Lymphoplasmacytic lymphoma other diagnostic studies: Difference between revisions
Sara Mohsin (talk | contribs) |
|||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Other [[diagnostic]] | Other [[Diagnostic study of choice|diagnostic studies]] for [[lymphoplasmacytic lymphoma]] include [[nerve conduction study]], [[electromyography]], [[Fundoscopy|funduscopy]], [[Viscosity|plasma viscosity]], and [[Mutation|mutational]] [[analysis]]. | ||
==Other Diagnostic Studies== | ==Other Diagnostic Studies== | ||
Other [[diagnostic]] | Other [[Diagnostic study of choice|diagnostic studies]] for [[lymphoplasmacytic lymphoma]] include: | ||
*'''[[Nerve conduction study|Nerve conduction study]]''' and '''[[electromyography]]''', which demonstrates:<ref name="ser">{{cite journal |vauthors=Nobile-Orazio E, Marmiroli P, Baldini L, Spagnol G, Barbieri S, Moggio M, Polli N, Polli E, Scarlato G |title=Peripheral neuropathy in macroglobulinemia: incidence and antigen-specificity of M proteins |journal=Neurology |volume=37 |issue=9 |pages=1506–14 |year=1987 |pmid=2442666 |doi= |url=}}</ref> | *'''[[Nerve conduction study|Nerve conduction study]]''' and '''[[electromyography]]''', which demonstrates:<ref name="ser">{{cite journal |vauthors=Nobile-Orazio E, Marmiroli P, Baldini L, Spagnol G, Barbieri S, Moggio M, Polli N, Polli E, Scarlato G |title=Peripheral neuropathy in macroglobulinemia: incidence and antigen-specificity of M proteins |journal=Neurology |volume=37 |issue=9 |pages=1506–14 |year=1987 |pmid=2442666 |doi= |url=}}</ref> | ||
**[[Demyelination]] with [[sensory]] involvement more than [[Motor control|motor]]. | **[[Demyelination]] with [[sensory]] involvement more than [[Motor control|motor]]. | ||
*'''[[Fundoscopy]]''', which demonstrates:<ref name="pmid27378193">{{cite journal| author=Castillo JJ, Garcia-Sanz R, Hatjiharissi E, Kyle RA, Leleu X, McMaster M et al.| title=Recommendations for the diagnosis and initial evaluation of patients with Waldenström Macroglobulinaemia: A Task Force from the 8th International Workshop on Waldenström Macroglobulinaemia. | journal=Br J Haematol | year= 2016 | volume= 175 | issue= 1 | pages= 77-86 | pmid=27378193 | doi=10.1111/bjh.14196 | pmc=5154335 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27378193 }} </ref> | *'''[[Fundoscopy]]''', which demonstrates:<ref name="pmid27378193">{{cite journal| author=Castillo JJ, Garcia-Sanz R, Hatjiharissi E, Kyle RA, Leleu X, McMaster M et al.| title=Recommendations for the diagnosis and initial evaluation of patients with Waldenström Macroglobulinaemia: A Task Force from the 8th International Workshop on Waldenström Macroglobulinaemia. | journal=Br J Haematol | year= 2016 | volume= 175 | issue= 1 | pages= 77-86 | pmid=27378193 | doi=10.1111/bjh.14196 | pmc=5154335 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27378193 }} </ref> | ||
**Dilated, segmented, and tortuous [[retinal veins]] giving a "sausage link" appearance | **[[Dilate|Dilated]], [[Segment (linguistics)|segmented]], and [[tortuous]] [[retinal veins]] giving a "sausage [[link]]" [[appearance]] | ||
**Useful in patients with suspected [[hyperviscosity syndrome]] | **Useful in [[patients]] with suspected [[hyperviscosity syndrome]] | ||
{| | {| | ||
| | | | ||
[[File:Retinal veins dilation gif.gif|thumb|300px|none|Ophthalmoscopic examination revealed dilatation and tortuosity of the retinal veins.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3102879_jkms-26-824-g004&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=43 Source: Kim YL. et al, Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea.]]] | [[File:Retinal veins dilation gif.gif|thumb|300px|none|[[Ophthalmoscope|Ophthalmoscopic]] examination revealed dilatation and tortuosity of the retinal veins. [https://openi.nlm.nih.gov/detailedresult.php?img=PMC3102879_jkms-26-824-g004&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=43 Source: Kim YL. et al, Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea.]]] | ||
| | | | ||
[[File:Retinal vein gif.gif|thumb|300px|none|Ophthalmologic findings in the presented case. Optic disk of the left eye is shown. | [[File:Retinal vein gif.gif|thumb|300px|none|Ophthalmologic findings in the presented case. The [[Optic disc|optic disk]] of the left eye is shown. The perivenous sheathing is indicated (black arrow). [https://openi.nlm.nih.gov/detailedresult.php?img=PMC4163423_CRIONM2014-165670.002&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=30 Source: Nipp R. et al, Dana-Farber Cancer Institute, 450 Brookline Avenue, Boston, MA 02215, USA.]]] | ||
|- | |- | ||
| | | | ||
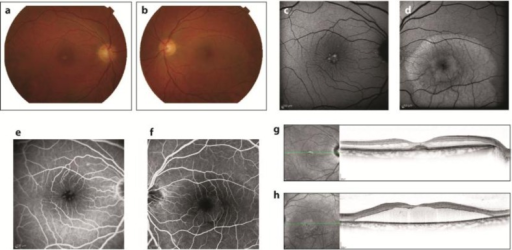
[[File:After therapy.png|thumb|300px|none| One year after therapy. The right fundus exhibited a roundish, subretinal, pseudovitelliform deposit (a). The deposit displayed uneven hyper-autofluorescence on a fundus | [[File:After therapy.png|thumb|300px|none| One year after therapy. The right fundus exhibited a roundish, subretinal, pseudovitelliform deposit (a). The deposit displayed uneven hyper-autofluorescence on a fundus autofluorescence photograph (c) and uneven staining in [[fluorescein angiography]] (e). It was associated with [[macular edema]] in an OCT horizontal scan (g). The left eye fundus exhibited a large retinal serous detachment (b), with accumulation of hyper-autofluorescent lipofuscin material in autofluorescence fundus photography (d). Fluorescein angiography was not contributive (f), but OCT showed the absence of central photoreceptors (h).[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3433005_cop-0003-0236-g02&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=27 Source: Brolly A. et al, Department of Ophthalmology, APHP, Hôpital Lariboisière, University Paris Diderot, Sorbonne Paris Cité, Bourges, France.]]] | ||
| | | | ||
[[File:Flor angiography gif.gif|thumb|500px|none| Fluorescein angiography: Hyperviscosity syndrome characterized by bilateral retinal venous dilation and tortuosity, retinal hemorrhages and peripheral | [[File:Flor angiography gif.gif|thumb|500px|none| [[Fluorescein angiography]]: Hyperviscosity syndrome characterized by bilateral retinal venous dilation and tortuosity, retinal hemorrhages and peripheral microaneurysms.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3433005_cop-0003-0236-g01&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=26 Source: Brolly A. et al, Department of Ophthalmology, APHP, Hôpital Lariboisière, University Paris Diderot, Sorbonne Paris Cité, Bourges, France.]]] | ||
|} | |} | ||
* '''[[Plasma]] [[viscosity]]''', which demonstrates:<ref name="pmid4014299">{{cite journal| author=Crawford J, Cox EB, Cohen HJ| title=Evaluation of hyperviscosity in monoclonal gammopathies. | journal=Am J Med | year= 1985 | volume= 79 | issue= 1 | pages= 13-22 | pmid=4014299 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4014299 }} </ref> | * '''[[Plasma]] [[viscosity]]''', which demonstrates:<ref name="pmid4014299">{{cite journal| author=Crawford J, Cox EB, Cohen HJ| title=Evaluation of hyperviscosity in monoclonal gammopathies. | journal=Am J Med | year= 1985 | volume= 79 | issue= 1 | pages= 13-22 | pmid=4014299 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4014299 }} </ref> | ||
**Values > 1.5 centipoise | **[[Value (mathematics)|Values]] > 1.5 centipoise: | ||
***Should be measured in patients presenting with [[signs]] | ***Should be [[Measure (mathematics)|measured]] in [[patients]] [[Presenting symptom|presenting]] with [[Signs and Symptoms|signs and symptoms]] [[Suggestion|suggestive]] of [[hyperviscosity syndrome]] or whenever the [[Monoclonal antibodies|monoclonal]] [[Immunoglobulin M|IgM]] [[protein]] spike is > 4 g/dL. | ||
* '''Mutational analysis''' for the ''[[MYD88]]'' [[gene]], since the [[MYD88]] L265P [[mutation]] is found in 90% of patients with [[lymphoplasmacytic lymphoma]].<ref name="pmid23321251">{{cite journal| author=Xu L, Hunter ZR, Yang G, Zhou Y, Cao Y, Liu X et al.| title=MYD88 L265P in Waldenström macroglobulinemia, immunoglobulin M monoclonal gammopathy, and other B-cell lymphoproliferative disorders using conventional and quantitative allele-specific polymerase chain reaction. | journal=Blood | year= 2013 | volume= 121 | issue= 11 | pages= 2051-8 | pmid=23321251 | doi=10.1182/blood-2012-09-454355 | pmc=3596964 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23321251 }} </ref> | * '''[[Mutation|Mutational]] [[analysis]]''' for the ''[[MYD88]]'' [[gene]], since the [[MYD88]] L265P [[mutation]] is found in 90% of [[patients]] with [[lymphoplasmacytic lymphoma]].<ref name="pmid23321251">{{cite journal| author=Xu L, Hunter ZR, Yang G, Zhou Y, Cao Y, Liu X et al.| title=MYD88 L265P in Waldenström macroglobulinemia, immunoglobulin M monoclonal gammopathy, and other B-cell lymphoproliferative disorders using conventional and quantitative allele-specific polymerase chain reaction. | journal=Blood | year= 2013 | volume= 121 | issue= 11 | pages= 2051-8 | pmid=23321251 | doi=10.1182/blood-2012-09-454355 | pmc=3596964 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23321251 }} </ref> | ||
*In patients with [[peripheral neuropathy]], other causes of [[neuropathy]] should be ruled out by performing respective tests (as required) for: | *In [[patients]] with [[peripheral neuropathy]], other [[causes]] of [[neuropathy]] should be ruled out by [[Performance status|performing]] respective [[Test|tests]] (as required) for: | ||
**[[Diabetes]] | **[[Diabetes]] | ||
**[[Cobalamin]] | **[[Cobalamin]] | ||
**([[Vitamin B12]]) deficiency | **([[Vitamin B12]]) [[deficiency]] | ||
**[[Thyroid]] [[dysfunction]] | **[[Thyroid]] [[dysfunction]] | ||
**[[Lyme disease]] | **[[Lyme disease]] | ||
| Line 40: | Line 40: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category: | [[Category:Disease]] | ||
[[Category:Blood]] | |||
[[Category:Hematology]] | |||
Latest revision as of 13:39, 30 October 2019
|
Lymphoplasmacytic lymphoma Microchapters |
|
Differentiating Lymphoplasmacytic Lymphoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Lymphoplasmacytic lymphoma other diagnostic studies On the Web |
|
American Roentgen Ray Society Images of Lymphoplasmacytic lymphoma other diagnostic studies |
|
Lymphoplasmacytic lymphoma other diagnostic studies in the news |
|
Blogs on Lymphoplasmacytic lymphoma other diagnostic studies |
|
Risk calculators and risk factors for Lymphoplasmacytic lymphoma other diagnostic studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Overview
Other diagnostic studies for lymphoplasmacytic lymphoma include nerve conduction study, electromyography, funduscopy, plasma viscosity, and mutational analysis.
Other Diagnostic Studies
Other diagnostic studies for lymphoplasmacytic lymphoma include:
- Nerve conduction study and electromyography, which demonstrates:[1]
- Demyelination with sensory involvement more than motor.
- Fundoscopy, which demonstrates:[2]
- Dilated, segmented, and tortuous retinal veins giving a "sausage link" appearance
- Useful in patients with suspected hyperviscosity syndrome
 |
 |
 |
 |
- Plasma viscosity, which demonstrates:[3]
- Values > 1.5 centipoise:
- Should be measured in patients presenting with signs and symptoms suggestive of hyperviscosity syndrome or whenever the monoclonal IgM protein spike is > 4 g/dL.
- Values > 1.5 centipoise:
- Mutational analysis for the MYD88 gene, since the MYD88 L265P mutation is found in 90% of patients with lymphoplasmacytic lymphoma.[4]
- In patients with peripheral neuropathy, other causes of neuropathy should be ruled out by performing respective tests (as required) for:
References
- ↑ Nobile-Orazio E, Marmiroli P, Baldini L, Spagnol G, Barbieri S, Moggio M, Polli N, Polli E, Scarlato G (1987). "Peripheral neuropathy in macroglobulinemia: incidence and antigen-specificity of M proteins". Neurology. 37 (9): 1506–14. PMID 2442666.
- ↑ Castillo JJ, Garcia-Sanz R, Hatjiharissi E, Kyle RA, Leleu X, McMaster M; et al. (2016). "Recommendations for the diagnosis and initial evaluation of patients with Waldenström Macroglobulinaemia: A Task Force from the 8th International Workshop on Waldenström Macroglobulinaemia". Br J Haematol. 175 (1): 77–86. doi:10.1111/bjh.14196. PMC 5154335. PMID 27378193.
- ↑ Crawford J, Cox EB, Cohen HJ (1985). "Evaluation of hyperviscosity in monoclonal gammopathies". Am J Med. 79 (1): 13–22. PMID 4014299.
- ↑ Xu L, Hunter ZR, Yang G, Zhou Y, Cao Y, Liu X; et al. (2013). "MYD88 L265P in Waldenström macroglobulinemia, immunoglobulin M monoclonal gammopathy, and other B-cell lymphoproliferative disorders using conventional and quantitative allele-specific polymerase chain reaction". Blood. 121 (11): 2051–8. doi:10.1182/blood-2012-09-454355. PMC 3596964. PMID 23321251.