|
|
| (36 intermediate revisions by 8 users not shown) |
| Line 1: |
Line 1: |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | | __NOTOC__ |
| | '''For patient information page on this topic, click [[{{PAGENAME}} (patient information)|here]].''' |
| {{Infobox_Disease | | {{Infobox_Disease |
| | Name = Oral candidiasis | | | Name = Oral candidiasis |
| | Image = Oral thrush.JPG | | | Image = Oral thrush.JPG |
| | Caption = Oral thrush | | | Caption = Oral thrush |
| | DiseasesDB = 29743
| |
| | ICD10 = {{ICD10|B|37|0|b|35}}
| |
| | ICD9 = {{ICD9|112.0}}
| |
| | ICDO =
| |
| | OMIM =
| |
| | MedlinePlus = 000966
| |
| | eMedicineSubj =
| |
| | eMedicineTopic =
| |
| | eMedicine_mult =
| |
| | MeshID =
| |
| }} | | }} |
| {{SI}} | | {{Oral candidiasis}} |
|
| |
|
| {{CMG}} | | {{CMG}} '''Associate Editor(s)-In-Chief:''' [[User: Prashanthsaddala|Prashanth Saddala M.B.B.S]] |
|
| |
|
| '''''Synonyms and related key words:''''' OPC, thrush, [[Candidiasis]] of the mouth and throat
| | {{SK}} OPC; thrush; oral thrush; candidiasis of the mouth and throat; candidosis; oral moniliasis; oropharyngeal candidiasis |
| | ==[[Oral candidiasis overview|Overview]]== |
|
| |
|
| ==Overview== | | ==[[Oral candidiasis historical perspective|Historical Perspective]]== |
| '''Oral [[candidiasis]]''', is an infection of [[yeast]] fungus, ''[[Candida albicans]]'', (or, less commonly, ''[[Candida glabrata]]'' or ''[[Candida tropicalis]]'') in the mucous membranes of the [[mouth]]. '''Oral thrush''' refers to temporary candidiasis in the mouths of babies, whilst if occurring in the mouth or throat of adults it may also be termed '''candidosis''' or '''moniliasis'''.
| |
|
| |
|
| == Pathophysiology== | | ==[[Oral candidiasis pathophysiology|Pathophysiology]]== |
| Candida albicans and C. glabrata. Less commonly, C.tropicalis, C. parapsilosis, and C. krusei. Rarely, other Candida species. Most cases of OPC are caused by the person’s own Candida organisms which normally live in the mouth or digestive tract. A person has symptoms when overgrowth of Candida organisms occurs.
| |
|
| |
|
| Most infections are endogenous in origin, but organisms can be transmitted on the hands of care givers.
| | ==[[Oral candidiasis causes|Causes]]== |
|
| |
|
| == Epidemiology and Demographics == | | ==[[Oral candidiasis differential diagnosis|Differentiating Oral Candidiasis from other Diseases]]== |
|
| |
|
| Fourth most common cause of nosocomial bloodstream infections. Incidence is 8 cases per 100,000 in the general population. Higher incidence among neonates and African-Americans. OPC used to be a common opportunistic infection in HIV-infected persons (prior to the introduction of highly active antiretroviral therapy [[HAART]]).
| | ==[[Oral candidiasis epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| Nosocomial disease surveillance is conducted by NNIS in selected hospitals. Active population-based surveillance for candidemia is being conducted in selected U.S. sites.
| | ==[[Oral candidiasis risk factors|Risk Factors]]== |
|
| |
|
| ''Sequelae''
| | ==[[Oral candidiasis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
| None with appropriate antifungal therapy. Mortality rate is almost 50% with bloodstream and disseminated infection.
| |
| | |
| ==Risk Factors==
| |
| | |
| Invasive disease occurs in critically ill patients in intensive-care units, in persons with severe granulocytopenia, and in hematopoietic stem cell and organ transplant recipients. OPC can be associated with HIV infection. VVC is often associated with pregnancy, diabetes mellitus, and antibiotic therapy.
| |
| | |
| ===Who is at special risk?===
| |
| * [[Newborn]] babies.
| |
| * Denture users.
| |
| * Poorly controlled [[diabetes]].
| |
| * As a side effect of medication, most commonly having taken [[antibiotic]]s. Inhaled [[corticosteroid]]s for treatment of lung conditions (e.g, [[Asthma]] or [[COPD]]) may also result in oral candidiasis which may be reduced by regularly rinsing the mouth with water after taking the medication.
| |
| * People with poor [[nutrition]], specifically vitamin A, iron and folate deficiencies.
| |
| * People with an [[immune deficiency]] (e.g. as a result of [[AIDS]]/[[HIV]] or [[chemotherapy]] treatment).
| |
| * Women undergoing hormonal changes, like pregnancy or those on birth control pills
| |
| * People who perform cunnilingus or fellatio on a sexual partner who has [[thrush]].
| |
| | |
| ===Thrush and Breastfeeding=== | |
| Because of the increased use of antibiotics in laboring women to reduce the transmission of [[Group B streptococcal infection]] to the infant, thrush has become more prevalent. Symptoms include:
| |
| * An oral rash in the infant's mouth
| |
| * A diaper rash that does not heal with conventional diaper rash treatments and ointments,
| |
| * Burning, painful nipples for the breastfeeding mother.
| |
| The rash and pain experienced by the mother can range from severe to mild and may complicate [[breastfeeding]]. Because thrush is assumed to be benign, it may be difficult to obtain treatment for an outbreak in the diaper area of an infant or mother's nipples. Over the counter yeast infection cream, that comes in the 7-day package, can be applied to the skin with good results within 24 - 48 hours. It should be washed off nipples before breastfeeding.
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| ===Symptoms===
| |
| Adults may experience discomfort or burning in the mouth. Symptoms of candidiasis in the esophagus may include pain and [[dysphagia]] ([[difficult swallowing]]).
| |
|
| |
| In babies the condition is termed thrush and is usually painless and causes no discomfort.
| |
|
| |
| ===Physical Examination===
| |
| Oral infections of candidia usually appear as thick white or cream-colour deposits. Underlying the deposits the mucosa of the mouth may appear inflamed (red and possibly slightly raised). Oral lesions are painless, white patches in the mouth.
| |
|
| |
| <div align="center">
| |
| <gallery heights="175" widths="175">
| |
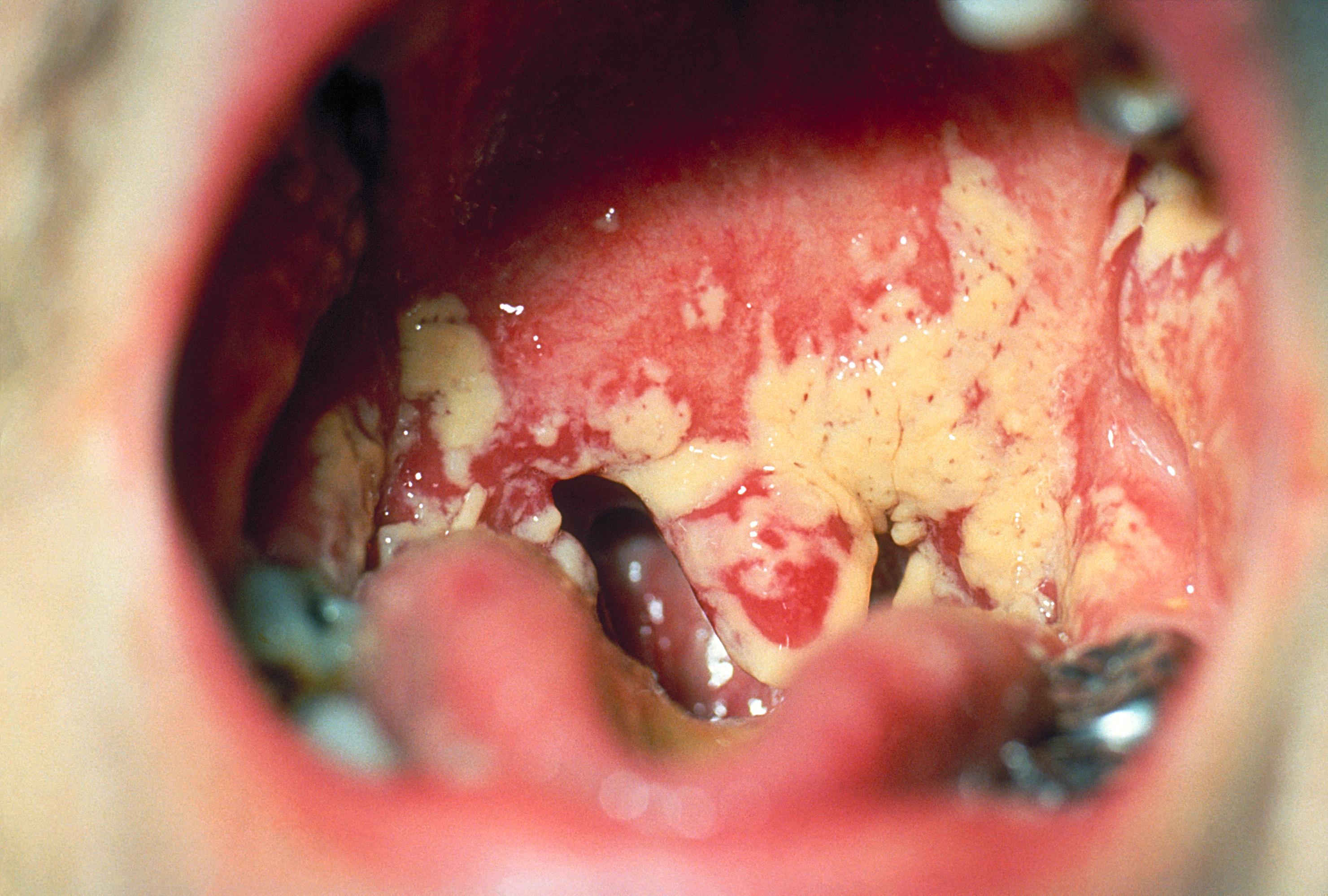
| Image:Oralcandi.JPG|Oral candidiasis on the [[tongue]] and soft [[palate]].
| |
| Image:Oral candidiasis.jpg|Oral manifestations of HIV infection and AIDS. Chronic oral candidiasis in patient with AIDS. <small>Image courtesy of Professor Peter Anderson DVM PhD and published with permission. [http://www.peir.net © PEIR, University of Alabama at Birmingham, Department of Pathology] </small>
| |
| Image:Oral candidiasis 2.jpg|Soft palate showing extensive oral candidiasis in patient with AIDS. <small>Image courtesy of Professor Peter Anderson DVM PhD and published with permission. [http://www.peir.net © PEIR, University of Alabama at Birmingham, Department of Pathology] </small>
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| ===Laboratory Studies===
| | [[Oral candidiasis history and symptoms|History and Symptoms]] | [[Oral candidiasis physical examination|Physical Examination]] | [[Oral candidiasis laboratory findings|Laboratory Findings]] | [[Oral candidiasis other diagnostic studies|Other Diagnostic Studies]] |
| [[Image:Candida albicans .jpg|left|thumb|250px|Agar plate culture of Candida albicans]] | |
| {{Clr}}
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
|
| |
|
| Any underlying cause, such as poor glucose control in diabetics, should be addressed. Oral candidiasis can be treated with topical [[anti-fungal]] drugs, such as [[nystatin]] (mycostatin), [[miconazole]] or [[amphotericin B]]. Patients who are immunocompromised, either with HIV/AIDS or as a result of chemotherapy, may require systemic treatment with oral or intravenous administered anti-fungals.
| | [[Oral candidiasis medical therapy|Medical Therapy]] | [[Oral candidiasis primary prevention|Primary Prevention]] | [[Oral candidiasis secondary prevention|Secondary Prevention]] | [[Oral candidiasis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Oral candidiasis future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| For adults, mild cases can be first treated by drinking acidic substances, such as orange juice, to make a harsher environment for the yeast and eating yogurt to replenish bacterial count that controls the yeast. If home treatment is not effective a physician may need to be consulted.
| | ==Case Studies== |
|
| |
|
| ==References==
| | [[Oral candidiasis case study one|Case #1]] |
| {{Reflist|2}}
| |
|
| |
|
| ==See Also== | | ==Related Chapters== |
|
| |
|
| * [[Candida albicans]] | | * [[Candida albicans]] |
| Line 96: |
Line 45: |
|
| |
|
| {{Mycoses}} | | {{Mycoses}} |
|
| |
|
| |
|
| [[da:Trøske (infektion)]] | | [[da:Trøske (infektion)]] |
| [[it:Mughetto (malattia)]] | | [[it:Mughetto (malattia)]] |
|
| |
|
| | {{WikiDoc Help Menu}} |
| | {{WikiDoc Sources}} |
| | |
| | [[Category:Disease]] |
| [[Category:Fungal diseases]] | | [[Category:Fungal diseases]] |
| [[Category:Gastroenterology]] | | [[Category:Gastroenterology]] |
| | [[Category:Emergency mdicine]] |
| | [[Category:Up-To-Date]] |
| [[Category:Infectious disease]] | | [[Category:Infectious disease]] |
| [[Category:Overview complete]] | | [[Category:Otolaryngology]] |
| [[Category:Signs and symptoms]] | | [[Category:Pediatrics]] |
| | | [[Category:Immunology]] |
| {{WikiDoc Help Menu}}
| |
| {{WikiDoc Sources}}
| |