Leukemia: Difference between revisions
Ahmed Younes (talk | contribs) (→Gender) |
No edit summary |
||
| Line 9: | Line 9: | ||
==Overview== | ==Overview== | ||
'''Leukemia''' (Greek leukos, “white”; haima, “blood”) | '''Leukemia''' (Greek leukos, “white”; haima, “blood”) can be defined as a group of [[hematopoietic stem cell]] [[malignancies]] due to [[genetic]] abnormalities that may lead to clonal proliferation of these cells. These group of diseases are classified based on the type of [[hematopoietic stem cell]] involved and the duration of the disease. The leukemias are the most common malignancies among children younger than 15 years. Among them, [[ALL|Acute Lymphoblastic Leukemia (ALL)]] is the most common leukemia and accounts for 77% of childhood leukemia. However, [[CLL|Chronic Lymphocytic Leukemia (CLL)]] is the most common form of leukemia in adults, and it accounts for 30% of all leukemias in the United States. The increased rate of proliferation and decreased rate of [[apoptosis]] in this progeny of cells may compromise normal [[bone marrow]] function and ultimately result in marrow failure. Clinical manifestations, diagnosis, laboratory findings, and therapy are different according to the type of malignancy. | ||
==Classification== | ==Classification== | ||
| Line 25: | Line 25: | ||
==Differentiating Leukemia from other Diseases== | ==Differentiating Leukemia from other Diseases== | ||
Leukemia must be differentiated from various diseases that cause [[weight loss]], [[night sweats]], [[hepatosplenomegaly]], and palpable [[lymph node]]s, such as [[hairy cell leukaemia]], prolymphocytic | Leukemia must be differentiated from various diseases that cause [[weight loss]], [[night sweats]], [[hepatosplenomegaly]], and palpable [[lymph node]]s, such as [[hairy cell leukaemia|hairy cell leukemia]], prolymphocytic leukemia, [[follicular lymphoma]], and [[mantle cell lymphoma]]. Based on the expression of cell surface markers, the table below differentiates different types of leukemia from other diseases that cause similar clinical presentations:<ref name="H">Hoffbrand V, Moss P. Essential Haematology. John Wiley & Sons; 2011</ref> | ||
{| | {| | ||
| Line 201: | Line 201: | ||
* Progressive accumulation of monoclonal [[B cell|B lymphocytes]] | * Progressive accumulation of monoclonal [[B cell|B lymphocytes]] | ||
| align="left" style="background:#F5F5F5;" + | | | align="left" style="background:#F5F5F5;" + | | ||
* The most common leukemia in adults in | * The most common leukemia in adults in western countries | ||
* M > F | * M > F | ||
* Median age 70 years old | * Median age 70 years old | ||
| Line 251: | Line 251: | ||
* Median age 50 to 55 years old | * Median age 50 to 55 years old | ||
* M >> F | * M >> F | ||
* More in Caucasians than Blacks | * More common in Caucasians than Blacks | ||
| align="left" style="background:#F5F5F5;" + | | | align="left" style="background:#F5F5F5;" + | | ||
* Exposures to [[ionizing radiation]], [[Pesticide|pesticides]], and farming | * Exposures to [[ionizing radiation]], [[Pesticide|pesticides]], and farming | ||
| Line 390: | Line 390: | ||
===Incidence=== | ===Incidence=== | ||
* The delay-adjusted [[incidence]] of leukemia in 2011 was estimated | * The delay-adjusted [[incidence]] of leukemia in 2011 was estimated as 15.48 per 100,000 persons in the United States. | ||
* In 2011, the age-adjusted [[incidence]] of leukemia was 13.66 per 100,000 persons in the United States. | * In 2011, the age-adjusted [[incidence]] of leukemia was 13.66 per 100,000 persons in the United States. | ||
| Line 396: | Line 396: | ||
===Age=== | ===Age=== | ||
* The overall age-adjusted [[incidence]] of leukemia in the United States between 2007 and 2011 | * The overall age-adjusted [[incidence]] of leukemia in the United States between 2007 and 2011 was 13 per 100,000. The age-adjusted [[incidence]] of leukemia by age category is: | ||
** Under 65 years: 6.5 per 100,000 | ** Under 65 years: 6.5 per 100,000 | ||
** 65 and over: 57.9 per 100,000 | ** 65 and over: 57.9 per 100,000 | ||
| Line 415: | Line 415: | ||
===Gender=== | ===Gender=== | ||
* In the United States, the age-adjusted [[prevalence]] of leukemia by gender in 2011 | * In the United States, the age-adjusted [[prevalence]] of leukemia by gender in 2011 was: | ||
** In males: 92.7 per 100,000 | ** In males: 92.7 per 100,000 | ||
** In females: 60.7 per 100,000 | ** In females: 60.7 per 100,000 | ||
* In the United States, the delay-adjusted [[incidence]] of leukemia by gender in 2011 | * In the United States, the delay-adjusted [[incidence]] of leukemia by gender in 2011 was: | ||
** In males: 19.93 per 100,000 persons | ** In males: 19.93 per 100,000 persons | ||
** In females: 11.89 per 100,000 persons | ** In females: 11.89 per 100,000 persons | ||
* In the United States, the age-adjusted [[incidence]] of leukemia by gender on 2011 | * In the United States, the age-adjusted [[incidence]] of leukemia by gender on 2011 was: | ||
** In males: 17.58 per 100,000 persons | ** In males: 17.58 per 100,000 persons | ||
** In females: 10.49 per 100,000 persons | ** In females: 10.49 per 100,000 persons | ||
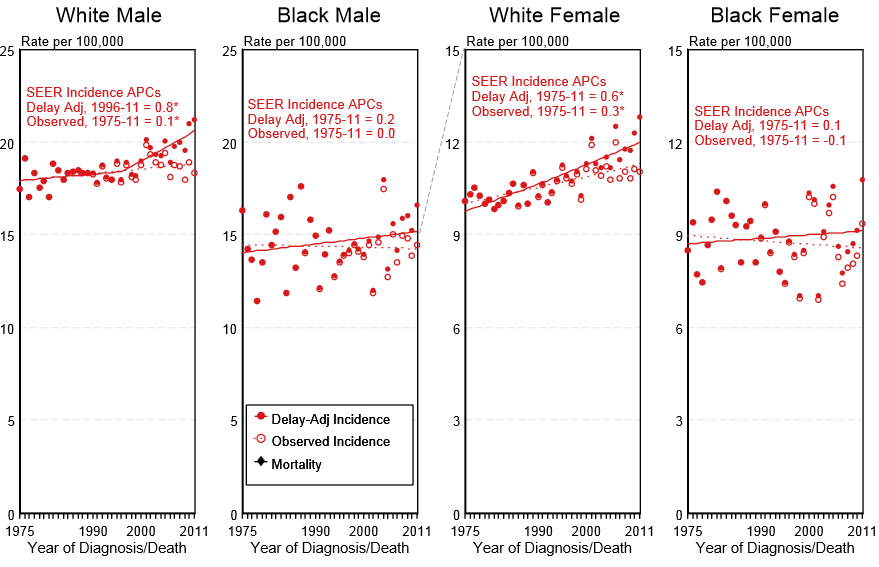
* Shown below is an image depicting the delay-adjusted [[incidence]] and observed [[incidence]] of leukemia by gender and race in the United States between 1975 and 2011. These graphs | * Shown below is an image depicting the delay-adjusted [[incidence]] and observed [[incidence]] of leukemia by gender and race in the United States between 1975 and 2011. These graphs were gathered from [[SEER]]: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. | ||
[[Image:Incidence of leukemia by gender and race in USA.PNG|700px|thumb|These graphs are adapted from [[SEER]]: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. - Delay-adjusted [[incidence]] and observed [[incidence]] of leukemia by gender and race in the United States between 1975 and 2011]] | [[Image:Incidence of leukemia by gender and race in USA.PNG|700px|thumb|These graphs are adapted from [[SEER]]: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute. - Delay-adjusted [[incidence]] and observed [[incidence]] of leukemia by gender and race in the United States between 1975 and 2011]] | ||
| Line 452: | Line 452: | ||
* Between 2004 and 2010, the 5-year relative survival of patients with leukemia was 60.3%. | * Between 2004 and 2010, the 5-year relative survival of patients with leukemia was 60.3%. | ||
* When stratified by age, the 5-year relative survival of patients with leukemia was 68.5% | * When stratified by age, the 5-year relative survival of patients with leukemia was 68.5% (44.1% for patients <65 and ≥ 65 years of age respectively). | ||
* Shown below is a table depicting the 5-year relative survival of patients by the type of leukemia in the United States between 2004 and 2010. | * Shown below is a table depicting the 5-year relative survival of patients by the type of leukemia in the United States between 2004 and 2010. | ||
Revision as of 16:16, 8 January 2019
|
Leukemia Microchapters |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2], Usama Talib, BSc, MD [3], Sadaf Sharfaei M.D.[4]
Synonyms and keywords: Leukaemia
Overview
Leukemia (Greek leukos, “white”; haima, “blood”) can be defined as a group of hematopoietic stem cell malignancies due to genetic abnormalities that may lead to clonal proliferation of these cells. These group of diseases are classified based on the type of hematopoietic stem cell involved and the duration of the disease. The leukemias are the most common malignancies among children younger than 15 years. Among them, Acute Lymphoblastic Leukemia (ALL) is the most common leukemia and accounts for 77% of childhood leukemia. However, Chronic Lymphocytic Leukemia (CLL) is the most common form of leukemia in adults, and it accounts for 30% of all leukemias in the United States. The increased rate of proliferation and decreased rate of apoptosis in this progeny of cells may compromise normal bone marrow function and ultimately result in marrow failure. Clinical manifestations, diagnosis, laboratory findings, and therapy are different according to the type of malignancy.
Classification
Leukemia may be classified as follows:
| Leukemia | |||||||||||||||||||||||||||||||||||||||
| Lymphoid progeny | Myeloid progeny | ||||||||||||||||||||||||||||||||||||||
| Acute lymphoblastic leukemia (ALL) | Chronic lymphocytic leukemia (CLL) | Acute Myeloid Leukemia (AML) | Chronic myeloid leukemia (CML) | ||||||||||||||||||||||||||||||||||||
Differentiating Leukemia from other Diseases
Leukemia must be differentiated from various diseases that cause weight loss, night sweats, hepatosplenomegaly, and palpable lymph nodes, such as hairy cell leukemia, prolymphocytic leukemia, follicular lymphoma, and mantle cell lymphoma. Based on the expression of cell surface markers, the table below differentiates different types of leukemia from other diseases that cause similar clinical presentations:[1]
| Disease | Etiology | Clinical Manifestation | Laboratory Findings | Gold standard diagnosis | Associated findings | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demography | History | Symptoms | Signs | ||||||||||||||
| Constitutional symptoms | Weight | Bleeding | Abdominal Pain | Vital sign | Jaundice | LAP | Hepatosplenomegaly | Other | CBC | Histopathology | Other | ||||||
| Acute myelogenous leukemia[2][3] |
|
|
|
↓ | + | – | – | Rare | Mild and asymptomatic |
|
|
|
| ||||
| Acute lymphoblastic leukemia[4][5] |
|
|
|
|
↓ | + | – | – | + | + |
|
|
|
| |||
| Chronic myelogenous leukemia[6][7] |
|
|
|
↓ | + | Abdominal fullness |
|
– | – | + |
|
|
|
|
| ||
| Disease | Etiology | Demography | History | Constitutional symptoms | Weight | Bleeding | Abdominal Pain | Vital sign | Jaundice | LAP | Hepatosplenomegaly | Other | CBC | Histopathology | Other | Gold standard diagnosis | Associated findings |
| Chronic lymphocytic leukemia[8] |
|
|
|
↓ | + | + | – | +
The most common abnormal finding |
+ |
|
|
|
|
| |||
| Hairy cell leukemia[9][10] |
|
|
↓ | + | Abdominal fullness |
|
– | ± | + |
|
|
|
|
||||
| Large granular lymphocytic leukemia[11][12] |
|
|
|
↓ | – | – | – | ± | + |
|
|
|
|
|
| ||
| Chronic neutrophilic leukemia[13] |
|
|
|
↓ | – | – | – | – | +
The most common clinical finding |
|
|
|
|
|
| ||
| Disease | Etiology | Demography | History | Constitutional symptoms | Weight | Bleeding | Abdominal Pain | Vital sign | Jaundice | LAP | Hepatosplenomegaly | Other | CBC | Histopathology | Other | Gold standard diagnosis | Associated findings |
Epidemiology and Demographics
Prevalence
- In the United States, the age-adjusted prevalence of leukemia is 75.3 per 100,000 in 2011.[14]
Incidence
- The delay-adjusted incidence of leukemia in 2011 was estimated as 15.48 per 100,000 persons in the United States.
- In 2011, the age-adjusted incidence of leukemia was 13.66 per 100,000 persons in the United States.
Age
- The overall age-adjusted incidence of leukemia in the United States between 2007 and 2011 was 13 per 100,000. The age-adjusted incidence of leukemia by age category is:
- Under 65 years: 6.5 per 100,000
- 65 and over: 57.9 per 100,000
- Shown below is a table depicting the overall age-adjusted incidence of leukemia per 100,000 individuals by age in the United States between 2007 and 2011 for the different types of leukemia.
| Acute lymphoblastic leukemia | Chronic lymphocytic leukemia | Acute myeloid leukemia | Chronic myeloid leukemia | |
| All ages | 1.7 | 4.4 | 3.8 | 1.7 |
| <65 | 1.7 | 1.4 | 1.8 | 0.9 |
| ≥65 | 1.6 | 25.2 | 17.5 | 6.8 |
Gender
- In the United States, the age-adjusted prevalence of leukemia by gender in 2011 was:
- In males: 92.7 per 100,000
- In females: 60.7 per 100,000
- In the United States, the delay-adjusted incidence of leukemia by gender in 2011 was:
- In males: 19.93 per 100,000 persons
- In females: 11.89 per 100,000 persons
- In the United States, the age-adjusted incidence of leukemia by gender on 2011 was:
- In males: 17.58 per 100,000 persons
- In females: 10.49 per 100,000 persons
- Shown below is an image depicting the delay-adjusted incidence and observed incidence of leukemia by gender and race in the United States between 1975 and 2011. These graphs were gathered from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.
Race
- Shown below is a table depicting the age-adjusted prevalence of leukemia by race in 2011 in the United States.
| All Races | White | Black | Asian/Pacific Islander | Hispanic | |
| Age-adjusted prevalence | 75.3 per 100,000 | 83.5 per 100,000 | 45.9 per 100,000 | 41.2 per 100,000 | 57.1 per 100,000 |
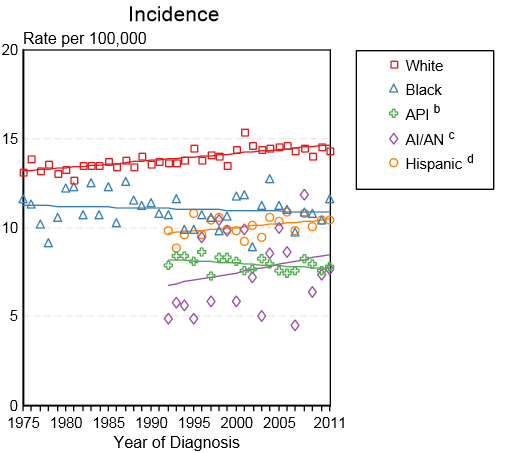
- Shown below is an image depicting the incidence of leukemia by race in the United States between 1975 and 2011.
API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native
Prognosis
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with leukemia was 60.3%.
- When stratified by age, the 5-year relative survival of patients with leukemia was 68.5% (44.1% for patients <65 and ≥ 65 years of age respectively).
- Shown below is a table depicting the 5-year relative survival of patients by the type of leukemia in the United States between 2004 and 2010.
| Acute lymphoblastic leukemia | Chronic lymphocytic leukemia | Acute myeloid leukemia | Chronic myeloid leukemia | |
| 5-year survival | 70% | 83.5% | 25.4% | 59.9% |
References
- ↑ Hoffbrand V, Moss P. Essential Haematology. John Wiley & Sons; 2011
- ↑ Saif A, Kazmi S, Naseem R, Shah H, Butt MO (August 2018). "Acute Myeloid Leukemia: Is That All There Is?". Cureus. 10 (8): e3198. doi:10.7759/cureus.3198. PMID 30410824. Vancouver style error: initials (help)
- ↑ Estey EH (April 2013). "Acute myeloid leukemia: 2013 update on risk-stratification and management". Am. J. Hematol. 88 (4): 318–27. doi:10.1002/ajh.23404. PMID 23526416.
- ↑ Sawalha Y, Advani AS (March 2018). "Management of older adults with acute lymphoblastic leukemia: challenges & current approaches". Int J Hematol Oncol. 7 (1): IJH02. doi:10.2217/ijh-2017-0023. PMC 6176956. PMID 30302234.
- ↑ Portell CA, Advani AS (April 2014). "Novel targeted therapies in acute lymphoblastic leukemia". Leuk. Lymphoma. 55 (4): 737–48. doi:10.3109/10428194.2013.823493. PMID 23841506.
- ↑ Saußele S, Silver RT (April 2015). "Management of chronic myeloid leukemia in blast crisis". Ann. Hematol. 94 Suppl 2: S159–65. doi:10.1007/s00277-015-2324-0. PMID 25814082.
- ↑ Eden RE, Coviello JM. PMID 30285354. Missing or empty
|title=(help) - ↑ Rai KR, Jain P (March 2016). "Chronic lymphocytic leukemia (CLL)-Then and now". Am. J. Hematol. 91 (3): 330–40. doi:10.1002/ajh.24282. PMID 26690614.
- ↑ Troussard X, Cornet E (December 2017). "Hairy cell leukemia 2018: Update on diagnosis, risk-stratification, and treatment". Am. J. Hematol. 92 (12): 1382–1390. doi:10.1002/ajh.24936. PMC 5698705. PMID 29110361.
- ↑ Wierda WG, Byrd JC, Abramson JS, Bhat S, Bociek G, Brander D, Brown J, Chanan-Khan A, Coutre SE, Davis RS, Fletcher CD, Hill B, Kahl BS, Kamdar M, Kaplan LD, Khan N, Kipps TJ, Lancet J, Ma S, Malek S, Mosse C, Shadman M, Siddiqi T, Stephens D, Wagner N, Zelenetz AD, Dwyer MA, Sundar H (November 2017). "Hairy Cell Leukemia, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology". J Natl Compr Canc Netw. 15 (11): 1414–1427. doi:10.6004/jnccn.2017.0165. PMID 29118233.
- ↑ Matutes E (March 2017). "Large granular lymphocytic leukemia. Current diagnostic and therapeutic approaches and novel treatment options". Expert Rev Hematol. 10 (3): 251–258. doi:10.1080/17474086.2017.1284585. PMID 28128670.
- ↑ Oshimi K (2017). "Clinical Features, Pathogenesis, and Treatment of Large Granular Lymphocyte Leukemias". Intern. Med. 56 (14): 1759–1769. doi:10.2169/internalmedicine.56.8881. PMC 5548667. PMID 28717070.
- ↑ Elliott MA, Tefferi A (August 2018). "Chronic neutrophilic leukemia: 2018 update on diagnosis, molecular genetics and management". Am. J. Hematol. 93 (4): 578–587. doi:10.1002/ajh.24983. PMID 29512199.
- ↑ Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.