Peritonsillar abscess
| Peritonsillar abscess | |
| ICD-10 | J36 |
|---|---|
| ICD-9 | 475 |
| DiseasesDB | 11141 |
| eMedicine | emerg/417 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Kiran Singh, M.D. [2] Prince Tano Djan, BSc, MBChB [3]
Overview
Peritonsillar abscess (PTA), also commonly referred to as quinsy, is defined as a collection of pus located between the tonsillar capsule and the pharyngeal constrictor muscles. It is the most common deep tissue infection of the neck.[1] Historically, it has been thought of as a complication of acute tonsillitis. However, recent studies have proposed additional hypothesis surrounding its pathogenesis making the understanding of the disease a medical dilemma.[2]
Historical perspective
The outline below shows the historical perspective of peritonsillar abscess.[3]
- In Second and third century BC, Celcius was the first to document in literature the treatment and pathogenesis of tonsillar pathology.
- In 1700s peritonsillar abscess was first described.
- In the 1930s and 1940s prior to the advent of antibiotics, surgical management was the most common treatment option for peritonsillar abscess. Interval tonsillectomy was mostly done after symptom resolution.
- By 1947, Chaud tonsillectomy or immediate surgical tonsillectomy became the treatment option.
Classification
On the basis of computed tomographical findings, peritonsillar abscess may be classified into 3 broad categories based on the following:
1. Shape of the abscess
On the basis of shaped it may be classified as:[4]
- Oval type or
- Cap type
2. Location of the abscess
On the basis of abscess location it may be differentiated into the following:[4]
- Superior or
- Inferior
3. Shape and location
On the basis of shaped and location it may be classified as:[4]
Pathophysiology
Anatomy
A good understanding of the tonsil and its surrounding space is important in the pathogenesis of peritonsillar abscess. The palatine tonsils are found in an anatomical structure called tonsillar fossa. This fossa is bounded anteriorly by palatoglossal muscle, posteriorly by palatopharyngeal muscle, laterally by a fibrous capsule and tonsillar crypts medially. Contents of the tonsillar crypts are expelled by contraction of the tonsillopharyngeus muscle.[5] The tonsils form during the last months of pregnancy and becomes fully formed by 6 to 7 years of age. It then undergoes involution until small size remains in older population. Located within the soft palate is the supratonsillar space occupied by series of 20 to 25 salivary glands described as Weber's glands. The ducts of these glands form a common duct which opens onto the posterior surface of the tonsil after passing through the tonsillar capsule. It is proposed that the secretions from these glands play a rule in food digestion. Peritonsillar abscesses form in the area between the palatine tonsil and its capsule.
Pathogenesis
The pathogenesis of peritonsillar abscess is still not well-understood.[2] There are two proposed theories believed to be involved in the pathogensis of peritonsillar abscess formation.[5][3][6][7]
- 1. It is proposed to arise from an extension of exudative tonsillitis.
Some authorities believe that blockage of drainage from tonsillar crypt in acute tonsillitis results in spread of infection into the peritonsillar space.
- 2. Involvement of Weber's gland account for the abscess formation. Some believe that peritonsillar abscess arises from infectious process involving group of salivary glands called Weber's glands located in the supratonsillar space.
Antigenic response following any disturbance arising from within the tonsillar crypt mucosa allows for lymphocytic interaction. This disruption in the crypt epithelium may be preceded by infectious process. Invasion and proliferation of the tonsillar crypt by infectious pathogens results in localized edema and influx of neutrophils. This is clinically seen as inflammed tonsil with or without exudation.[5] Pus accumulation within tissue behind the supratonsillar space leads to tonsillar bulging, uvula and palate deviation.
Gross pathology
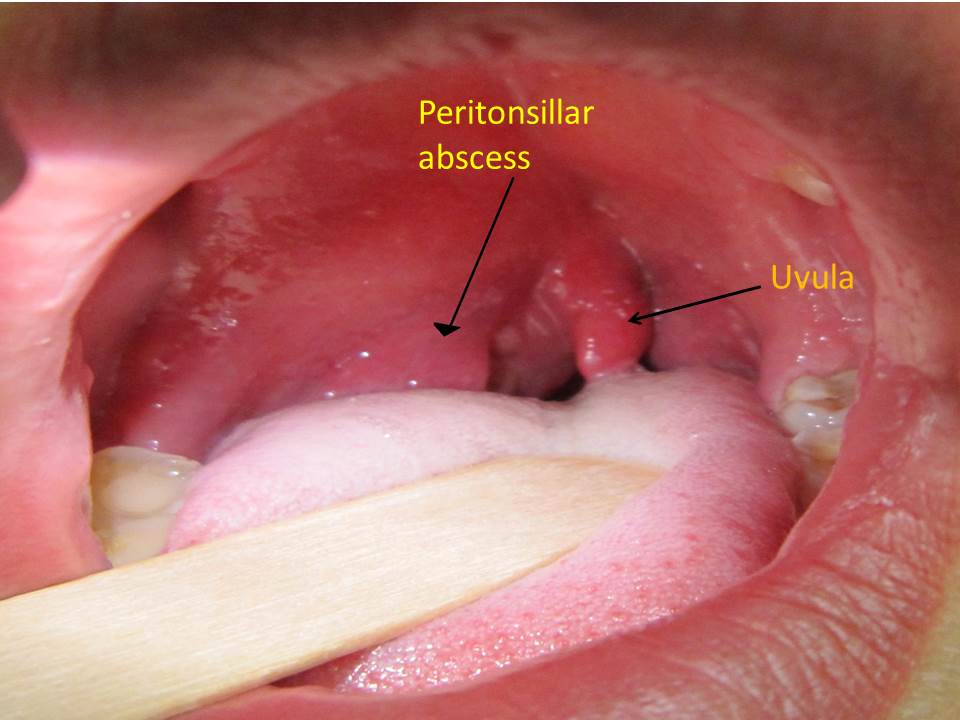
On gross pathology, the tonsillar region is edematous and inflammed as shown below: [8]
Causes
PTA usually arises as a complication of an untreated or partially treated episode of acute tonsillitis. The infection, in these cases, spreads to the peritonsillar area (peritonsillitis). This region comprises loose connective tissue and is hence susceptible to formation of abscess. Peritonsilar abscess can also occur de novo. Both aerobic and anaerobic bacteria can be causative.[9][9]
Life-threatening causes
Life-threatening conditions may result in death or permanent disability within 24 hours if left untreated. Peritonsillar abscess may become a life-threatening condition and must be treated as such irrespective of the cause.[10][9]
Most common cause
The most frequent pathogen of peritonsillar abscess is Streptococcus pyogenes.[10][9][11][12]
Common causes
Some common causes of peritonsillar abscess include:[10][9]
- Fusobacterium necrophorum
- Streptococcus milleri
- Staphylococci
- Haemophilus
- Fusobacterium
- Prevotella
- Acinetobacter spp.
- Candida albicans
- Peptostreptococcus spp.
- Pseudomonas spp.
- Enterobacter spp.
- Klebsiella
Less common causes
Less common causes of peritonsillar abscess include:[10][9]
Differentiating Peritonsillar abscess from Other Diseases
| Variable | Peritonsillar abscess | Croup | Epiglottitis | Pharyngitis | Tonsilitis | Retropharyngeal abscess | |
|---|---|---|---|---|---|---|---|
| Presentation | Cough | ✔ | — | Sore throat, pain on swallowing, fever, headache, abdominal pain, nausea and vomiting | Sore throat, pain on swallowing, fever, headache, cough | Neck pain, stiff neck, torticollis | |
| Stridor | ✔ | ✔ | |||||
| Drooling | — | ✔ | |||||
| Others are Hoarseness, Difficulty breathing, symptoms of the common cold, Runny nose, Fever | Other symptoms include difficulty breathing, fever, chills, difficulty swallowing, hoarseness of voice | ||||||
| Causes | Parainfluenza virus | H. influenza type b, beta-hemolytic streptococci, Staphylococcus aureus, fungi and viruses. | Group A beta-hemolytic streptococcus. | Most common cause is viral including adenovirus, rhinovirus, influenza, coronavirus, and respiratory syncytial virus. Second most common causes are bacterial; Group A streptococcal bacteria,[13] | Polymicrobial infection. Mostly; Streptococcus pyogenes, Staphylococcus aureus and respiratory anaerobes (example; Fusobacteria, Prevotella, and Veillonella species)[14][15][16][10][17][18] | ||
| Physical exams findings | Suprasternal and intercostal indrawing,[19] Inspiratory stridor[20], expiratory wheezing,[20] Sternal wall retractions[21] | Cyanosis, Cervical lymphadenopathy, Inflammed epiglottis | Inflammed pharynx with or without exudate | Fever, especially 100°F or higher.[22][23]Erythema, edema and Exudate of the tonsils.[24] cervical lymphadenopathy, Dysphonia.[25] | Child may be unable to open the mouth widely. May have enlarged
cervical lymph nodes and neck mass. | ||
| Age commonly affected | The highest occurrence is in adults between 20 to 40 years of age.[1] | Mainly 6 months and 3 years old
rarely, adolescents and adults[26] |
Used to be mostly found in
pediatric age group between 3 to 5 years, however, recent trend favors adults as most commonly affected individuals[27] with a mean age of 44.94 years. |
Mostly in children and young adults,
with 50% of cases identified between the ages of 5 to 24 years.[28] |
Primarily affects children
between 5 and 15 years old.[29] |
Mostly between 2-4 years, but can occur in other age groups.[30][31] | |
| Imaging finding | Steeple sign on neck X-ray | Thumbprint sign on neck x-ray | — | Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.[4][32][33] | On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen[34][35] | ||
| Treatment | Dexamethasone and nebulised epinephrine | Airway maintenance, parenteral Cefotaxime or Ceftriaxone in combination with Vancomycin. Adjuvant therapy includes corticosteroids and racemic Epinephrine.[36][37] | Antimicrobial therapy mainly penicillin-based and analgesics. | Antimicrobial therapy mainly penicillin-based and analgesics with tonsilectomy in selected cases. | Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; ampicillin-sulbactam or clindamycin. | ||
Other differential diagnosis not listed in the table includes:
- Infectious mononucleosis,
- Lymphoma,
- Peritonsillar cellulitis
Epidemiology and Demographics
Prevalence and incidence
The incidence of peritonsillar abscess is highest between November to December and April to May. This has been associated with the highest rates of streptococcal pharyngitis and exudative tonsillitis around that these times.[38][39]
Age
Peritonsillar abscess occur in all age groups. The highest occurrence is in adults between 20 to 40 years of age.[1][40][41]
Race
There is no racial predilection to developing peritonsillar abscess.
Gender
Males are more commonly affected with peritonsillar abscess than female with male to female ratio of approximately 1.4:1. However, equal male to female ratios have been reported in some studies as well.[42][43][44][45][46][47][48]
Developed and developing countries
Peritonsillar abscess has not been found to vary significantly among countries.
Risk Factors
Common risk factors in the development of peritonsillar abscess include:[49][50]
- Smoking
- Previous PTA episodes
- History of recurrent pharyngotonsillitis
- Poor oral hygiene
Screening
Natural History, Complications, and Prognosis
Natural history
Complications
The following are some complications that may follow peritonsillar abscess:
- Extraperitonsillar spread example parapharyngeal extension, deep neck tissues and posterior mediastinum[51][52][4]
Peritonsillar abscess may spread through the deep fascia of the neck with associated rapid progression to a more serious infection.
- Airway obstruction
- Aspiration pneumonitis or lung abscess secondary to peritonsillar abscess rupture
- Death secondary to hemorrhage from erosion or septic necrosis into carotid sheath
- Poststreptococcal sequelae (e.g., glomerulonephritis, rheumatic fever) when infection is caused by Group A streptococcus
Prognosis
Diagnosis
History and Symptoms
- Unlike tonsillitis, which is more common in the pediatric age group, peritonsillar abscess has a more even age spread — from children to adults.
- Drooling
- Dysphagia
- Foul smelling breath
- Fever
- Headache
- Hoarseness,muffled voice (also called hot potato voice)
- Odynophagia
- Otalgia (on the side of the abscess)
- Sore throat ( may be severe and unilateral)
- Stridor[53]
- Malaise
Physical Examination
Physical examination findings suggestive of peritonsillar abscess include the following:[1][54][3][55]
- Muffled voice (also called "hot potato voice")
- Contralateral deflection of the uvula
- The tonsil is generally displaced inferiorly and medially
- Facial swelling
- Tender submandibular and anterior cervical lymph nodes
- Tonsillar hypertrophy with likely peritonsillar edema.
- Trismus
- Drooling
- Rancid or fetor breath
Laboratory Findings
Imaging Findings
Treatment
Medical Therapy
Antimicrobial Regimen
Surgery
Prevention
Primary prevention
Secondary Prevention
Notable Quinsy sufferers
- George Washington is believed to have died of complications arising from Quinsy.[56]
- Michel de Montaigne's quinsy brought about the paralysis of his tongue.
- Georges Bizet
- James Gregory of the band The Ordinary Boys was almost killed by quinsy because it was left untreated
- Brian Sweeney
- Alan Burrows
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Galioto NJ (2008). "Peritonsillar abscess". Am Fam Physician. 77 (2): 199–202. PMID 18246890.
- ↑ 2.0 2.1 Powell EL, Powell J, Samuel JR, Wilson JA (2013). "A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation". J Antimicrob Chemother. 68 (9): 1941–50. doi:10.1093/jac/dkt128. PMID 23612569.
- ↑ 3.0 3.1 3.2 Passy V (1994). "Pathogenesis of peritonsillar abscess". Laryngoscope. 104 (2): 185–90. doi:10.1288/00005537-199402000-00011. PMID 8302122.
- ↑ 4.0 4.1 4.2 4.3 4.4 Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H; et al. (2016). "Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy". Auris Nasus Larynx. 43 (2): 182–6. doi:10.1016/j.anl.2015.09.014. PMID 26527518.
- ↑ 5.0 5.1 5.2 L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286
- ↑ Blair AB, Booth R, Baugh R (2015). "A unifying theory of tonsillitis, intratonsillar abscess and peritonsillar abscess". Am J Otolaryngol. 36 (4): 517–20. doi:10.1016/j.amjoto.2015.03.002. PMID 25865201.
- ↑ Herzon FS, Martin AD (2006). "Medical and surgical treatment of peritonsillar, retropharyngeal, and parapharyngeal abscesses". Curr Infect Dis Rep. 8 (3): 196–202. PMID 16643771.
- ↑ DescriptionEnglish: A right sided peritonsilar abscess Date 13 May 2011 Source Own work Author James Heilman,MD wikimedia commons https://commons.wikimedia.org/wiki/File:PeritonsilarAbsess.jpg
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S (2008). "Changing trends in bacteriology of peritonsillar abscess". J Laryngol Otol. 122 (9): 928–30. doi:10.1017/S0022215107001144. PMID 18039418.
- ↑ 10.0 10.1 10.2 10.3 10.4 Brook I (2004). "Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses". J Oral Maxillofac Surg. 62 (12): 1545–50. PMID 15573356.
- ↑ Snow DG, Campbell JB, Morgan DW (1991). "The microbiology of peritonsillar sepsis". J Laryngol Otol. 105 (7): 553–5. PMID 1875138.
- ↑ Matsuda A, Tanaka H, Kanaya T, Kamata K, Hasegawa M (2002). "Peritonsillar abscess: a study of 724 cases in Japan". Ear Nose Throat J. 81 (6): 384–9. PMID 12092281.
- ↑ Putto A (1987). "Febrile exudative tonsillitis: viral or streptococcal?". Pediatrics. 80 (1): 6–12. PMID 3601520.
- ↑ Cheng J, Elden L (2013). "Children with deep space neck infections: our experience with 178 children". Otolaryngol Head Neck Surg. 148 (6): 1037–42. doi:10.1177/0194599813482292. PMID 23520072.
- ↑ Abdel-Haq N, Quezada M, Asmar BI (2012). "Retropharyngeal abscess in children: the rising incidence of methicillin-resistant Staphylococcus aureus". Pediatr Infect Dis J. 31 (7): 696–9. doi:10.1097/INF.0b013e318256fff0. PMID 22481424.
- ↑ Inman JC, Rowe M, Ghostine M, Fleck T (2008). "Pediatric neck abscesses: changing organisms and empiric therapies". Laryngoscope. 118 (12): 2111–4. doi:10.1097/MLG.0b013e318182a4fb. PMID 18948832.
- ↑ Wright CT, Stocks RM, Armstrong DL, Arnold SR, Gould HJ (2008). "Pediatric mediastinitis as a complication of methicillin-resistant Staphylococcus aureus retropharyngeal abscess". Arch Otolaryngol Head Neck Surg. 134 (4): 408–13. doi:10.1001/archotol.134.4.408. PMID 18427007.
- ↑ Asmar BI (1990). "Bacteriology of retropharyngeal abscess in children". Pediatr Infect Dis J. 9 (8): 595–7. PMID 2235179.
- ↑ Johnson D (2009). "Croup". BMJ Clin Evid. 2009. PMC 2907784. PMID 19445760.
- ↑ 20.0 20.1 Cherry, James D. (2008). "Croup". New England Journal of Medicine. 358 (4): 384–391. doi:10.1056/NEJMcp072022. ISSN 0028-4793.
- ↑ Johnson D (2009). "Croup". BMJ Clin Evid. 2009. PMC 2907784. PMID 19445760.
- ↑ Tonsillitis. Medline Plus. https://www.nlm.nih.gov/medlineplus/ency/article/001043.htm. Accessed May 2nd, 2016.
- ↑ "Tonsillitis - NHS Choices".
- ↑ Stelter K (2014). "Tonsillitis and sore throat in children". GMS Curr Top Otorhinolaryngol Head Neck Surg. 13: Doc07. doi:10.3205/cto000110. PMC 4273168. PMID 25587367.
- ↑ "Tonsillitis - Symptoms - NHS Choices".
- ↑ Tong MC, Chu MC, Leighton SE, van Hasselt CA (1996). "Adult croup". Chest. 109 (6): 1659–62. PMID 8769531.
- ↑ Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED (2016). "Epiglottitis: It Hasn't Gone Away". Anesthesiology. 124 (6): 1404–7. doi:10.1097/ALN.0000000000001125. PMID 27031010.
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Sharav, Yair; Benoliel, Rafael (2008). Orofacial Pain and Headache. Elsevier. ISBN 0723434123.
- ↑ Craig FW, Schunk JE (2003). "Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management". Pediatrics. 111 (6 Pt 1): 1394–8. PMID 12777558.
- ↑ Coulthard M, Isaacs D (1991). "Neonatal retropharyngeal abscess". Pediatr Infect Dis J. 10 (7): 547–9. PMID 1876473.
- ↑ Nogan S, Jandali D, Cipolla M, DeSilva B (2015). "The use of ultrasound imaging in evaluation of peritonsillar infections". Laryngoscope. 125 (11): 2604–7. doi:10.1002/lary.25313. PMID 25946659.
- ↑ Fordham MT, Rock AN, Bandarkar A, Preciado D, Levy M, Cohen J; et al. (2015). "Transcervical ultrasonography in the diagnosis of pediatric peritonsillar abscess". Laryngoscope. 125 (12): 2799–804. doi:10.1002/lary.25354. PMID 25945805.
- ↑ Philpott CM, Selvadurai D, Banerjee AR (2004). "Paediatric retropharyngeal abscess". J Laryngol Otol. 118 (12): 919–26. PMID 15667676.
- ↑ Vural C, Gungor A, Comerci S (2003). "Accuracy of computerized tomography in deep neck infections in the pediatric population". Am J Otolaryngol. 24 (3): 143–8. PMID 12761699.
- ↑ Nickas BJ (2005). "A 60-year-old man with stridor, drooling, and "tripoding" following a nasal polypectomy". J Emerg Nurs. 31 (3): 234–5, quiz 321. doi:10.1016/j.jen.2004.10.015. PMID 15983574.
- ↑ Wick F, Ballmer PE, Haller A (2002). "Acute epiglottis in adults". Swiss Med Wkly. 132 (37–38): 541–7. PMID 12557859.
- ↑ Belleza WG, Kalman S (2006). "Otolaryngologic emergencies in the outpatient setting". Med Clin North Am. 90 (2): 329–53. doi:10.1016/j.mcna.2005.12.001. PMID 16448878.
- ↑ Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH, Infectious Diseases Society of America (2002). "Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America". Clin Infect Dis. 35 (2): 113–25. doi:10.1086/340949. PMID 12087516.
- ↑ Steyer TE (2002). "Peritonsillar abscess: diagnosis and treatment". Am Fam Physician. 65 (1): 93–6. PMID 11804446.
- ↑ Khayr W, Taepke J (2005). "Management of peritonsillar abscess: needle aspiration versus incision and drainage versus tonsillectomy". Am J Ther. 12 (4): 344–50. PMID 16041198.
- ↑ Ong YK, Goh YH, Lee YL (2004). "Peritonsillar infections: local experience". Singapore Med J. 45 (3): 105–9. PMID 15029410.
- ↑ Marom T, Cinamon U, Itskoviz D, Roth Y (2010). "Changing trends of peritonsillar abscess". Am J Otolaryngol. 31 (3): 162–7. doi:10.1016/j.amjoto.2008.12.003. PMID 20015734.
- ↑ Klug TE (2014). "Incidence and microbiology of peritonsillar abscess: the influence of season, age, and gender". Eur J Clin Microbiol Infect Dis. 33 (7): 1163–7. doi:10.1007/s10096-014-2052-8. PMID 24474247.
- ↑ Gavriel H, Lazarovitch T, Pomortsev A, Eviatar E (2009). "Variations in the microbiology of peritonsillar abscess". Eur J Clin Microbiol Infect Dis. 28 (1): 27–31. doi:10.1007/s10096-008-0583-6. PMID 18612664.
- ↑ Sunnergren O, Swanberg J, Mölstad S (2008). "Incidence, microbiology and clinical history of peritonsillar abscesses". Scand J Infect Dis. 40 (9): 752–5. doi:10.1080/00365540802040562. PMID 19086341.
- ↑ Hidaka H, Kuriyama S, Yano H, Tsuji I, Kobayashi T (2011). "Precipitating factors in the pathogenesis of peritonsillar abscess and bacteriological significance of the Streptococcus milleri group". Eur J Clin Microbiol Infect Dis. 30 (4): 527–32. doi:10.1007/s10096-010-1114-9. PMID 21086007.
- ↑ Costales-Marcos M, López-Álvarez F, Núñez-Batalla F, Moreno-Galindo C, Alvarez Marcos C, Llorente-Pendás JL (2012). "[Peritonsillar infections: prospective study of 100 consecutive cases]". Acta Otorrinolaringol Esp. 63 (3): 212–7. doi:10.1016/j.otorri.2012.01.001. PMID 22425204.
- ↑ Lehnerdt G, Senska K, Fischer M, Jahnke K (2005). "[Smoking promotes the formation of peritonsillar abscesses]". Laryngorhinootologie. 84 (9): 676–9. doi:10.1055/s-2005-870289. PMID 16142623.
- ↑ Dilkes MG, Dilkes JE, Ghufoor K (1992). "Smoking and quinsy". Lancet. 339 (8808): 1552. PMID 1351238.
- ↑ Coughlin AM, Baugh RF, Pine HS (2014). "Lingual tonsil abscess with parapharyngeal extension: a case report". Ear Nose Throat J. 93 (9): E7–8. PMID 25255362.
- ↑ Deeva YV (2015). "[SURGICAL TREATMENT OF TONSILLAR NECK PHLEGMON]". Klin Khir (7): 47–8. PMID 26591220.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Nwe TT, Singh B (2000). "Management of pain in peritonsillar abscess". J Laryngol Otol. 114 (10): 765–7. PMID 11127146.
- ↑ Mount Vernon Plantation (2006). "Part 4. President and Back Home". Meet George Washington. Mount Vernon Ladies Association. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help)
External links
Template:Respiratory pathology
ka:პერიტონზილური აბსცესი nl:Peritonsillair abces fi:Kurkkupaise