Oral candidiasis: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
{{Infobox_Disease | {{Infobox_Disease | ||
| Line 15: | Line 16: | ||
| MeshID = | | MeshID = | ||
}} | }} | ||
{{ | {{Oral candidiasis}} | ||
{{CMG}} | {{CMG}} | ||
Revision as of 20:11, 26 November 2012
For patient information click here
| Oral candidiasis | |
 | |
|---|---|
| Oral thrush | |
| ICD-10 | B37.0 |
| ICD-9 | 112.0 |
| DiseasesDB | 29743 |
| MedlinePlus | 000966 |
|
Oral candidiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Oral candidiasis On the Web |
|
American Roentgen Ray Society Images of Oral candidiasis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and related key words: OPC, thrush, oral thrush, candidiasis of the mouth and throat, candidosis, oral moniliasis
Overview
Oral candidiasis, is an infection of yeast fungus, Candida albicans, (or, less commonly, Candida glabrata or Candida tropicalis) in the mucous membranes of the mouth.
Pathophysiology
Candida albicans and C. glabrata. Less commonly, C.tropicalis, C. parapsilosis, and C. krusei. Rarely, other Candida species. Most cases of OPC are caused by the person’s own Candida organisms which normally live in the mouth or digestive tract. A person has symptoms when overgrowth of Candida organisms occurs.
Most infections are endogenous in origin, but organisms can be transmitted on the hands of care givers.
Epidemiology and Demographics
- Thrush is the fourth most common cause of nosocomial bloodstream infections.
- The incidence is 8 cases per 100,000 in the general population.
- Higher incidence among neonates and African-Americans.
- OPC used to be a common opportunistic infection in HIV-infected persons (prior to the introduction of highly active antiretroviral therapy HAART).
Natrual History, Comoplications, Prognosis
There are no sequela with appropriate antifungal therapy. In contrast, among immunocompromised patients with disseminated infections, the mortality rate is almost 50%.
Risk Factors
Invasive disease occurs in critically ill patients in intensive-care units, in persons with severe granulocytopenia, and in hematopoietic stem cell and organ transplant recipients. OPC can be associated with HIV infection. VVC is often associated with pregnancy, diabetes mellitus, and antibiotic therapy.
Who is at special risk?
- Newborn babies.
- Denture users.
- Poorly controlled diabetes.
- As a side effect of medication, most commonly having taken antibiotics. Inhaled corticosteroids for treatment of lung conditions (e.g, Asthma or COPD) may also result in oral candidiasis which may be reduced by regularly rinsing the mouth with water after taking the medication.
- People with poor nutrition, specifically vitamin A, iron and folate deficiencies.
- People with an immune deficiency (e.g. as a result of AIDS/HIV or chemotherapy treatment).
- Women undergoing hormonal changes, like pregnancy or those on birth control pills
- People who perform cunnilingus or fellatio on a sexual partner who has thrush.
Thrush and Breastfeeding
Because of the increased use of antibiotics in laboring women to reduce the transmission of Group B streptococcal infection to the infant, thrush has become more prevalent. Symptoms include:
- An oral rash in the infant's mouth
- A diaper rash that does not heal with conventional diaper rash treatments and ointments,
- Burning, painful nipples for the breastfeeding mother.
The rash and pain experienced by the mother can range from severe to mild and may complicate breastfeeding. Because thrush is assumed to be benign, it may be difficult to obtain treatment for an outbreak in the diaper area of an infant or mother's nipples. Over the counter yeast infection cream, that comes in the 7-day package, can be applied to the skin with good results within 24 - 48 hours. It should be washed off nipples before breastfeeding.
Diagnosis
Symptoms
Adults may experience discomfort or burning in the mouth. Symptoms of candidiasis in the esophagus may include pain and dysphagia (difficult swallowing).
In babies the condition is termed thrush and is usually painless and causes no discomfort.
Physical Examination
Oral infections of candidia usually appear as thick white or cream-colour deposits. Underlying the deposits the mucosa of the mouth may appear inflamed (red and possibly slightly raised). Oral lesions are painless, white patches in the mouth.
-
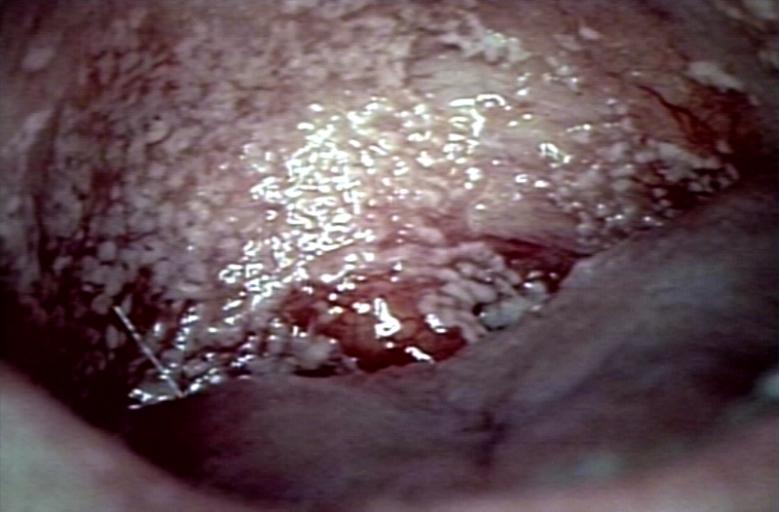
Oral manifestations of HIV infection and AIDS. Chronic oral candidiasis in patient with AIDS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
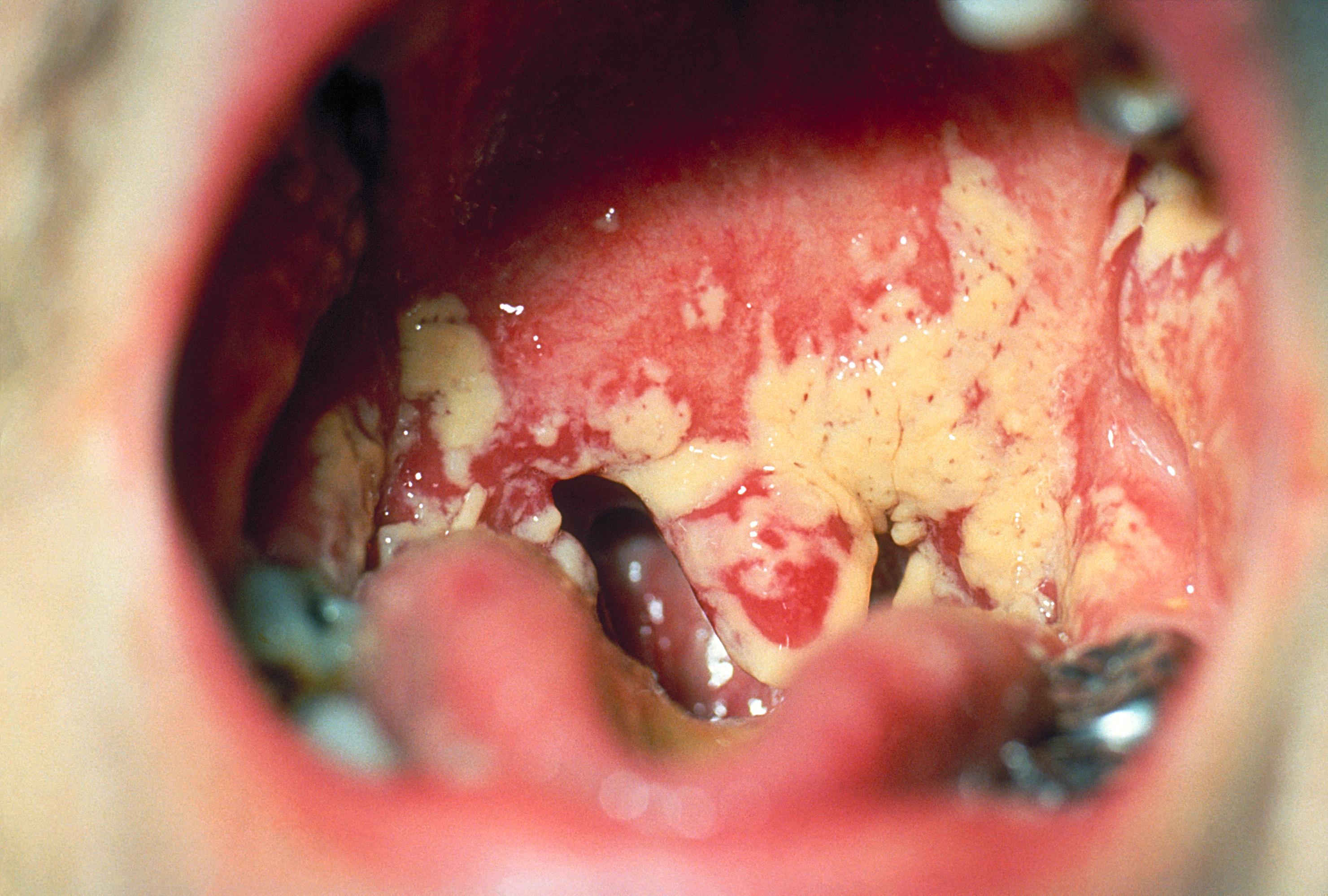
Soft palate showing extensive oral candidiasis in patient with AIDS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
Laboratory Studies

Treatment
Any underlying cause, such as poor glucose control in diabetics, should be addressed. Oral candidiasis can be treated with topical anti-fungal drugs, such as nystatin (mycostatin), miconazole or amphotericin B. Patients who are immunocompromised, either with HIV/AIDS or as a result of chemotherapy, may require systemic treatment with oral or intravenous administered anti-fungals.
For adults, mild cases can be first treated by drinking acidic substances, such as orange juice, to make a harsher environment for the yeast and eating yogurt to replenish bacterial count that controls the yeast. If home treatment is not effective a physician may need to be consulted.
Prevention
Nosocomial disease surveillance is conducted by NNIS in selected hospitals. Active population-based surveillance for candidemia is being conducted in selected U.S. sites.