Legionellosis differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
|||
| (22 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} | {{CMG}} [[Ogechukwu Hannah Nnabude, MD]] | ||
==Overview== | ==Overview== | ||
[[Legionnaires' disease]] must be differentiated from other causes of [[fever]], [[dyspnea]], [[cough]], and [[sputum]] production, such as [[bacterial pneumonia]], [[viral pneumonia]], and other causes of [[atypical pneumonia]]. | |||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
[[Legionnaires' disease]] must be differentiated from other causes of [[fever]], [[dyspnea]], [[cough]], and [[sputum]] production, such as [[bacterial pneumonia]], [[viral pneumonia]], and other causes of [[atypical pneumonia]].<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
{| | {| | ||
| Line 16: | Line 16: | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Chest X-ray | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Chest X-ray | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |[[ | ! align="center" style="background:#DCDCDC;" |[[Legionnaires' disease]] <ref name="pmid26231463">{{cite journal| author=Cunha BA, Burillo A, Bouza E| title=Legionnaires' disease. | journal=Lancet | year= 2016 | volume= 387 | issue= 10016 | pages= 376-385 | pmid=26231463 | doi=10.1016/S0140-6736(15)60078-2 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26231463 }} </ref> <ref name="pmid28159178">{{cite journal| author=Cunha BA, Cunha CB| title=Legionnaire's Disease: A Clinical Diagnostic Approach. | journal=Infect Dis Clin North Am | year= 2017 | volume= 31 | issue= 1 | pages= 81-93 | pmid=28159178 | doi=10.1016/j.idc.2016.10.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28159178 }} </ref> <ref name="pmid28159171">{{cite journal| author=Chahin A, Opal SM| title=Severe Pneumonia Caused by Legionella pneumophila: Differential Diagnosis and Therapeutic Considerations. | journal=Infect Dis Clin North Am | year= 2017 | volume= 31 | issue= 1 | pages= 111-121 | pmid=28159171 | doi=10.1016/j.idc.2016.10.009 | pmc=7135102 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28159171 }} </ref> | ||
| | | align="left" style="background:#F5F5F5;" | | ||
**[[ | *[[Dry cough]] | ||
*[[Fever|High grade fever]] | |||
*[[Breath sounds|Bronchial breath sounds]] | |||
*[[Asthenia]] | |||
*[[Dyspnea|Progressive dyspnea]] | |||
*[[diarrhea]] | |||
*[[Seizures]] and other neurological findings | |||
| | *[[nausea]], and [[vomiting]] | ||
*[[Adult respiratory distress syndrome]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*Legionella urinary antigen positive | *Legionella urinary antigen positive | ||
*[[Leukocytosis]] with relative [[lymphopenia]] | *[[Leukocytosis]] with relative [[lymphopenia]] | ||
*[[Hyponatremia]] | *[[Hyponatremia]] | ||
*[[Hypophosphatemia]] | *[[Hypophosphatemia]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
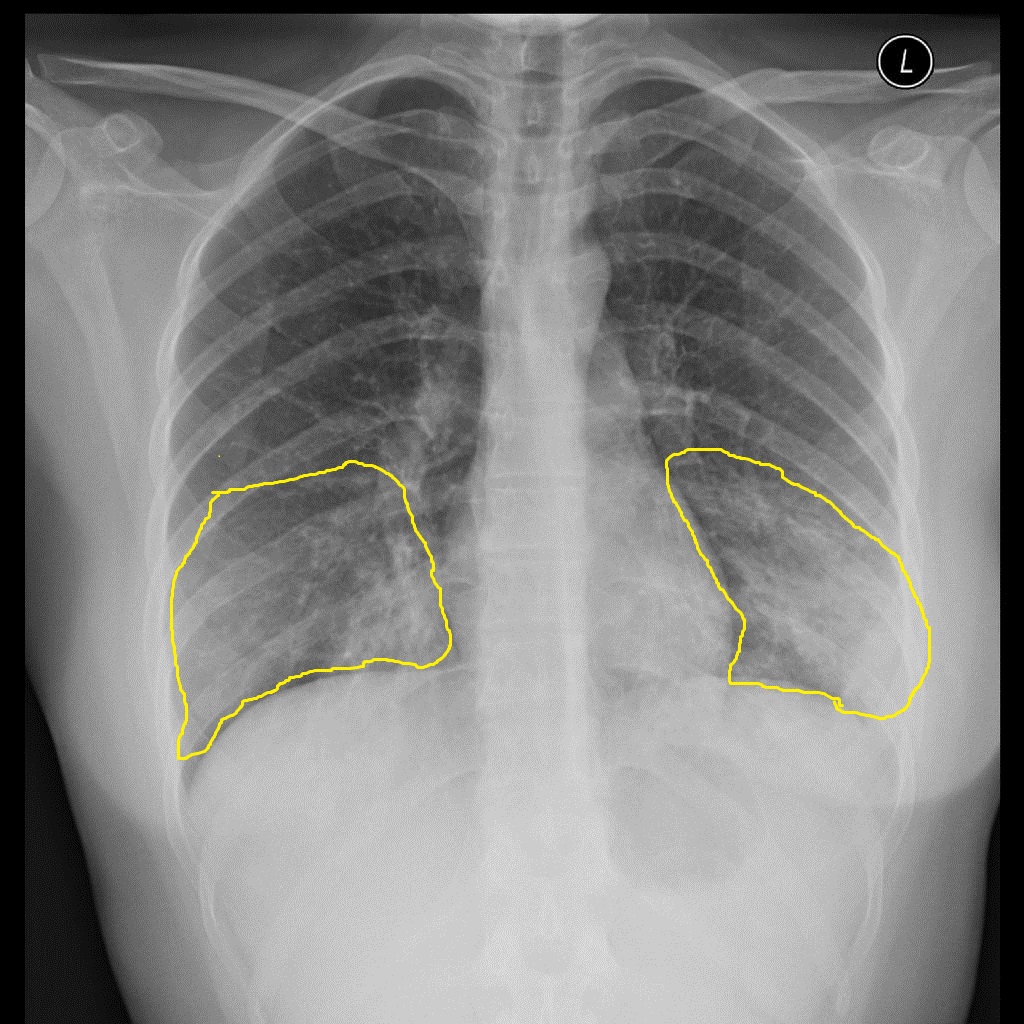
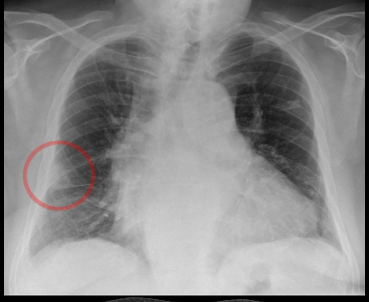
*[[Alveoli|Alveolar consolidation]] on chest radiograph | *[[Alveoli|Alveolar consolidation]] on chest radiograph | ||
*[[Consolidation (medicine)|Lobar consolidation]] on chest radiograph | *[[Consolidation (medicine)|Lobar consolidation]] on chest radiograph | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[File:Legionella pneumonie Chest Xray.jpg|thumb|Chest X-ray of a patient with Legionnaires disease courtesy Hellerhoff]] | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" | | ! align="center" style="background:#DCDCDC;" |[[Q fever]] <ref name="pmid15182283">{{cite journal| author=Okimoto N, Asaoka N, Osaki K, Kurihara T, Yamato K, Sunagawa T | display-authors=etal| title=Clinical features of Q fever pneumonia. | journal=Respirology | year= 2004 | volume= 9 | issue= 2 | pages= 278-82 | pmid=15182283 | doi=10.1111/j.1440-1843.2004.00586.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15182283 }} </ref> <ref name="pmid9743171">{{cite journal| author=Caron F, Meurice JC, Ingrand P, Bourgoin A, Masson P, Roblot P | display-authors=etal| title=Acute Q fever pneumonia: a review of 80 hospitalized patients. | journal=Chest | year= 1998 | volume= 114 | issue= 3 | pages= 808-13 | pmid=9743171 | doi=10.1378/chest.114.3.808 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9743171 }} </ref> | ||
| align="left" style="background:#F5F5F5;" | | |||
*[[Fever]] | |||
*Dry [[cough]] | |||
* [[ | *[[Dyspnea]] | ||
| | *[[Pleuritic chest pain]] | ||
* [[Antibody]] detection using [[Immunofluorescence|indirect immunofluorescence]] (IIF) | *[[myalgia]] | ||
* [[Polymerase chain reaction|PCR]] | *[[headache]] | ||
* [[Coxiella burnetii|''C. burnetii'']] | | align="left" style="background:#F5F5F5;" | | ||
* A two-to-three fold increase in [[Aspartate transaminase|AST]] and [[ALT]] | *[[Antibody]] detection using [[Immunofluorescence|indirect immunofluorescence]] (IIF) | ||
| | *[[Polymerase chain reaction|PCR]] | ||
| | *[[Coxiella burnetii|''C. burnetii'']] cultivated on special media such as embryonated eggs or cell culture | ||
[[Image:Q fever.gif|center|300px|thumb|Q fever pneumonia | *A two-to-three fold increase in [[Aspartate transaminase|AST]] and [[ALT]] | ||
| align="left" style="background:#F5F5F5;" | | |||
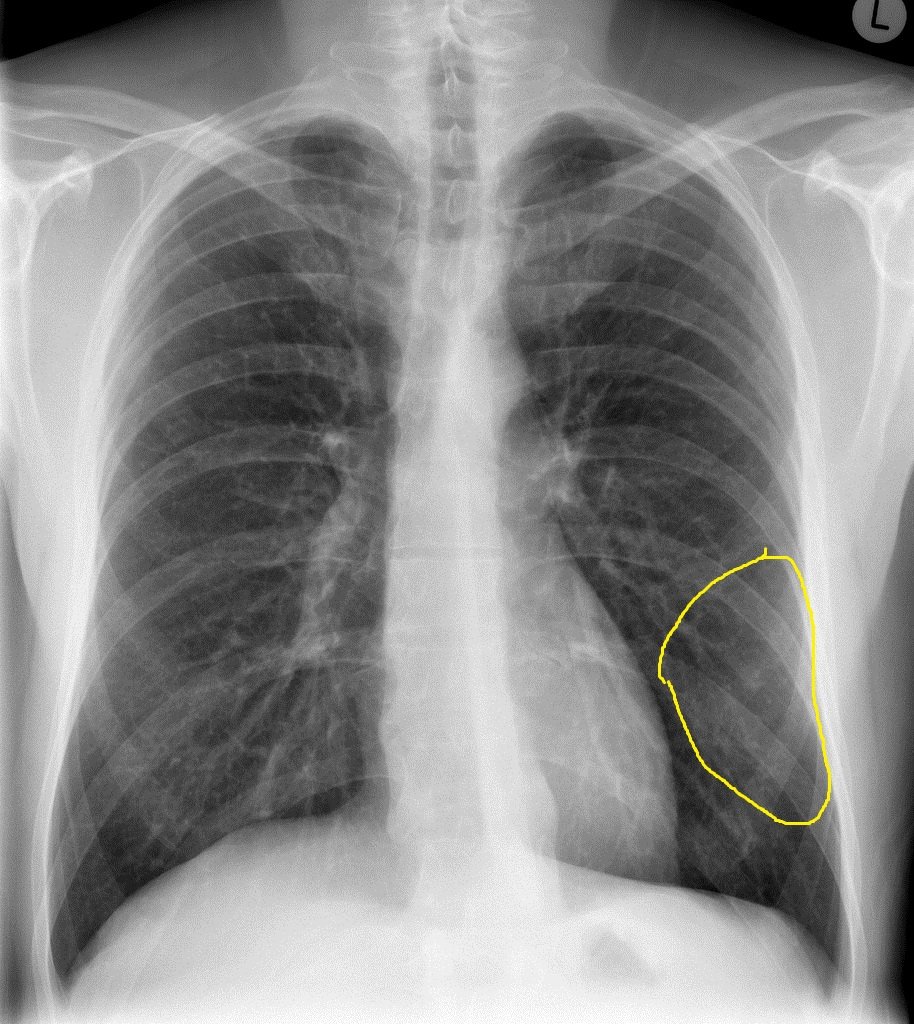
Multiple soft infiltrative shadows on CXR | |||
| align="center" style="background:#F5F5F5;" | | |||
[[Image:Q fever.gif|center|300px|thumb|Q fever pneumonia - Case courtesy of Royal Melbourne Hospital Respiratory, Radiopaedia.org, rID 21993 ]] | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |[[mycoplasma pneumonia|''Mycoplasma'' pneumonia]] | ! align="center" style="background:#DCDCDC;" |[[mycoplasma pneumonia|''Mycoplasma'' pneumonia]] <ref name="pmid27148202">{{cite journal| author=Parrott GL, Kinjo T, Fujita J| title=A Compendium for Mycoplasma pneumoniae. | journal=Front Microbiol | year= 2016 | volume= 7 | issue= | pages= 513 | pmid=27148202 | doi=10.3389/fmicb.2016.00513 | pmc=4828434 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27148202 }} </ref> <ref name="pmid29264006">{{cite journal| author=Saraya T| title=Mycoplasma pneumoniae infection: Basics. | journal=J Gen Fam Med | year= 2017 | volume= 18 | issue= 3 | pages= 118-125 | pmid=29264006 | doi=10.1002/jgf2.15 | pmc=5689399 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29264006 }} </ref> | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Dry cough]] | *[[Dry cough]] | ||
*[[Fever]] | |||
*[[Pharyngitis]] | |||
*[[Nausea and vomiting]] | |||
*[[Sinus congestion]] | |||
*[[Pleuritic chest pain]] | *[[Pleuritic chest pain]] | ||
*[[Inflamed]], opaque, hypomobile [[tympanic membrane]] | *[[Inflamed]], opaque, hypomobile [[tympanic membrane]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Lymphocytosis]] | |||
*[[Cold agglutinins]] positive | |||
* [[Leukocytosis]] | *Positive [[CoNombs test]] | ||
* [[Thrombocytosis]] | *[[Leukocytosis]] | ||
| | *[[Thrombocytosis]] | ||
| align="left" style="background:#F5F5F5;" | | |||
*[[Alveolar]] [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *[[Alveolar]] [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
*Interstitial infiltrate on [[chest radiograph]] | *Interstitial infiltrate on [[chest radiograph]] | ||
*Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[Image:Atypical-pneumonia-mycoplasma - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781.jpg|center|300px|thumb|Mycoplasma pneumonia - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781]] | [[Image:Atypical-pneumonia-mycoplasma - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781.jpg|center|300px|thumb|Mycoplasma pneumonia - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781]] | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |[[Chlamydia pneumonia]] | ! align="center" style="background:#DCDCDC;" |[[Chlamydia pneumonia]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
* | *Associated with [[upper respiratory tract]] symptoms | ||
*Associated with extrapulmonary maifestations such as: | |||
**[[Meningitis]] | |||
* | **[[Guillain-Barre syndrome]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
* | *Normal WBC count | ||
* | *Positive [[Antibody|antichlamydial antibody]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[Image:Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567.jpg|center|300px|thumb|Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567]] | [[Image:Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567.jpg|center|300px|thumb|Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567]] | ||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |Acute interstitial pneumonia | ! align="center" style="background:#DCDCDC;" |[[Acute interstitial pneumonia]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Dry cough]] | *[[Dry cough]] | ||
*[[Dyspnea|Progressive dyspnea]] | *[[Dyspnea|Progressive dyspnea]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*Nonspecific | *Nonspecific | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*Disseminated [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *Disseminated [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
*Interstitial infiltrate on chest radiograph | *Interstitial infiltrate on chest radiograph | ||
*Increased uptake on gallium scan | *Increased uptake on gallium scan | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[File:Acute Interstitial Pneumonitis Chest Xray - Case Courtesy of Dr Salam, Radiopaedia, rID 45404.jpeg|thumb|Acute Interstitial Pneumonitis Chest X-ray - Case Courtesy of Dr Salam, Radiopaedia, rID 45404]] | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |Pneumococcal pneumonia | ! align="center" style="background:#DCDCDC;" |[[Pneumococcal pneumonia]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Fever|High grade fever]] | *[[Fever|High grade fever]] | ||
*[[Hemoptysis]] | *[[Hemoptysis]] | ||
| Line 107: | Line 119: | ||
*[[Productive cough]] | *[[Productive cough]] | ||
*[[Egophony]] | *[[Egophony]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Gram positive bacteria|Gram positive]] [[diplococci]] on sputum Gram stain | *[[Gram positive bacteria|Gram positive]] [[diplococci]] on sputum Gram stain | ||
*[[Pleural effusion]] ([[exudative]]) | *[[Pleural effusion]] ([[exudative]]) | ||
*Respiratory alkalosis | *Respiratory alkalosis | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*Parenchymal hyperlucency on [[chest radiograph]] | *Parenchymal hyperlucency on [[chest radiograph]] | ||
*Increased uptake on [[gallium scan]] | *Increased uptake on [[gallium scan]] | ||
| Line 117: | Line 129: | ||
*Alveolar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *Alveolar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
*Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[File:Pneumococcal Pneumonia Chest Xray..jpg|thumb|Chest X-ray of a patient with pneumococcal pneumonia - case courtesy Dr Jack Ren, Radiopaedia.org, rID 29090]] | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |Pneumocystis carinii pneumonia | ! align="center" style="background:#DCDCDC;" |[[Pneumocystis carinii pneumonia]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Immunosuppressive]] state | *[[Immunosuppressive]] state | ||
*[[Subcutaneous emphysema]] | *[[Subcutaneous emphysema]] | ||
*[[Cough|Hacking cough]] | *[[Cough|Hacking cough]] | ||
*[[Dyspnea|Progressive dyspnea]] | *[[Dyspnea|Progressive dyspnea]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Respiratory alkalosis]] | *[[Respiratory alkalosis]] | ||
*Serum beta-D-glucan elevation | *Serum beta-D-glucan elevation | ||
| | | align="left" style="background:#F5F5F5;" | | ||
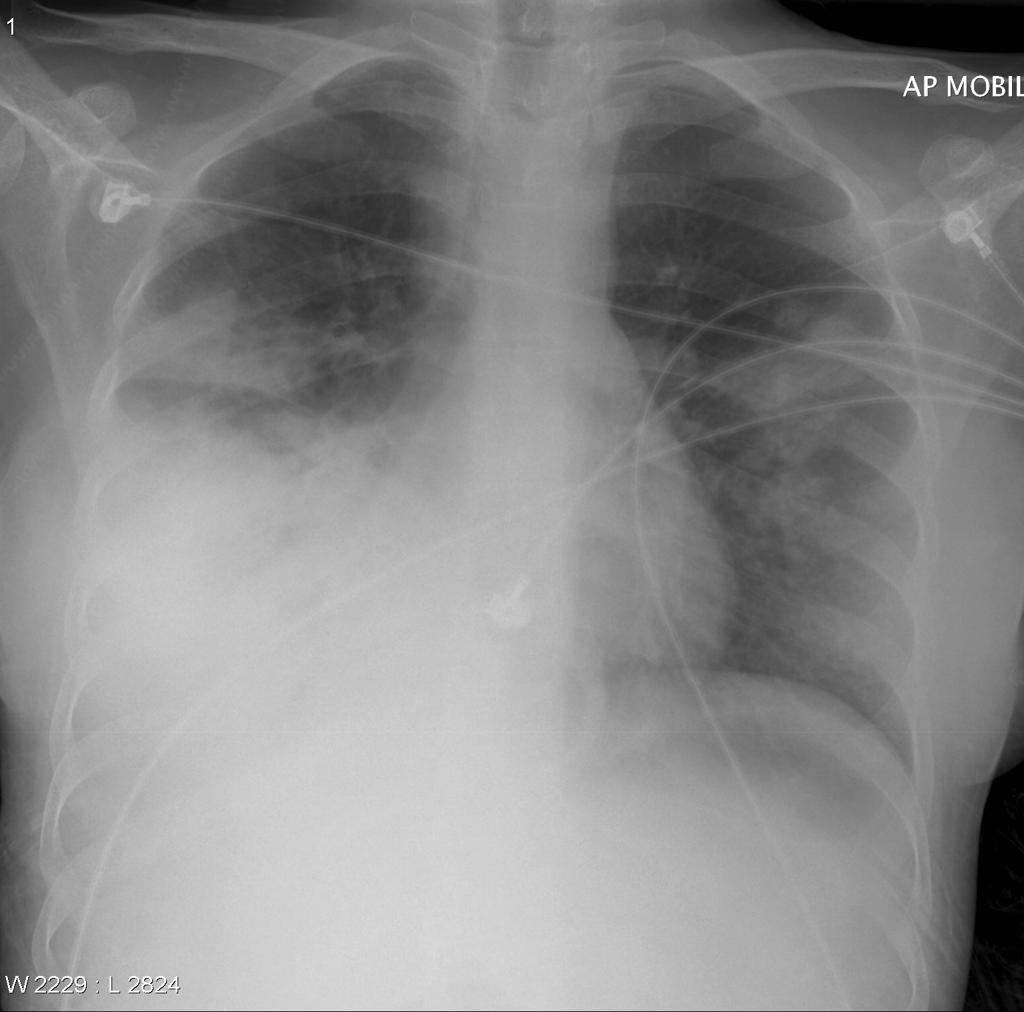
*[[Alveolar]] [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *[[Alveolar]] [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
*Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
*Interstitial infiltrate on [[chest radiograph]] | *Interstitial infiltrate on [[chest radiograph]] | ||
*[[Pneumomediastinum]] on [[chest radiograph]] | *[[Pneumomediastinum]] on [[chest radiograph]] | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[File:Acute Interstitial Pneumonitis Chest Xray - Case Courtesy of Dr Salam, Radiopaedia, rID 45404.jpeg|thumb|Pneumocystis Jiroverci Chest Xray - Case Courtesy of Dr Behrang Amini, Radiopaedia, rID 1901]] | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" |Pulmonary embolism | ! align="center" style="background:#DCDCDC;" |[[Pulmonary embolism]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*Calf [[pain]] or [[swelling]] | *Calf [[pain]] or [[swelling]] | ||
*Decreased [[pulse pressure]] | *Decreased [[pulse pressure]] | ||
| Line 154: | Line 168: | ||
*[[Venous stasis]] | *[[Venous stasis]] | ||
*[[Bone fracture]] | *[[Bone fracture]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[D-dimer]] elevation | *[[D-dimer]] elevation | ||
*[[Hypocapnia]] | *[[Hypocapnia]] | ||
| Line 162: | Line 176: | ||
*[[Right axis deviation]] on ECG | *[[Right axis deviation]] on ECG | ||
*Right ventricular overload on ECG | *Right ventricular overload on ECG | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*Normal [[chest radiograph]] | *Normal [[chest radiograph]] | ||
*[[Atelectasis]] on [[chest radiograph]] | *[[Atelectasis]] on [[chest radiograph]] | ||
| Line 172: | Line 186: | ||
*Segmental [[perfusion]] defect on lung scan | *Segmental [[perfusion]] defect on lung scan | ||
*[[V/Q scan|V/Q]] mismatch on lung scan | *[[V/Q scan|V/Q]] mismatch on lung scan | ||
| | | align="center" style="background:#F5F5F5;" | | ||
[[File:Hampton Hump.PNG|thumb|Hampton Hump in a patient with pulmonary embolism courtesy of Hellerhoff]] | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" | | ! align="center" style="background:#DCDCDC;" |[[Viral pneumonia]] | ||
| align="left" style="background:#F5F5F5;" | | |||
| | |||
| | |||
*[[Pleuritic chest pain]] | *[[Pleuritic chest pain]] | ||
*[[Breath sounds|Bronchial breath sounds]] | *[[Breath sounds|Bronchial breath sounds]] | ||
| Line 202: | Line 196: | ||
*Fine [[rales]] | *Fine [[rales]] | ||
*[[Breath sounds|Bronchovesicular breath sounds]] | *[[Breath sounds|Bronchovesicular breath sounds]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*[[Lymphocytosis]] | *[[Lymphocytosis]] | ||
*[[Respiratory alkalosis]] | *[[Respiratory alkalosis]] | ||
| | | align="left" style="background:#F5F5F5;" | | ||
*Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | *Lobar [[Consolidation (medicine)|consolidation]] on [[chest radiograph]] | ||
*Interstitial infiltrate on [[chest radiograph]] | *Interstitial infiltrate on [[chest radiograph]] | ||
| | | align="center" style="background:#F5F5F5;" | | ||
|} | |} | ||
==References== | ==References== | ||
Latest revision as of 20:58, 28 July 2022
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Ogechukwu Hannah Nnabude, MD
Overview
Legionnaires' disease must be differentiated from other causes of fever, dyspnea, cough, and sputum production, such as bacterial pneumonia, viral pneumonia, and other causes of atypical pneumonia.
Differential Diagnosis
Legionnaires' disease must be differentiated from other causes of fever, dyspnea, cough, and sputum production, such as bacterial pneumonia, viral pneumonia, and other causes of atypical pneumonia.[1]
| Disease | Clinical manifestation | Lab findings | Imaging findings | Chest X-ray |
|---|---|---|---|---|
| Legionnaires' disease [2] [3] [4] |
|
|
|
 |
| Q fever [5] [6] |
|
Multiple soft infiltrative shadows on CXR |
 | |
| Mycoplasma pneumonia [7] [8] |
|
|
|
 |
| Chlamydia pneumonia |
|
|
 | |
| Acute interstitial pneumonia |
|
|
 | |
| Pneumococcal pneumonia |
|
|
|
 |
| Pneumocystis carinii pneumonia |
|
|
 | |
| Pulmonary embolism |
|
|
|
 |
| Viral pneumonia |
|
References
- ↑ Irfan M, Farooqi J, Hasan R (2013). "Community-acquired pneumonia". Curr Opin Pulm Med. 19 (3): 198–208. doi:10.1097/MCP.0b013e32835f1d12. PMID 23422417.
- ↑ Cunha BA, Burillo A, Bouza E (2016). "Legionnaires' disease". Lancet. 387 (10016): 376–385. doi:10.1016/S0140-6736(15)60078-2. PMID 26231463.
- ↑ Cunha BA, Cunha CB (2017). "Legionnaire's Disease: A Clinical Diagnostic Approach". Infect Dis Clin North Am. 31 (1): 81–93. doi:10.1016/j.idc.2016.10.007. PMID 28159178.
- ↑ Chahin A, Opal SM (2017). "Severe Pneumonia Caused by Legionella pneumophila: Differential Diagnosis and Therapeutic Considerations". Infect Dis Clin North Am. 31 (1): 111–121. doi:10.1016/j.idc.2016.10.009. PMC 7135102 Check
|pmc=value (help). PMID 28159171. - ↑ Okimoto N, Asaoka N, Osaki K, Kurihara T, Yamato K, Sunagawa T; et al. (2004). "Clinical features of Q fever pneumonia". Respirology. 9 (2): 278–82. doi:10.1111/j.1440-1843.2004.00586.x. PMID 15182283.
- ↑ Caron F, Meurice JC, Ingrand P, Bourgoin A, Masson P, Roblot P; et al. (1998). "Acute Q fever pneumonia: a review of 80 hospitalized patients". Chest. 114 (3): 808–13. doi:10.1378/chest.114.3.808. PMID 9743171.
- ↑ Parrott GL, Kinjo T, Fujita J (2016). "A Compendium for Mycoplasma pneumoniae". Front Microbiol. 7: 513. doi:10.3389/fmicb.2016.00513. PMC 4828434. PMID 27148202.
- ↑ Saraya T (2017). "Mycoplasma pneumoniae infection: Basics". J Gen Fam Med. 18 (3): 118–125. doi:10.1002/jgf2.15. PMC 5689399. PMID 29264006.