Mitral regurgitation echocardiography: Difference between revisions
No edit summary |
|||
| Line 6: | Line 6: | ||
==Determination of the Underlying Cause of Mitral Regurgitation on Echocardiography== | ==Determination of the Underlying Cause of Mitral Regurgitation on Echocardiography== | ||
===Mitral Valve Prolapse / Myxomatous Mitral Valve=== | |||
Mitral valve prolapse is now the most common cause of mitral regurgitation in the Western world. Echocardiography in MVP demonstrates thick and redundant leaflets and chordae. The echocardiographic criteria for the diagnosis of MVP include: | |||
:#Movement of any part of either leaflet more than 2 mm behind the annular plane in parasternal long axis view and | |||
:#Movement of the point of co-aptation behind the annular plane in the apical 4 chamber view | |||
Over time, the poor tensile strength of the chordae leads to their progressive elongation and / or rupture. Ruptured chordae appear as flail segments. | |||
===Rheumatic Mitral Regurgitation=== | ===Rheumatic Mitral Regurgitation=== | ||
In '''rheumatic mitral regurgitation''', there is some degree of commissural fusion and thickening of the tips visible in 2 dimensional echocardiography. The movement of the valve leaflets is restricted. | In '''rheumatic mitral regurgitation''', there is some degree of commissural fusion and thickening of the tips visible in 2 dimensional echocardiography. The movement of the valve leaflets is restricted. | ||
===Annular Calcification=== | ===Annular Calcification=== | ||
| Line 25: | Line 30: | ||
Functional MR results due to LV dilatation and systolic dysfunction in those with a structurally normal [[mitral valve]] apparatus. | Functional MR results due to LV dilatation and systolic dysfunction in those with a structurally normal [[mitral valve]] apparatus. | ||
==Echocardiographic Monitoring== | ==Echocardiographic Monitoring== | ||
The 2006 [[ACC]]/[[AHA]] guidelines included recommendations for echocardiographic monitoring in asymptomatic patients with chronic MR <ref name="pmid18820172">{{cite journal| author=Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD et al.| title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. | journal=Circulation | year= 2008 | volume= 118 | issue= 15 | pages= e523-661 | pmid=18820172| doi=10.1161/CIRCULATIONAHA.108.190748 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18820172 }} </ref>. Echocardiography is performed to assess the left ventricular ejection fraction and end-systolic dimension. | The 2006 [[ACC]]/[[AHA]] guidelines included recommendations for echocardiographic monitoring in asymptomatic patients with chronic MR <ref name="pmid18820172">{{cite journal| author=Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD et al.| title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. | journal=Circulation | year= 2008 | volume= 118 | issue= 15 | pages= e523-661 | pmid=18820172| doi=10.1161/CIRCULATIONAHA.108.190748 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18820172 }} </ref>. Echocardiography is performed to assess the left ventricular ejection fraction and end-systolic dimension. | ||
Revision as of 22:42, 15 April 2012
|
Mitral Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mitral regurgitation echocardiography On the Web |
|
American Roentgen Ray Society Images of Mitral regurgitation echocardiography |
|
Risk calculators and risk factors for Mitral regurgitation echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.'; Mohammed A. Sbeih, M.D.[3]
Overview
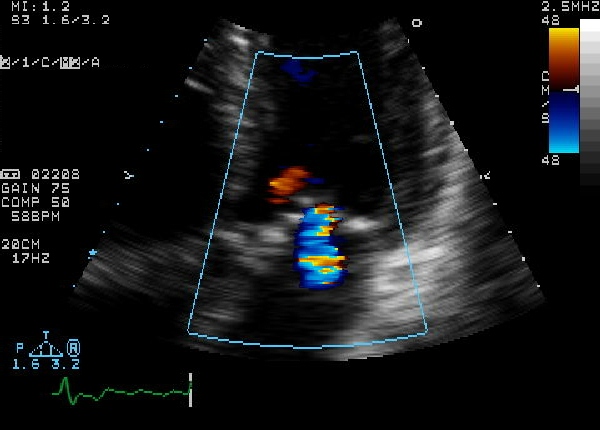
Transthoracic echocardiography should be performed in a patient with suspected mitral regurgitation to confirm the diagnosis and to establish the baseline severity of disease. It should then be performed to monitor the course of disease over time. Color doppler flow on the transthoracic echocardiogram (TTE) will reveal a jet of blood flowing from the left ventricle into the left atrium during ventricular systole. Echocardiographic features that suggest severe mitral regurgitation include systolic reversal of flow in the pulmonary veins and filling of the entire left atrial cavity by the regurgitant jet of MR.
Determination of the Underlying Cause of Mitral Regurgitation on Echocardiography
Mitral Valve Prolapse / Myxomatous Mitral Valve
Mitral valve prolapse is now the most common cause of mitral regurgitation in the Western world. Echocardiography in MVP demonstrates thick and redundant leaflets and chordae. The echocardiographic criteria for the diagnosis of MVP include:
- Movement of any part of either leaflet more than 2 mm behind the annular plane in parasternal long axis view and
- Movement of the point of co-aptation behind the annular plane in the apical 4 chamber view
Over time, the poor tensile strength of the chordae leads to their progressive elongation and / or rupture. Ruptured chordae appear as flail segments.
Rheumatic Mitral Regurgitation
In rheumatic mitral regurgitation, there is some degree of commissural fusion and thickening of the tips visible in 2 dimensional echocardiography. The movement of the valve leaflets is restricted.
Annular Calcification
Mitral annulus is usually smaller in systole. The increased rigidity due to annular calcification impairs contraction. In 2D- echocardiography, there is increased echogenicity on the LV side immediately adjacent to the attachment of the posterior mitral valve leaflet. Region of anterior mitral leaflet is only rarely involved. This is common in elderly subjects and younger ones with chronic renal failure and hypertension.
Ischaemic Mitral Regurgitation
Mitral regurgitation can occur in ischemia as a result of regional left ventricular dysfunction with abnormal contraction of papillary muscle or underlying ventricular wall. Myocardial infarction can result in MR at rest while if the underlying cause is ischemia the MR may be intermittent. The echocardiogram is characterized by restricted valve leaflet motion and tenting of mitral valve in systole.
Papillary Muscle Rupture
This is usually a complication of myocardial infarction. If entire papillary muscle is disconnected from the left ventricle severe MR results and few survive. Partial rupture is more common.
Functional Mitral Regurgitation
Functional MR results due to LV dilatation and systolic dysfunction in those with a structurally normal mitral valve apparatus.
Echocardiographic Monitoring
The 2006 ACC/AHA guidelines included recommendations for echocardiographic monitoring in asymptomatic patients with chronic MR [1]. Echocardiography is performed to assess the left ventricular ejection fraction and end-systolic dimension.
| Degree of mitral regurgitation | Regurgitant fraction | Regurgitant Orifice area |
|---|---|---|
| Mild mitral regurgitation | < 20 percent | |
| Moderate mitral regurgitation | 20 - 40 percent | |
| Moderate to severe mitral regurgitation | 40 - 60 percent | |
| Severe mitral regurgitation | > 60 percent | > 0.3 cm2 |
Assessment of Severity of Mitral Regurgitation
The degree of severity of mitral regurgitation can be quantified by the percentage of the left ventricular stroke volume that regurgitates into the left atrium (the regurgitant fraction).
Methods that have been used to assess the regurgitant fraction in mitral regurgitation include:
- Echocardiography.
- Cardiac catheterization.
- Fast CT scan.
- Cardiac MRI.
The echocardiographic technique to measure the regurgitant fraction is to determine the forward flow through the mitral valve (from the left atrium to the left ventricle) during ventricular diastole, and comparing it with the flow out of the left ventricle through the aortic valve in ventricular systole.
This method assumes that the aortic valve does not suffer from aortic insufficiency. The regurgitant fraction would be described as:
Another way to quantify the degree of mitral regurgitation is to determine the area of the regurgitant flow at the level of the valve. This is known as the regurgitant orifice area, and correlates with the size of the defect in the mitral valve.
One particular echocardiographic technique used to measure the orifice area is measurement of the proximal isovelocity surface area (PISA). The flaw of using PISA to determine the mitral valve regurgitant orifice area is that it measures the flow at one moment in time in the cardiac cycle, which may not reflect the average performance of the regurgitant jet.
Colour Flow Mapping
- Size of flow recruitment is noted.
- Jet base width at the valve level.
- Intra atrial jet area if it is a central jet.
- Jet direction is usually away from a prolapsing leaflet and behind a restricted leaflet.
Continuous Wave Doppler
- Shape and density of signal - In severe Mitral regurgitation, the flow is dense and triangular.
- If as dense as forward flow, it is severe.
Pulse Wave Doppler(PW)
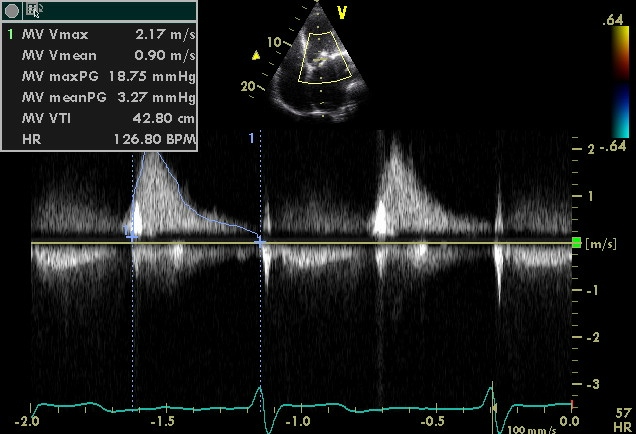
- PW in apical-4-chamber view.
- E wave more than 1.2m/s indicates severe MR.
- Even minor mitral stenosis or hyperdynamic circulation can increase E wave.
- If A-wave dominant, severe MR is virtually ruled out.
Vena Contracta
- vena contracta is the narrowest region of regurgitant jet (usually just below the valve in LA).
- >0.7 cm - severe MR.
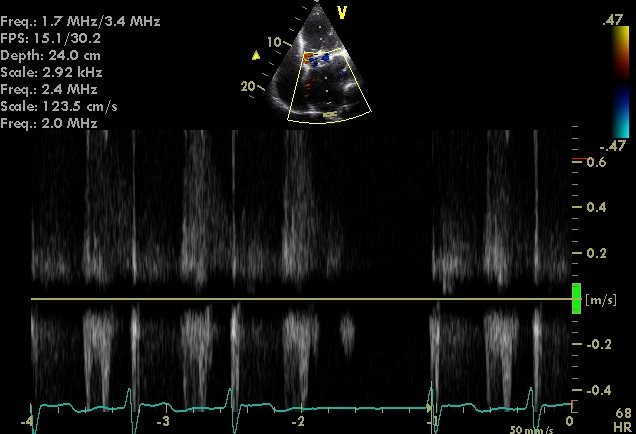
Pulmonary Venous Flow
- Usually forward throughout cycle.
- Systolic dominant.
- As MR worsens, there is a blunting of systolic flow.
- If severe MR - systolic flow reversal.
Regurgitant Volume
- Mitral regurgitant volume = Mitral inflow volume - LV outflow volume.
- Mitral inflow volume = Vti * Cross sectional area of mitral valve.
- LV outflow volume = Vti * Cross sectional area at LV outflow.
- Regurtitant volume - <20% - mild , >50% severe
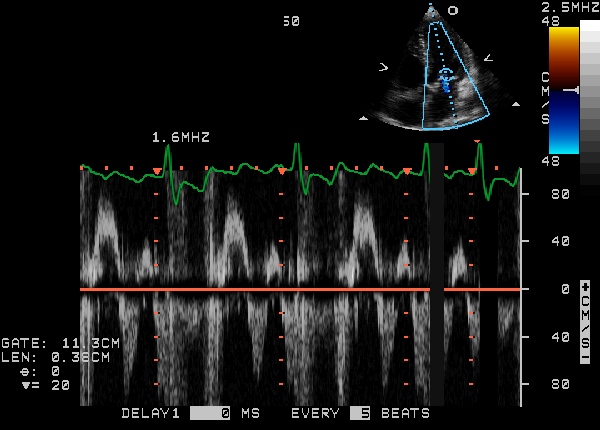
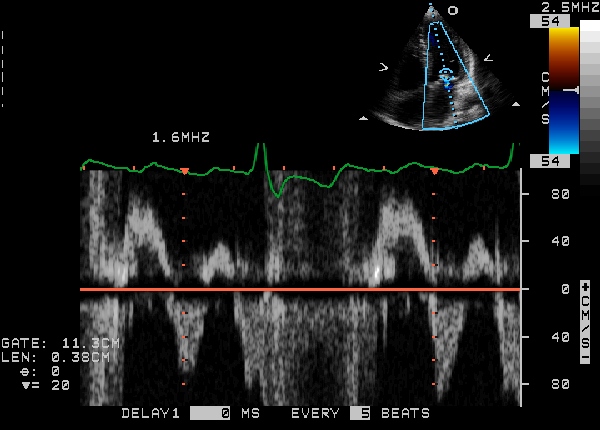
PISA (Proximal Isovelocity Surface Area)
The radius of Proximal isovelocity surface area or flow convergence zone which is a 3-dimensional surface area proximal to a narrowed orifice at which all the blood velocities are equal, can be used to calculate the severity of mitral regurgitation. The principle is that if the mitral regurgitation is mild, only the blood nearer to the valve orifice accelerates towards the atrium while in severe regurgitation, blood farther away from the valve moves back.
PISA radius
A simple method to determine severity of mitral regurgitation is to measure the PISA radius. Regurgitation is mild if radius is <0.4 cm and severe if >1 cm.
Regurgitant Flow (Instantaneous)
The instantaneous regurgitant flow can be calculated from the PISA radius and can be used to assess the severity of mitral regurgitation.
Regurgitant flow = 2π * r2 * Valiasing
Effective Regurgitant Orifice Area (EROA)
Effective regurgitant orifice area can be calculated using the instantaneous regurgitant flow. The formula can be derived from the following:
Valiasing * 2πr2 = Vmax * EROA
hence:
- EROA = PISA (2πr2) * Valiasing / Vmax
Mild = 0-20 cm2, moderate = 20 - 40 cm2, severe = >40 cm2
Regurgitant volume can be calculated from this.
- Regurgitant volume = Effective regurgitant orifice area * Vtime integrale
Diastolic Mitral Regurgitation Secondary to Severe Aortic Stenosis
<youtube v=wzYVcqVLspw/> <googlevideo>424719160215823743&hl=en</googlevideo>
<googlevideo>-1316686479831791521&hl=en</googlevideo>
Severity (Summary)
| Severity | mild | severe |
|---|---|---|
| Jet area | <4 cm2 | >8 cm2 |
| Jet width | thin | >0.6 |
| vena contracta | <0.3 | >0.7 |
| PISA radius | <0.4 | >1 |
| Pulmonary venous flow | systolic dominant | systolic flow reversal |
| Mitral inflow | can be A wave dominant | E wave dominant >1.2m/s |
| Continuous wave doppler | soft and parabolic | dense and triangular |
| LV and LA | normal size | enlarged (in chronic MR) |
| duration | can be short | holosystolic |
| Regurgitant volume | <30 ml | >60 ml |
| EROA | 0-20 cm2 | >40 cm2 |
ACC/AHA Guidelines- Indications for Transthoracic Echocardiography (DO NOT EDIT) [2]
| “ |
Class I1. Transthoracic echocardiography is indicated for baseline evaluation of LV size and function, RV and left atrial size, pulmonary artery pressure, and severity of MR (Table 4) in any patient suspected of having MR. (Level of Evidence: C) 2. Transthoracic echocardiography is indicated for delineation of the mechanism of MR. (Level of Evidence: B) 3. Transthoracic echocardiography is indicated for annual or semiannual surveillance of LV function (estimated by ejection fraction and end-systolic dimension) in asymptomatic patients with moderate to severe MR. (Level of Evidence: C) 4. Transthoracic echocardiography is indicated in patients with MR to evaluate the MV apparatus and LV function after a change in signs or symptoms. (Level of Evidence: C) 5. Transthoracic echocardiography is indicated to evaluate LV size and function and MV hemodynamics in the initial evaluation after MV replacement or MV repair. (Level of Evidence: C) Class IIa1. Exercise Doppler echocardiography is reasonable in asymptomatic patients with severe MR to assess exercise tolerance and the effects of exercise on pulmonary artery pressure and MR severity. (Level of Evidence: C) Class III1. Transthoracic echocardiography is not indicated for routine follow-up evaluation of asymptomatic patients with mild MR and normal LV size and systolic function. (Level of Evidence: C) |
” |
ACC/AHA Guidelines- Indications for Transesophageal Echocardiography (DO NOT EDIT) [2]
| “ |
Class I1. Preoperative or intraoperative transesophageal echocardiography is indicated to establish the anatomic basis for severe MR in patients in whom surgery is recommended to assess feasibility of repair and to guide repair. (Level of Evidence: B) 2. Transesophageal echocardiography is indicated for evaluation of MR patients in whom transthoracic echocardiography provides nondiagnostic information regarding severity of MR, mechanism of MR, and/or status of LV function. (Level of Evidence: B) Class IIa1. Preoperative transesophageal echocardiography is reasonable in asymptomatic patients with severe MR who are considered for surgery to assess feasibility of repair. (Level of Evidence: C) Class III1. Transesophageal echocardiography is not indicated for routine follow-up or surveillance of asymptomatic patients with native valve MR. (Level of Evidence: C) |
” |
 |
- Mitral Ring Dehiscence Post Repair With Severe Mitral Regurgitation
{{#ev:googlevideo|7246533519972889950&hl=en}}
- Severe Mitral Regurgitation From Ring Dehiscence Pulmonary Vein Pulsed Wave Doppler
- Severe Mitral Regurgitation Pulmonary Vein Pulsed Wave Doppler
Sources
- 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease [2].
References
- ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172.
- ↑ 2.0 2.1 2.2 Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". J Am Coll Cardiol. 52 (13): e1–142. doi:10.1016/j.jacc.2008.05.007. PMID 18848134.