AE}}{{VSKP}} | {{CMG}}; {{AE}}{{VSKP}}{{DYM}} | ||
{{SK}} Sore throat; Group A streptococcal pharyngitis; Bacterial pharyngitis; Viral pharyngitis; Acute pharyngitis; Chronic pharyngitis | {{SK}} Sore throat; Group A streptococcal pharyngitis; Bacterial pharyngitis; Viral pharyngitis; Acute pharyngitis; Chronic pharyngitis | ||
==Overview== | ==Overview== | ||
A triad of [[sore throat]], [[fever]], and pharyngeal [[inflammation]] marked by [[erythema]] and [[edema]] are usually described as [[acute pharyngitis]], although [[exudates]], [[vesicles]], or [[ulcerations]] may also be present. The inflammation of the [[pharynx]], which presents as a [[sore throat]], is [[pharyngitis]]. It is a [[pain and nociception|painful]] inflammation of the [[pharynx]] and is colloquially referred to as a sore throat. [[Pharyngitis]] is a common medical problem in the outpatient medical setting, resulting in more than seven million [[pediatric]] visits each year. Most types of pharyngitis are caused by infectious etiologies. The most common cause of pharyngitis is a [[viral infection]]. However, some of the more serious types of [[pharyngitis]] are attributed to bacterial etiologies, such as [[Group A streptococcus|group A-hemolytic Streptococcus]] pyogenes ([[Group A beta-hemolytic streptococci|GAS]]). Complications from [[Group A streptococcal infection|GAS]] pharyngitis include [[rheumatic fever]], [[Abscesses|deep space abscesses]], and [[toxic shock]]. Although most episodes of [[pharyngitis]] are acute in nature, a small percentage becomes [[recurrent]] or chronic. With regards to [[chronic pharyngitis]], [[non-infectious]] etiologies, such as [[Laryngopharyngeal]] [[reflux disease]] and periodic [[fever]], [[aphthous ulcers]], pharyngitis, and [[Adenitis|adenitis syndrome]] also need to be considered. Both medical and surgical therapies are effective in managing pharyngitis. Antibiotic treatment requires first-line medical therapy. Surgical management via [[adenotonsillectomy]] is recommended for certain indications. [[Adenotonsillectomy]] has been shown to be effective in reducing the burden of disease and improving the global quality of life and disease-specific. Several procedures, including traditional and [[intracapsular]] [[tonsillectomies]], exist for [[adenotonsillectomy]]. | |||
== Historical Perspective == | == Historical Perspective == | ||
The sore throat was first described in the literature as 'some variants of sore throat' in the year 1879 by R. L. Bowles, M.D., in the British Medical Journal. Later, in 1885, David Newman, M.D., described [[pathology]], symptoms, and treatment of [[pharyngitis]].In 1910, the importance of [[bacteriological]] tests was shown in doubtful cases of pharyngitis. In 1931, three case reports were described and inferred that chronic [[non-tuberculous]] [[bronchial]] disease such as [[influenza]], [[whooping cough]], and [[measles]] is associated with chronic [[nasopharyngitis]] and also described the importance of conservative treatment in chronic nasopharyngitis. | |||
== Pathophysiology == | == Pathophysiology == | ||
The [[pathogenesis]] of the sore throat due to [[pharyngitis]] is poorly understood. | The [[pathogenesis]] of the sore throat due to [[pharyngitis]] is poorly understood. The [[pharynx]] is often the first site of infection for many [[contagious]] diseases such as pharyngitis because [[pathogens]] such as [[viruses]] and [[bacteria]] often settle in the [[nasopharynx]] though [[inhalation]] or through droplets. [[Viral pharyngitis]] usually transmit from person to person through direct touch or through droplets transmission. The foreign invader reproduces rapidly after settling on the [[nasopharynx]]. Generally [[pharyngitis]] is a primary disease, but may be associated with systemic disorders such as the [[Retroviral|acute retroviral syndrome]], or part of a more generalized [[upper respiratory tract infection]]. | ||
== Causes == | == Causes == | ||
[[Pharyngitis]] can be caused by infectious [[microorganisms]] or [[non-infectious]] agents. It is usually caused by [[viruses]] but may be caused by [[bacterial]] or [[fungal]] etiology. [[Gastroesophageal reflux disease]] (GERD) or particularly [[Esophageal reflux|extra esophageal reflux]] (EER) can also cause an acid pharyngitis in adults and children. | [[Pharyngitis]] can be caused by infectious [[microorganisms]] or [[non-infectious]] agents. It is usually caused by [[viruses]] but may be caused by [[bacterial]] or [[fungal]] etiology. [[Gastroesophageal reflux disease]] (GERD) or particularly [[Esophageal reflux|extra esophageal reflux]] (EER) can also cause an acid [[pharyngitis]] in adults and children. | ||
== Classification == | == Classification == | ||
Pharyngitis can be classified based on the duration as acute pharyngitis or chronic pharyngitis. | Pharyngitis can be classified based on the duration as [[acute pharyngitis]] or [[chronic pharyngitis]]. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
The major goal of the differentiating patients with sore throat or acute pharyngitis is to exclude potentially dangerous causes (e.g. [[Group A streptococcus]]), to identify any treatable causes, and to improve symptoms. Identifying the treatable causes is important because timely treatment with antibiotics helps prevent complications such as [[acute rheumatic fever]], [[post streptococcal glomerulonephritis]]. | The major goal of the differentiating patients with [[sore throat]] or [[acute pharyngitis]] is to exclude potentially dangerous causes (e.g. [[Group A streptococcus]]), to identify any treatable causes, and to improve symptoms. Identifying the treatable causes is important because timely treatment with antibiotics helps prevent complications such as [[acute rheumatic fever]], [[post streptococcal glomerulonephritis]]. Pharyngitis should be differentiated from other infectious causes which mimic sore throat that includes [[oral thrush]], [[infectious mononucleosis]], [[epiglottitis]] and [[peritonsillar abscess]]. | ||
== Epidemiology and Demographics == | == Epidemiology and Demographics == | ||
With more than 10 million outpatient visits per year, [[pharyngitis]] is one of the most common disorders in adults and children. [[Viruses]] are the single most common cause of [[pharyngitis]] and account for 25 percent to 45 percent of all cases. [[Group A streptococcus]] presents in up to 37% of all children presenting with a sore throat to an outpatient clinic or ED and 24% of those presenting at younger than 5 years. [[Group A streptococcus]] is by far the most common [[bacterial]] cause of [[acute pharyngitis]], accounting for approximately 15 to 30 percent of cases in children and 5 to 10 percent of cases in adults. Peak seasons for [[sore throat]] include late winter and early spring. | |||
== Risk Factors == | == Risk Factors == | ||
[[Pharyngitis]] is [[contagious]], so anyone in close proximity to someone with the [[illness]], is at risk. Social situations with prolonged close interpersonal contact are associated with a higher incidence of the disease, such as in schools, dormitories, or military barracks. Other common risk factors include History of ill contact, Overcrowding, Frequent sinus infections, Smoking, attending | [[Pharyngitis]] is [[contagious]], so anyone in close proximity to someone with the [[illness]], is at risk. Social situations with prolonged close interpersonal contact are associated with a higher incidence of the disease, such as in schools, dormitories, or military barracks. Other common risk factors include a History of ill contact, Overcrowding, Frequent sinus infections, Smoking, attending daycare, [[immunocompromised]] patients, etc. | ||
== Natural History, Complications & Prognosis == | == Natural History, Complications & Prognosis == | ||
Acute pharyngitis is typically described as the triad of sore throat, fever, and pharyngeal inflammation characterized by [[erythema]] and [[edema]], although [[Exudate|exudates]], [[vesicles]], or [[ulcerations]] may also be present. Although pharyngitis may be a primary disorder, sore throat and pharyngeal erythema may also be prominent in systemic disorders, such as the [[Human Immunodeficiency Virus (HIV)|acute retroviral syndrome]], or part of a more generalized [[upper respiratory tract infection]]. Most cases of acute pharyngitis are due to common viral infections and are benign, self-limited processes. The appropriate recognition of patients with more complicated infections that require diagnostic evaluations and treatment is one of the challenges of primary care medicine. | [[Acute pharyngitis]] is typically described as the triad of [[sore throat]], [[fever]], and pharyngeal [[inflammation]] characterized by [[erythema]] and [[edema]], although [[Exudate|exudates]], [[vesicles]], or [[ulcerations]] may also be present. Although [[pharyngitis]] may be a primary disorder, [[sore throat]] and pharyngeal [[erythema]] may also be prominent in systemic disorders, such as the [[Human Immunodeficiency Virus (HIV)|acute retroviral syndrome]], or part of a more generalized [[upper respiratory tract infection]]. Most cases of [[acute pharyngitis]] are due to common [[viral infections]] and are [[benign]], self-limited processes. The appropriate recognition of patients with more complicated infections that require diagnostic evaluations and treatment is one of the challenges of primary care medicine. An estimated 1-2% of [[acute pharyngitis]] progresses to recurrent or [[chronic disease]]. | ||
== Diagnosis== | == Diagnosis== | ||
'''Key points in the evaluation of acute pharyngitis''' | '''Key points in the evaluation of acute pharyngitis''' | ||
* Essential to diagnosis is the identification of treatable causes (e.g. [[Group A streptococcus]]) to prevent complications. | * Essential to diagnosis is the identification of treatable causes (e.g. [[Group A streptococcus]]) to prevent complications. | ||
* Signs and symptoms of [[Group A streptococcal infection|GAS]] pharyngitis include acute onset of sore throat with tonsillar or pharyngeal [[Exudate|exudates]], tender [[Lymphadenopathy|anterior cervical lymphadenopathy]] and [[fever]]. | * Signs and symptoms of [[Group A streptococcal infection|GAS]] pharyngitis include acute onset of sore throat with tonsillar or pharyngeal [[Exudate|exudates]], tender [[Lymphadenopathy|anterior cervical lymphadenopathy]] and [[fever]]. | ||
* Signs and symptoms consistent with viral etiologies include [[conjunctivitis]], coryza, oral ulcers, cough, and diarrhea. | * Signs and symptoms consistent with viral etiologies include [[conjunctivitis]], [[coryza]], oral ulcers, [[cough]], and [[diarrhea]]. | ||
* Testing for [[Group A streptococcal infection|GAS]] pharyngitis should not be pursued in those with signs and symptoms indicative of a viral etiology. | * Testing for [[Group A streptococcal infection|GAS]] pharyngitis should not be pursued in those with signs and symptoms indicative of a viral etiology. | ||
* Rapid antigen detection tests (RADTs) alone are sufficient for the diagnosis of [[Group A streptococcal infection|GAS]] in adults, but negative results should be backed up by throat culture in children. | * [[Rapid antigen]] detection tests ([[RADTs]]) alone are sufficient for the diagnosis of [[Group A streptococcal infection|GAS]] in adults, but negative results should be backed up by throat culture in children. | ||
* Specific techniques should be used to identify other causes where appropriate. | * Specific techniques should be used to identify other causes where appropriate. | ||
| Line 53: | Line 50: | ||
|- | |- | ||
! Screening for acute pharyngitis | ! Screening for acute pharyngitis | ||
| Use Centor criteria || Use clinical and epidemiologic findings to assess patient’s risk of [[Group A streptococcal infection|GABHS]] (e.g., sudden onset of sore throat, [[fever]], [[odynophagia]], [[Erythema|tonsillar erythema]], [[Exudate|exudates]], [[Lymphadenitis|cervical lymphadenitis]], or history of streptococcal exposure) | | Use Centor criteria || Use clinical and epidemiologic findings to assess patient’s risk of [[Group A streptococcal infection|GABHS]] (e.g., sudden onset of sore throat, [[fever]], [[odynophagia]], [[Erythema|tonsillar erythema]], [[Exudate|exudates]], [[Lymphadenitis|cervical lymphadenitis]], or history of [[streptococcal]] exposure) | ||
|- | |- | ||
! Diagnostic testing | ! Diagnostic testing | ||
| Line 59: | Line 56: | ||
|RADT or throat culture in all patients at risk | |RADT or throat culture in all patients at risk | ||
|- | |- | ||
! Back-up culture needed if RADT | ! Back-up culture needed if RADT results negative? | ||
|Adults: No | |Adults: No | ||
Children: Yes | Children: Yes | ||
| Line 76: | Line 73: | ||
|} | |} | ||
=== History and Symptoms === | === History and Symptoms === | ||
Pharyngitis is a very common inflammatory condition of the pharynx accompanied by a sore throat and occasionally difficulty in swallowing. | [[Pharyngitis]] is a very common inflammatory condition of the pharynx accompanied by a sore throat and occasionally difficulty in swallowing. Other symptoms depends on the etiology such as [[bacterial]] or [[viral]]. | ||
{| class="wikitable" | {| class="wikitable" | ||
! colspan="2" |Clinical features of acute pharyngitis | ! colspan="2" |Clinical features of acute pharyngitis | ||
| Line 88: | Line 85: | ||
* Fever | * Fever | ||
* Headache | * Headache | ||
* Nausea, vomiting, abdominal pain | * [[Nausea]], [[vomiting]], abdominal pain | ||
* Tonsillopharyngeal inflammation | * [[Tonsillopharyngeal]] inflammation | ||
* Patchy tonsillopharyngeal exudates | * Patchy [[tonsillopharyngeal]] exudates | ||
* Palatal petechiae | * Palatal [[petechiae] | ||
* Anterior cervical adenitis (tender nodes) | * Anterior cervical [[adenitis]] (tender nodes) | ||
* Winter and early spring presentation | * Winter and early spring presentation | ||
* History of exposure to strep pharyngitis | * History of exposure to strep pharyngitis | ||
* [[Scarlet fever|Scarlatiniform rash]] | * [[Scarlet fever|Scarlatiniform rash]] | ||
| valign = top | | | valign = top | | ||
* Conjunctivitis | * [[Conjunctivitis]] | ||
* Coryza | * [[Coryza]] | ||
* Cough | * [[Cough]] | ||
* Diarrhea | * [[Diarrhea]] | ||
* Hoarseness | * [[Hoarseness]] | ||
* Discrete ulcerative stomatitis | * Discrete [[ulcerative]] [[stomatitis]] | ||
* Viral exanthema | * [[Viral exanthema]] | ||
|} | |} | ||
=== Physical Examination === | === Physical Examination === | ||
Patients with pharyngitis typically have low-grade [[fever]] and pharyngeal erythema, suggestive of viral etiology or pharyngeal exudate or petechia, suggestive of [[Group A streptococcal infection|GAS]]. Additional signs include enlarged edematous tonsils, enlarged and/or tender cervical adenopathy, rash may or may not be present. [[Scarlet fever|Scarlatiniform rash]], which is marked by multiple small red papules that are widely and diffusely distributed but spare the | Patients with [[pharyngitis]] typically have low-grade [[fever]] and pharyngeal [[erythema]], suggestive of [[viral]] etiology or [[pharyngeal]] [[exudate]] or [[petechia]], suggestive of [[Group A streptococcal infection|GAS]]. Additional signs include enlarged [[edematous]] [[tonsils]], enlarged and/or [[tender]] [[cervical]] [[adenopathy]], the [[rash]] that may or may not be present. [[Scarlet fever|Scarlatiniform rash]], which is marked by multiple small red [[papules]] that are widely and diffusely distributed but spare the [[palms]] and [[soles]], is suggestive of [[Group A streptococcal infection|GAS]]. | ||
'''Centor criteria'''<br>The original Center score uses four signs and symptoms to estimate the probability of acute [[streptococcal]] [[pharyngitis]] in adults with a [[sore throat]] The score was later modified by adding age. It is important to evaluate for a definitive diagnosis to exclude [[Group A streptococcal infection|GAS]] and to avoid unnecessary lab tests and antibiotic use. Centor criteria are a widely used and accepted clinical decision tool in identifying patients for whom neither [[microbiologic]] tests nor [[antimicrobial]] therapy is necessary. The Center score to use for children and adults with a [[sore throat]] to estimate the probability of [[Streptococcus]] pyogenes infection. | |||
{| border="5" | {| border="5" | ||
| colspan="2" align="center" |'''Modified Centor criteria''' | | colspan="2" align="center" |'''Modified Centor criteria''' | ||
| Line 119: | Line 115: | ||
| align="center" |'''Points''' | | align="center" |'''Points''' | ||
|'''Total score''' | |'''Total score''' | ||
| align="center" |'''Chance of streptococcal infection in community''' | | align="center" |'''Chance of [[streptococcal]] infection in community''' | ||
'''with usual levels of infection, %''' | '''with usual levels of infection, %''' | ||
| align="center" |'''Suggested management''' | | align="center" |'''Suggested management''' | ||
| Line 129: | Line 125: | ||
| rowspan="2" |No culture or antibiotic is required | | rowspan="2" |No culture or antibiotic is required | ||
|- | |- | ||
| align="left" |Absence of cough | | align="left" |Absence of [[cough]] | ||
|align="center" | +1 | |align="center" | +1 | ||
|align="center" |1 | |align="center" |1 | ||
|align="center" |4-6% | |align="center" |4-6% | ||
|- | |- | ||
| align="left" |Swollen and tender anterior cervical nodes | | align="left" |[[Swollen]] and [[tender]] anterior [[cervical]] [[nodes]] | ||
|align="center" | +1 | |align="center" | +1 | ||
|align="center" |2 | |align="center" |2 | ||
|align="center" |10-12% | |align="center" |10-12% | ||
| rowspan="2" |RADT or Culture and treat only if culture result is positive | | rowspan="2" |[[RADT]] or Culture and treat only if culture result is positive | ||
|- | |- | ||
| align="left" |Tonsillar swelling or exudates | | align="left" |[[Tonsillar]] [[swelling]] or [[exudates]] | ||
|align="center" | +1 | |align="center" | +1 | ||
|align="center" |3 | |align="center" |3 | ||
| Line 160: | Line 156: | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
There is broad overlap between the signs and symptoms of streptococcal and non-streptococcal (usually viral) pharyngitis, and the ability to identify streptococcal pharyngitis accurately on the basis of clinical grounds alone is generally poor. | There is a broad overlap between the signs and symptoms of [[streptococcal]] and non-streptococcal (usually viral) [[pharyngitis]], and the ability to identify streptococcal pharyngitis accurately on the basis of clinical grounds alone is generally poor. Therefore, except when obvious viral clinical and epidemiological features are present, a laboratory test should be performed to determine whether [[Group A streptococcal infection|GAS]] is present in the pharynx. Even subjects with all clinical features in a particular scoring system can be confirmed to have streptococcal pharyngitis only about 35%–50% of the time and this is particularly the case in children. Swabbing the throat and testing for [[GAS]] pharyngitis with rapid antigen detection test ([[RADT]])&/ culture should be performed because the clinical features alone do not reliably discriminate between [[GAS]] and [[viral]] pharyngitis except when overt viral features like [[rhinorrhea]], [[cough]], oral [[ulcers]], and/or hoarseness are present. | ||
* The rapid streptococcal antigen tests are widely available and have been used and studied extensively as an adjunct to making the diagnosis of [[Group A streptococcal|GAS]] pharyngitis. Specificity for the test has been reported to be as high as 95%, with a sensitivity of 80% to 90%. Throat cultures are much more sensitive, between 90% and 95%. However, they require up to 48 hours for results. | * The rapid streptococcal antigen tests are widely available and have been used and studied extensively as an adjunct to making the diagnosis of [[Group A streptococcal|GAS]] pharyngitis. [[Specificity]] for the test has been reported to be as high as 95%, with a [[sensitivity]] of 80% to 90%. Throat cultures are much more sensitive, between 90% and 95%. However, they require up to 48 hours for results. | ||
* A test negative for [[Group A streptococcal|GAS]] provides reassurance that the patient likely has a [[viral]] cause of [[pharyngitis]]. A negative test result also allows the clinician to safely avoid the use of antibiotics. Because of the general increase in rates of resistance to antibiotics, [[antimicrobial]] therapy should be prescribed only for proven episodes of [[ GAS]] pharyngitis. | |||
=== Special Considerations in the Diagnosis of Acute Pharyngitis in Adults === | |||
[[Group A streptococcal infection|GAS]] causes only 5%–15% of cases of acute pharyngitis in adults. The risk of [[acute pharyngitis]] due to GAS among adults is higher for parents of school-age children and for those whose occupation brings them into close association with children. However, the risk of a first attack of [[ARF]] is extremely low in adults, even with an undiagnosed and untreated episode of [[streptococcal pharyngitis]]. Because of these epidemiological distinctions, the use of a clinical algorithm without microbiological confirmation has been suggested as an acceptable alternative basis for the diagnosis of infection in adults. However, use of this diagnostic strategy would result in treatment of an unacceptably large number of adults with [[non-streptococcal]] [[pharyngitis]], which is an undesirable result in this age group, which has a low prevalence of [[GAS]] [[pharyngiti]]s and a very low risk of [[rheumatic fever]] or [[Rheumatic heart disease|rheumatic carditis]]. However, routine use of backup throat cultures for those with a negative [[RADT]] is not necessary for adults in usual circumstances, because of the low incidence of GAS pharyngitis in adults and because the risk of subsequent acute rheumatic fever is generally exceptionally low in adults with [[acute pharyngitis]]. | |||
===Special Considerations in the Diagnosis of Acute Pharyngitis in Children <3 Years === | ===Special Considerations in the Diagnosis of Acute Pharyngitis in Children <3 Years === | ||
The prevalence of GAS pharyngitis is significantly lower for children <3 years of age, ranging from 10% to 14%, and if a corresponding rise in [[Antistreptococcal antibodies|Antistreptococcal-O antibody]] (ASO) is required, the prevalence can be as low as 0%– 6%. | The prevalence of [[GAS]] pharyngitis is significantly lower for children <3 years of age, ranging from 10% to 14%, and if a corresponding rise in [[Antistreptococcal antibodies|Antistreptococcal-O antibody]] (ASO) is required, the prevalence can be as low as 0%– 6%. Thus, diagnostic testing for [[GAS]] pharyngitis is not routinely indicated in children <3 years of age. However, if a child is <3 years of age and there is household contact with a school-aged sibling with documented [[streptococcal pharyngitis]], then it is reasonable to consider testing the child if the child is symptomatic. Therefore, if a child is in daycare or another setting with a high rate of cases of [[Group A streptococcal|GAS]] infections, then it is reasonable to test symptomatic children and treat them if they are found to be positive for [[GAS]]. | ||
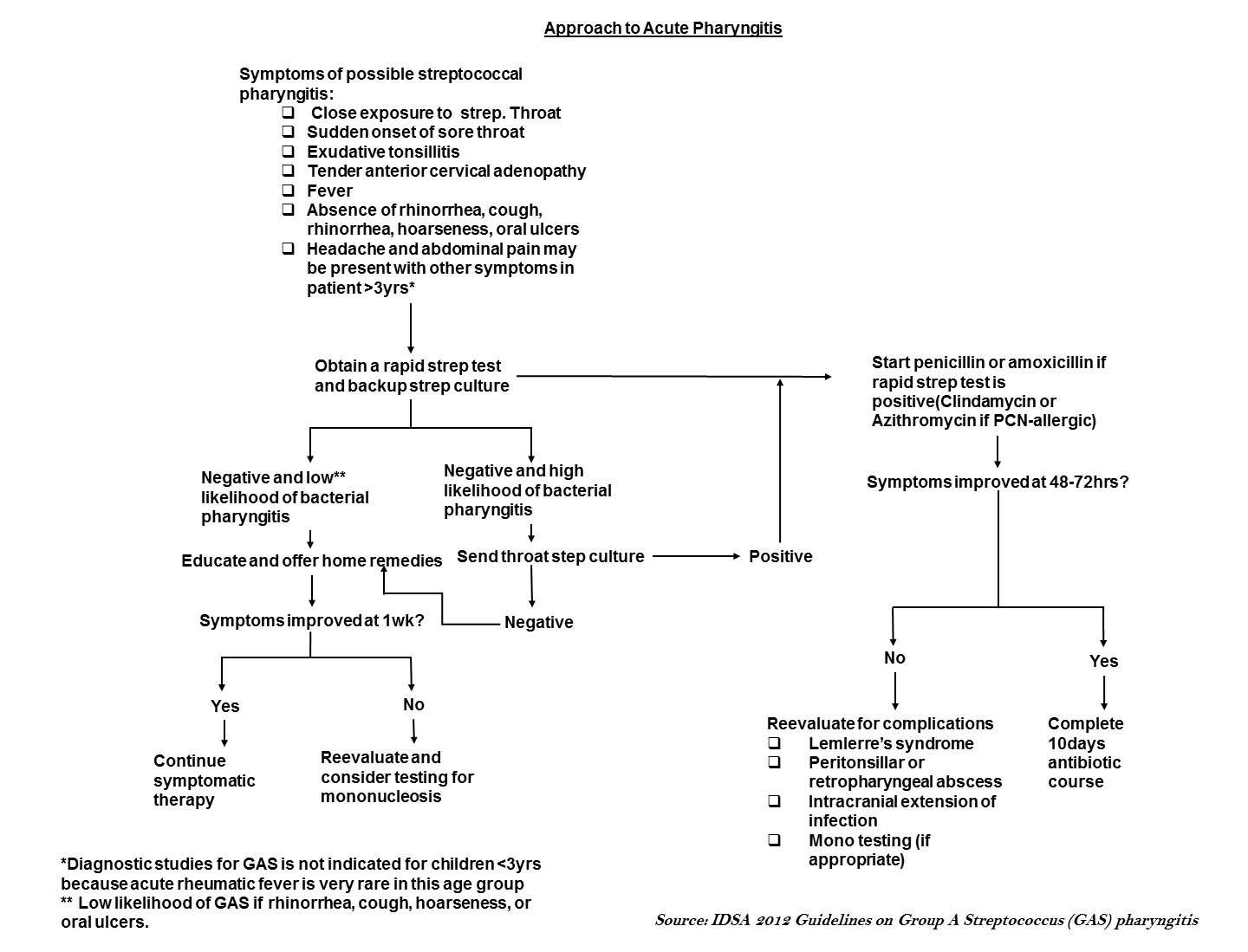
===Algorithm for evaluation of acute pharyngitis=== | ===Algorithm for evaluation of acute pharyngitis=== | ||
The major goal of the evaluation of patients with sore throat or acute pharyngitis is to exclude potentially dangerous causes (e.g. [[Group A streptococcus]]), to identify any treatable causes, and to improve symptoms. Identifying [[group A streptococcus]] (GAS) is important because timely treatment with antibiotics helps prevent post streptococcal complications such as [[acute rheumatic fever]]. | The major goal of the evaluation of patients with [[sore throat]] or [[acute pharyngitis]] is to exclude potentially dangerous causes (e.g. [[Group A streptococcus]]), to identify any treatable causes, and to improve symptoms. Identifying [[group A streptococcus]] (GAS) is important because timely treatment with antibiotics helps prevent post-streptococcal complications such as [[acute rheumatic fever]]. The evaluation includes a thorough history, focused physical examination, and diagnostic testing in selected patients. | ||
[[Image:Evaluation of acute pharyngitis.jpg|1000px]] | [[Image:Evaluation of acute pharyngitis.jpg|1000px]] | ||
== Treatment == | == Treatment == | ||
As is evident from potential etiologic agents of pharyngitis, [[group A streptococcus]] is the only commonly occurring form of acute pharyngitis for which antibiotic therapy is definitely indicated. Therefore, for a patient with acute pharyngitis, the clinical decision that usually needs to be made is whether or not the pharyngitis is attributable to GAS | As is evident from potential etiologic agents of [[pharyngitis]], [[group A streptococcus]] is the only commonly occurring form of [[acute pharyngitis]] for which antibiotic therapy is definitely indicated. Therefore, for a patient with [[acute pharyngitis]], the clinical decision that usually needs to be made is whether or not the pharyngitis is attributable to [[GAS]]. | ||
=== Medical Therapy === | === Medical Therapy === | ||
Patients with acute GAS pharyngitis should be treated with an appropriate antibiotic at an appropriate dose for a duration likely to eradicate the organism from the pharynx (usually 10 days). Based on their narrow spectrum of activity, | Patients with [[acute GAS pharyngitis]] should be treated with an appropriate antibiotic at an appropriate dose for a duration likely to eradicate the organism from the pharynx (usually 10 days). Based on their narrow spectrum of activity, the frequency of adverse reactions, and modest cost, [[penicillin]] or [[amoxicillin]] is the recommended drug of choice for those non-allergic to these agents. Treatment of GAS pharyngitis in penicillin-allergic individuals should include a [[Cephalosporin|first generation cephalosporin]] (for those not anaphylactically sensitive) for 10 days, [[clindamycin]] or [[clarithromycin]] for 10 days, or [[azithromycin]] for 5 days. Adjunctive therapy with [[nonsteroidal anti-inflammatory drugs]] (NSAIDs), [[acetaminophen]], [[aspirin]], or [[Corticosteroid|corticosteroids]] may be useful in the management of GAS pharyngitis. | ||
=== Surgery === | === Surgery === | ||
[[Tonsillectomy]] may be an option for patients with recurrent streptococcal | [[Tonsillectomy]] may be an option for patients with recurrent [[streptococcal]] infections. | ||
=== Prevention === | === Prevention === | ||
Accurate diagnosis of streptococcal pharyngitis followed by appropriate antimicrobial therapy is important for the prevention of [[acute rheumatic fever]] and for the prevention of suppurative complications such as [[peritonsillar abscess]], [[Lymphadenitis|cervical lymphadenitis]], [[mastoiditis]]. | Accurate diagnosis of [[streptococcal pharyngitis]] followed by appropriate [[antimicrobial]] therapy is important for the prevention of [[acute rheumatic fever]] and for the prevention of suppurative complications such as [[peritonsillar abscess]], [[Lymphadenitis|cervical lymphadenitis]], [[mastoiditis]]. | ||
==References== | ==References== | ||
Latest revision as of 18:57, 25 December 2020
|
Pharyngitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pharyngitis overview On the Web |
|
American Roentgen Ray Society Images of Pharyngitis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Venkata Sivakrishna Kumar Pulivarthi M.B.B.S [2]Delband Yekta Moazami, M.D.[3]
Synonyms and keywords: Sore throat; Group A streptococcal pharyngitis; Bacterial pharyngitis; Viral pharyngitis; Acute pharyngitis; Chronic pharyngitis
Overview
A triad of sore throat, fever, and pharyngeal inflammation marked by erythema and edema are usually described as acute pharyngitis, although exudates, vesicles, or ulcerations may also be present. The inflammation of the pharynx, which presents as a sore throat, is pharyngitis. It is a painful inflammation of the pharynx and is colloquially referred to as a sore throat. Pharyngitis is a common medical problem in the outpatient medical setting, resulting in more than seven million pediatric visits each year. Most types of pharyngitis are caused by infectious etiologies. The most common cause of pharyngitis is a viral infection. However, some of the more serious types of pharyngitis are attributed to bacterial etiologies, such as group A-hemolytic Streptococcus pyogenes (GAS). Complications from GAS pharyngitis include rheumatic fever, deep space abscesses, and toxic shock. Although most episodes of pharyngitis are acute in nature, a small percentage becomes recurrent or chronic. With regards to chronic pharyngitis, non-infectious etiologies, such as Laryngopharyngeal reflux disease and periodic fever, aphthous ulcers, pharyngitis, and adenitis syndrome also need to be considered. Both medical and surgical therapies are effective in managing pharyngitis. Antibiotic treatment requires first-line medical therapy. Surgical management via adenotonsillectomy is recommended for certain indications. Adenotonsillectomy has been shown to be effective in reducing the burden of disease and improving the global quality of life and disease-specific. Several procedures, including traditional and intracapsular tonsillectomies, exist for adenotonsillectomy.
Historical Perspective
The sore throat was first described in the literature as 'some variants of sore throat' in the year 1879 by R. L. Bowles, M.D., in the British Medical Journal. Later, in 1885, David Newman, M.D., described pathology, symptoms, and treatment of pharyngitis.In 1910, the importance of bacteriological tests was shown in doubtful cases of pharyngitis. In 1931, three case reports were described and inferred that chronic non-tuberculous bronchial disease such as influenza, whooping cough, and measles is associated with chronic nasopharyngitis and also described the importance of conservative treatment in chronic nasopharyngitis.
Pathophysiology
The pathogenesis of the sore throat due to pharyngitis is poorly understood. The pharynx is often the first site of infection for many contagious diseases such as pharyngitis because pathogens such as viruses and bacteria often settle in the nasopharynx though inhalation or through droplets. Viral pharyngitis usually transmit from person to person through direct touch or through droplets transmission. The foreign invader reproduces rapidly after settling on the nasopharynx. Generally pharyngitis is a primary disease, but may be associated with systemic disorders such as the acute retroviral syndrome, or part of a more generalized upper respiratory tract infection.
Causes
Pharyngitis can be caused by infectious microorganisms or non-infectious agents. It is usually caused by viruses but may be caused by bacterial or fungal etiology. Gastroesophageal reflux disease (GERD) or particularly extra esophageal reflux (EER) can also cause an acid pharyngitis in adults and children.
Classification
Pharyngitis can be classified based on the duration as acute pharyngitis or chronic pharyngitis.
Differential Diagnosis
The major goal of the differentiating patients with sore throat or acute pharyngitis is to exclude potentially dangerous causes (e.g. Group A streptococcus), to identify any treatable causes, and to improve symptoms. Identifying the treatable causes is important because timely treatment with antibiotics helps prevent complications such as acute rheumatic fever, post streptococcal glomerulonephritis. Pharyngitis should be differentiated from other infectious causes which mimic sore throat that includes oral thrush, infectious mononucleosis, epiglottitis and peritonsillar abscess.
Epidemiology and Demographics
With more than 10 million outpatient visits per year, pharyngitis is one of the most common disorders in adults and children. Viruses are the single most common cause of pharyngitis and account for 25 percent to 45 percent of all cases. Group A streptococcus presents in up to 37% of all children presenting with a sore throat to an outpatient clinic or ED and 24% of those presenting at younger than 5 years. Group A streptococcus is by far the most common bacterial cause of acute pharyngitis, accounting for approximately 15 to 30 percent of cases in children and 5 to 10 percent of cases in adults. Peak seasons for sore throat include late winter and early spring.
Risk Factors
Pharyngitis is contagious, so anyone in close proximity to someone with the illness, is at risk. Social situations with prolonged close interpersonal contact are associated with a higher incidence of the disease, such as in schools, dormitories, or military barracks. Other common risk factors include a History of ill contact, Overcrowding, Frequent sinus infections, Smoking, attending daycare, immunocompromised patients, etc.
Natural History, Complications & Prognosis
Acute pharyngitis is typically described as the triad of sore throat, fever, and pharyngeal inflammation characterized by erythema and edema, although exudates, vesicles, or ulcerations may also be present. Although pharyngitis may be a primary disorder, sore throat and pharyngeal erythema may also be prominent in systemic disorders, such as the acute retroviral syndrome, or part of a more generalized upper respiratory tract infection. Most cases of acute pharyngitis are due to common viral infections and are benign, self-limited processes. The appropriate recognition of patients with more complicated infections that require diagnostic evaluations and treatment is one of the challenges of primary care medicine. An estimated 1-2% of acute pharyngitis progresses to recurrent or chronic disease.
Diagnosis
Key points in the evaluation of acute pharyngitis
- Essential to diagnosis is the identification of treatable causes (e.g. Group A streptococcus) to prevent complications.
- Signs and symptoms of GAS pharyngitis include acute onset of sore throat with tonsillar or pharyngeal exudates, tender anterior cervical lymphadenopathy and fever.
- Signs and symptoms consistent with viral etiologies include conjunctivitis, coryza, oral ulcers, cough, and diarrhea.
- Testing for GAS pharyngitis should not be pursued in those with signs and symptoms indicative of a viral etiology.
- Rapid antigen detection tests (RADTs) alone are sufficient for the diagnosis of GAS in adults, but negative results should be backed up by throat culture in children.
- Specific techniques should be used to identify other causes where appropriate.
| Recommendation | American College of Physicians (ACP) | Infectious Diseases Society of America (IDSA) |
|---|---|---|
| Screening for acute pharyngitis | Use Centor criteria | Use clinical and epidemiologic findings to assess patient’s risk of GABHS (e.g., sudden onset of sore throat, fever, odynophagia, tonsillar erythema, exudates, cervical lymphadenitis, or history of streptococcal exposure) |
| Diagnostic testing | RADT with Centor score of 2 or 3 only | RADT or throat culture in all patients at risk |
| Back-up culture needed if RADT results negative? | Adults: No
Children: Yes |
Adults: No
Children: Yes |
| Who requires antibiotic treatment? | Empiric antibiotics for Centor score of 3 or 4; treat patients with positive RADT result | Positive RADT result or throat culture |
| Antibiotic of choice | Oral penicillin V (Veetids; brand no longer available in the United States); intramuscular penicillin G benzathine (Bicillin L-A); oral amoxicillin with equal effectiveness and better palatability in children | |
| Penicillin allergy | Oral erythromycin; cephalosporin (first generation) | |
History and Symptoms
Pharyngitis is a very common inflammatory condition of the pharynx accompanied by a sore throat and occasionally difficulty in swallowing. Other symptoms depends on the etiology such as bacterial or viral.
| Clinical features of acute pharyngitis | |
|---|---|
| Group A streptococcal pharyngitis | Viral pharyngitis |
|
|
Physical Examination
Patients with pharyngitis typically have low-grade fever and pharyngeal erythema, suggestive of viral etiology or pharyngeal exudate or petechia, suggestive of GAS. Additional signs include enlarged edematous tonsils, enlarged and/or tender cervical adenopathy, the rash that may or may not be present. Scarlatiniform rash, which is marked by multiple small red papules that are widely and diffusely distributed but spare the palms and soles, is suggestive of GAS.
Centor criteria
The original Center score uses four signs and symptoms to estimate the probability of acute streptococcal pharyngitis in adults with a sore throat The score was later modified by adding age. It is important to evaluate for a definitive diagnosis to exclude GAS and to avoid unnecessary lab tests and antibiotic use. Centor criteria are a widely used and accepted clinical decision tool in identifying patients for whom neither microbiologic tests nor antimicrobial therapy is necessary. The Center score to use for children and adults with a sore throat to estimate the probability of Streptococcus pyogenes infection.
| Modified Centor criteria | Appropriate management according to the total score | ||||
| Criteria | Points | Total score | Chance of streptococcal infection in community
with usual levels of infection, % |
Suggested management | |
| Fever (temperature > 38°C) | +1 | 0 | 2-3% | No culture or antibiotic is required | |
| Absence of cough | +1 | 1 | 4-6% | ||
| Swollen and tender anterior cervical nodes | +1 | 2 | 10-12% | RADT or Culture and treat only if culture result is positive | |
| Tonsillar swelling or exudates | +1 | 3 | 27-28% | ||
| Age 3–14 yr | +1 | 4 | 38–63% | Culture all and treat emperically with penicillin on clinical grounds | |
| Age 15–44 yr | 0 | ||||
| Age ≥ 45 yr | -1 | ||||
Laboratory Findings
There is a broad overlap between the signs and symptoms of streptococcal and non-streptococcal (usually viral) pharyngitis, and the ability to identify streptococcal pharyngitis accurately on the basis of clinical grounds alone is generally poor. Therefore, except when obvious viral clinical and epidemiological features are present, a laboratory test should be performed to determine whether GAS is present in the pharynx. Even subjects with all clinical features in a particular scoring system can be confirmed to have streptococcal pharyngitis only about 35%–50% of the time and this is particularly the case in children. Swabbing the throat and testing for GAS pharyngitis with rapid antigen detection test (RADT)&/ culture should be performed because the clinical features alone do not reliably discriminate between GAS and viral pharyngitis except when overt viral features like rhinorrhea, cough, oral ulcers, and/or hoarseness are present.
- The rapid streptococcal antigen tests are widely available and have been used and studied extensively as an adjunct to making the diagnosis of GAS pharyngitis. Specificity for the test has been reported to be as high as 95%, with a sensitivity of 80% to 90%. Throat cultures are much more sensitive, between 90% and 95%. However, they require up to 48 hours for results.
- A test negative for GAS provides reassurance that the patient likely has a viral cause of pharyngitis. A negative test result also allows the clinician to safely avoid the use of antibiotics. Because of the general increase in rates of resistance to antibiotics, antimicrobial therapy should be prescribed only for proven episodes of GAS pharyngitis.
Special Considerations in the Diagnosis of Acute Pharyngitis in Adults
GAS causes only 5%–15% of cases of acute pharyngitis in adults. The risk of acute pharyngitis due to GAS among adults is higher for parents of school-age children and for those whose occupation brings them into close association with children. However, the risk of a first attack of ARF is extremely low in adults, even with an undiagnosed and untreated episode of streptococcal pharyngitis. Because of these epidemiological distinctions, the use of a clinical algorithm without microbiological confirmation has been suggested as an acceptable alternative basis for the diagnosis of infection in adults. However, use of this diagnostic strategy would result in treatment of an unacceptably large number of adults with non-streptococcal pharyngitis, which is an undesirable result in this age group, which has a low prevalence of GAS pharyngitis and a very low risk of rheumatic fever or rheumatic carditis. However, routine use of backup throat cultures for those with a negative RADT is not necessary for adults in usual circumstances, because of the low incidence of GAS pharyngitis in adults and because the risk of subsequent acute rheumatic fever is generally exceptionally low in adults with acute pharyngitis.
Special Considerations in the Diagnosis of Acute Pharyngitis in Children <3 Years
The prevalence of GAS pharyngitis is significantly lower for children <3 years of age, ranging from 10% to 14%, and if a corresponding rise in Antistreptococcal-O antibody (ASO) is required, the prevalence can be as low as 0%– 6%. Thus, diagnostic testing for GAS pharyngitis is not routinely indicated in children <3 years of age. However, if a child is <3 years of age and there is household contact with a school-aged sibling with documented streptococcal pharyngitis, then it is reasonable to consider testing the child if the child is symptomatic. Therefore, if a child is in daycare or another setting with a high rate of cases of GAS infections, then it is reasonable to test symptomatic children and treat them if they are found to be positive for GAS.
Algorithm for evaluation of acute pharyngitis
The major goal of the evaluation of patients with sore throat or acute pharyngitis is to exclude potentially dangerous causes (e.g. Group A streptococcus), to identify any treatable causes, and to improve symptoms. Identifying group A streptococcus (GAS) is important because timely treatment with antibiotics helps prevent post-streptococcal complications such as acute rheumatic fever. The evaluation includes a thorough history, focused physical examination, and diagnostic testing in selected patients.
Treatment
As is evident from potential etiologic agents of pharyngitis, group A streptococcus is the only commonly occurring form of acute pharyngitis for which antibiotic therapy is definitely indicated. Therefore, for a patient with acute pharyngitis, the clinical decision that usually needs to be made is whether or not the pharyngitis is attributable to GAS.
Medical Therapy
Patients with acute GAS pharyngitis should be treated with an appropriate antibiotic at an appropriate dose for a duration likely to eradicate the organism from the pharynx (usually 10 days). Based on their narrow spectrum of activity, the frequency of adverse reactions, and modest cost, penicillin or amoxicillin is the recommended drug of choice for those non-allergic to these agents. Treatment of GAS pharyngitis in penicillin-allergic individuals should include a first generation cephalosporin (for those not anaphylactically sensitive) for 10 days, clindamycin or clarithromycin for 10 days, or azithromycin for 5 days. Adjunctive therapy with nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, aspirin, or corticosteroids may be useful in the management of GAS pharyngitis.
Surgery
Tonsillectomy may be an option for patients with recurrent streptococcal infections.
Prevention
Accurate diagnosis of streptococcal pharyngitis followed by appropriate antimicrobial therapy is important for the prevention of acute rheumatic fever and for the prevention of suppurative complications such as peritonsillar abscess, cervical lymphadenitis, mastoiditis.