Oral candidiasis laboratory findings: Difference between revisions
Ahmed Younes (talk | contribs) |
Ahmed Younes (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Oral candidiasis}} {{CMG}} | {{Oral candidiasis}} | ||
{{CMG}}{{AY}} | |||
==Overview== | ==Overview== | ||
Diagnosis of oral candidiasis is usually clinical based on symptoms and physical examination. A culture may also be performed; however, because [[Candida]] organisms are normal inhabitants of the human mouth, a positive culture by itself does not make the diagnosis. | Diagnosis of oral candidiasis is usually clinical based on symptoms and physical examination. A culture may also be performed; however, because [[Candida]] organisms are normal inhabitants of the human mouth, a positive culture by itself does not make the diagnosis. | ||
Revision as of 16:44, 10 May 2017
|
Oral candidiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Oral candidiasis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Oral candidiasis laboratory findings |
|
Risk calculators and risk factors for Oral candidiasis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Ahmed Younes M.B.B.CH [2]
Overview
Diagnosis of oral candidiasis is usually clinical based on symptoms and physical examination. A culture may also be performed; however, because Candida organisms are normal inhabitants of the human mouth, a positive culture by itself does not make the diagnosis.
Laboratory Findings
Diagnosis of oropharyngeal candidiasis is usually clinical and confirmatory diagnostic tests are rarely needed. Oral smears are obtained through gentle scraping of the lesions and spreading the debris directly on a glass slide. In cases of hyperplastic candidiasis, biopsy is indiccated.[1] Both smears and biopsies can be stained by periodic acid Schiff stain which stains the walls of the fungi red. Candida also can be stained using gram stain (strongly gram positive)[2]
Histopathologic examination:
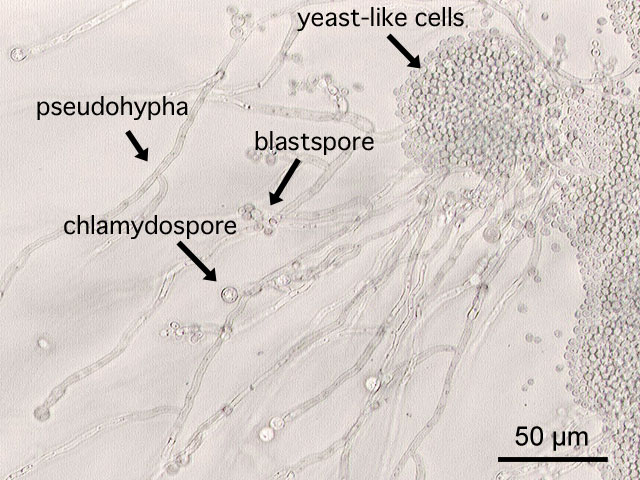
Blastospores (yeast form) and pseudohyphae in the superficial epithelial layer is very characteristic for candidiasis. Blastospores can be present in other opportunistic fungal infections ( Cryptococcus neoformans or Histoplasma capsulatum) that can have similar presentation and present in immunocompromised patient. If candida is suspected clinically while only blastospores are evident in histopathologic examination, exmamining more smears searching for pseusohyphae is indicated.[3][2]
Pseusdomembranous candidiasis:
Epithilium appears thickened wiith parakeratosis (superficial separation of a layer of the epithelium). Epithilium is usually infilitrated by PMNs and lamina propria is infiltrated by chronic inflammatory cells. Pseudohyphae appear as weakly basophilic structures that is embedded within the epithelium.[3][2]
Atrophic candidiasis:
Atrophic candidiasis is similar to pseusdomembranous candidiasis but the difference is in the absence of parakeratosis. Epithelium is usually atrophic and thin.[3][2]
Hyperplastic candidiasis:
Epithelium is ususallly hyperplastic, hyperkeratotic and acanthotic with dysplasia in some cases.[3][2]
 |
 |
|---|---|
 |
 |
References
- ↑ Moris DV, Melhem MS, Martins MA, Souza LR, Kacew S, Szeszs MW, Carvalho LR, Pimenta-Rodrigues MV, Berghs HA, Mendes RP (2012). "Prevalence and antifungal susceptibility of Candida parapsilosis complex isolates collected from oral cavities of HIV-infected individuals". J. Med. Microbiol. 61 (Pt 12): 1758–65. doi:10.1099/jmm.0.045112-0. PMID 22956748.
- ↑ 2.0 2.1 2.2 2.3 2.4 Kumaraswamy KL, Vidhya M, Rao PK, Mukunda A (2012). "Oral biopsy: oral pathologist's perspective". J Cancer Res Ther. 8 (2): 192–8. doi:10.4103/0973-1482.98969. PMID 22842360.
- ↑ 3.0 3.1 3.2 3.3 Sangeorzan JA, Bradley SF, He X, Zarins LT, Ridenour GL, Tiballi RN, Kauffman CA (1994). "Epidemiology of oral candidiasis in HIV-infected patients: colonization, infection, treatment, and emergence of fluconazole resistance". Am. J. Med. 97 (4): 339–46. PMID 7942935.