Left bundle branch block electrocardiogram
|
Left bundle branch block Microchapters |
|
Differentiating Left Bundle Branch Block from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Left bundle branch block electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Left bundle branch block electrocardiogram |
|
Risk calculators and risk factors for Left bundle branch block electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Electrocardiogram
Electrocardiographic Criteria
The criteria to diagnose a left bundle branch block on an electrocardiogram includes the following:
- The heart rhythm must be supraventricular in origin. A wide QRS complex that is not preceded by P waves would not qualify.
- The QRS duration must be greater than or equal to 120 milliseconds.
- There should be a QS or rS complex in lead V1.
- There should be a monophasic R wave in lead I and lead V6.
The T wave deflection should be opposite of the terminal deflection of the QRS complex. This lack of concordance in direction is known as appropriate T wave discordance, and it is expected in patients with a left bundle branch block. A concordant T wave may suggest the presence of either ischemia or myocardial infarction.
Reading Ischemia in The Presence of LBBB
LBBB can simulate an MI due to the associated secondary ST changes and pseudoinfarction q waves that it is associated with. It can mask the EKG changes of an MI.
Ordinarily in the setting of left bundle branch block, the T waves are inverted in the lateral leads (they are 'discordant'). If they become upright, they are called 'concordant', and concordant T waves can be observed in ST elevation MI. The EKG below was obtained in a patient with a new left bundle branch block (LBBB) and a totally occluded left anterior descending artery.

Sgarbossa's Criteria
An EKG scoring system was developed, and the Sgarbossa's criteria were assessed on patients from the GUSTO-1 trial. These patients were scored from 0-5 for the presence of LBBB in the context of an acute myocardial infarction.[1] Three criteria are included in the scoring system, and a score of at least 3 points is required to make the diagnosis of STEMI.
| Criteria | Score |
| ST-segment elevation ≥ 1 mm and concordant with QRS complex | 5 points |
| ST-segment depression ≥ 1 mm in lead V1,V2, or V3 | 3 points |
| ST-segment elevation ≥ 5 mm and discordant with QRS complex | 2 points |
Cabrera's Sign
Cabrera's sign refers to notching at 40 milliseconds in the ascending limb of the S wave in leads V3 and V4. This sign has a sensitivity of 27% and specificity approaching 90%.
Chapman's Sign
Chapman's sign refers to prominent notching of the ascending limb of the R wave in lead V5 or V6. Similar to Cabrera's sign, this sign has a very low sensitivity but specificity approaching 90%.
Pseudoinfarct Patterns: Simulation of an Anterior MI
- LBBB can cause a poor R wave progression. In the presence of LBBB, there is often a decrease in the amplitude of R waves to the mid precordium in the absence of a septal infarct.
- QS complexes are often seen in the right precordial leads in uncomplicated LBBB, and they may even extend as far out as V5 or V6.
- Non infarctional Q waves may be seen in aVL.
- The electrical basis for the appearance of q waves is that LBBB] causes a loss of the normal septal R waves in the right precordial leads. The septum is no longer being depolarized from left to right as it normally does because of the delay in conduction down the left bundle. Therefore, there is a loss of the early R wave.
- There can occasionally be Rs complexes in V1. These unanticipated initial positive forces are due to early RV depolarization and may actually mask the q waves (i.e. loss of initial septal forces) that accompany an anteroseptal MI.
Simulation of an Inferior MI
- Noninfarctional QS complexes can be seen in leads II, III, and aVF in LBBB.
- There are a number of autopsy cases were there are QS waves inferiorly without evidence of an MI.
- There are several reported cases of intermittent LBBB in which the inferior QS waves were present only in the aberrantly conducted beats.
- Conversely, LBBB may mask the development of Q waves in an MI.
Secondary ST segment and T Wave Changes
- Primary ST segment and T wave changes are repolarization changes that are seen with ischemia or electrolyte imbalance. They reflect actual changes in the myocardial action potentials.
- Secondary ST segment and T wave changes occur when the sequence of ventricular activation is altered without any disturbance in the electrical properties of the myocardial cells such as those seen in LBBB.
- As a result of secondary ST segment and T wave changes, the QRS and the T wave vectors are oriented in opposite directions. This finding is known as discordance of the QRS and T wave vectors.
- The QRS is often predominantly negative in the right precordial leads while the T wave is oriented positively. In those leads where there is a tall positive R wave there is a negative T wave.
- These secondary ST segment and T wave changes often mimic infarction, and furthermore they may mask the ST segment and T wave changes of an MI.
- Sometimes primary ST segment and T wave changes will be superimposed on the LBBB pattern and the following suggests the diagnosis of ischemia or infarction:
- ST segment elevation in leads with a predominant R wave. In uncomplicated LBBB, the ST segment is isoelectric or depressed.
- T wave inversions in the right to midprecordial leads or in other leads with a predominantly negative QRS. In other words there is an absence of discordance, and there is the presence of concordance.
- Morphology: In leads with a predominant R wave, the ST segment begins to slope downwards and blends into the T wave. The ascending limb of the T wave ascends back to the baseline at a more acute angle.
- The ischemic T waves have a more symmetric appearance and a slightly upwardly bowed ST segment.
- ST segment and T wave elevations simulating acute infarction: The ST segment can be markedly elevated (up to 10 mm or more at the J point ) in leads with a QS or rS segment in uncomplicated LBBB. In addition, there can be a loss of R wave progression.
- T wave inversions in intermittent LBBB: May develop deep T wave inversions in the right to midprecordial leads of normally conducted beats in the absence of CAD. These T wave inversions are deepest in leads V1 to V4 with a symmetric or coved appearance.
Etiology of Q Waves
- As described earlier, in LBBB there is a loss of depolarization from left to right, which produced an initial r wave in the right precordial leads.
- Now there is depolarization from right to left. Consequently the initial r wave is lost, and the non infarctional QS complexes may appear in the precordial leads.
- The reversal of septal activation results in RS complexes in the left precordial leads.
Can You Read a Left Ventricular Free Wall Infarction in the Presence of a LBBB?
- No. This pattern of infarction results in abnormal q waves in the midprecordial to lateral precordial leads.
- In LBBB the initial septal depolarization forces are directed from right to left. These leftward septal forces will produce an initial R wave in the midprecordial to the lateral precordial leads, masking the loss of potential q waves produced by the infarction.
- Therefore, left ventricular free wall infarction by itself will not produce diagnostic q waves in the presence of a LBBB.
- Poor R wave progression is seen in uncomplicated LBBB.
Can You Read a Septal Infarction in the Presence of LBBB?
- Yes. The septal forces are directed to the left in LBBB.
- If enough of the septum is infarcted, abnormal QR, QRS, or qrs types of complexes may appear in the midprecordial to lateral precordial leads in order to eliminate the initial leftward septal forces.
- These initial q waves may reflect posterior and superior forces from the spared basal portion of the septum.
- Small q waves of 0.03 sec or less may be seen in leads I, V5, and V6 in uncomplicated LBBB.
- The presence of q waves laterally is an example of false localization. [2]
Incomplete LBBB
The criteria for diagnosing an incomplete LBBB include:
- QRS duration between 110 and 119 ms in adults, between 90 and 100 ms in children 8 to 16 years of age, and between 80 and 90 ms in children less than 8 years of age.
- Presence of left ventricular hypertrophy pattern.
- R peak time greater than 60 ms in leads V4, V5, and V6.
- Absence of Q wave in leads I, V5, and V6.
- ST and T wave displacement opposite to the major deflection of the QRS complex.
EKG Examples
Shown below is an EKG of left bundle branch block depicting an RsR' pattern (M pattern) in lead V6, and a wide QRS complex in both leads V1 and V6.
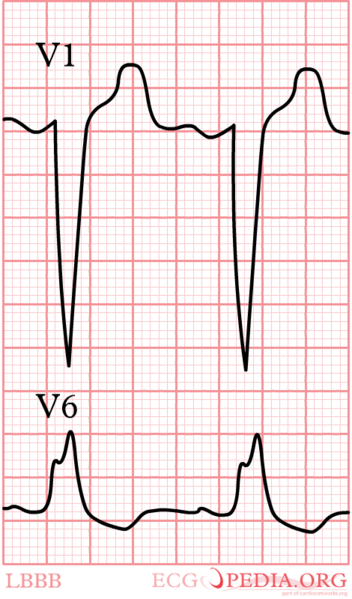
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:LBBB.png
Shown below is an EKG with an RsR' pattern (M pattern) in leads V4, V5, and V6 suggesting a left bundle branch block. Also seen are wide QRS complexes throughout the precordium, and ST segment depression in leads II, V5, and V6.
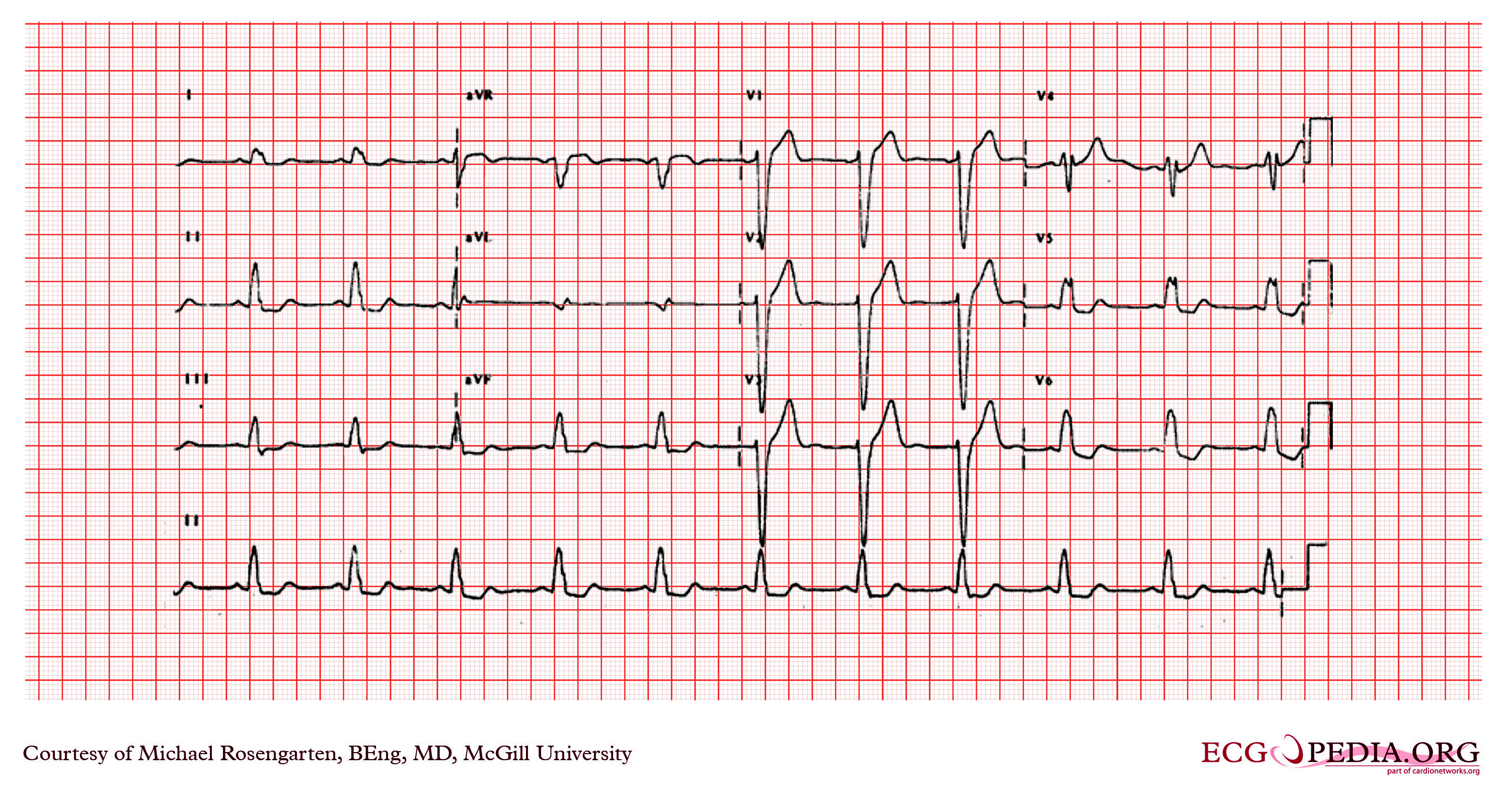
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:E23.jpg
Shown below is an EKG with a left axis deviation and an RsR' pattern (M pattern) in all limb leads (leads I, II, III, aVR, aVL, and aVF) and in lead V6, depicting a left bundle branch block. Tachycardia is also present with a rate of more than 100 beats per minute.
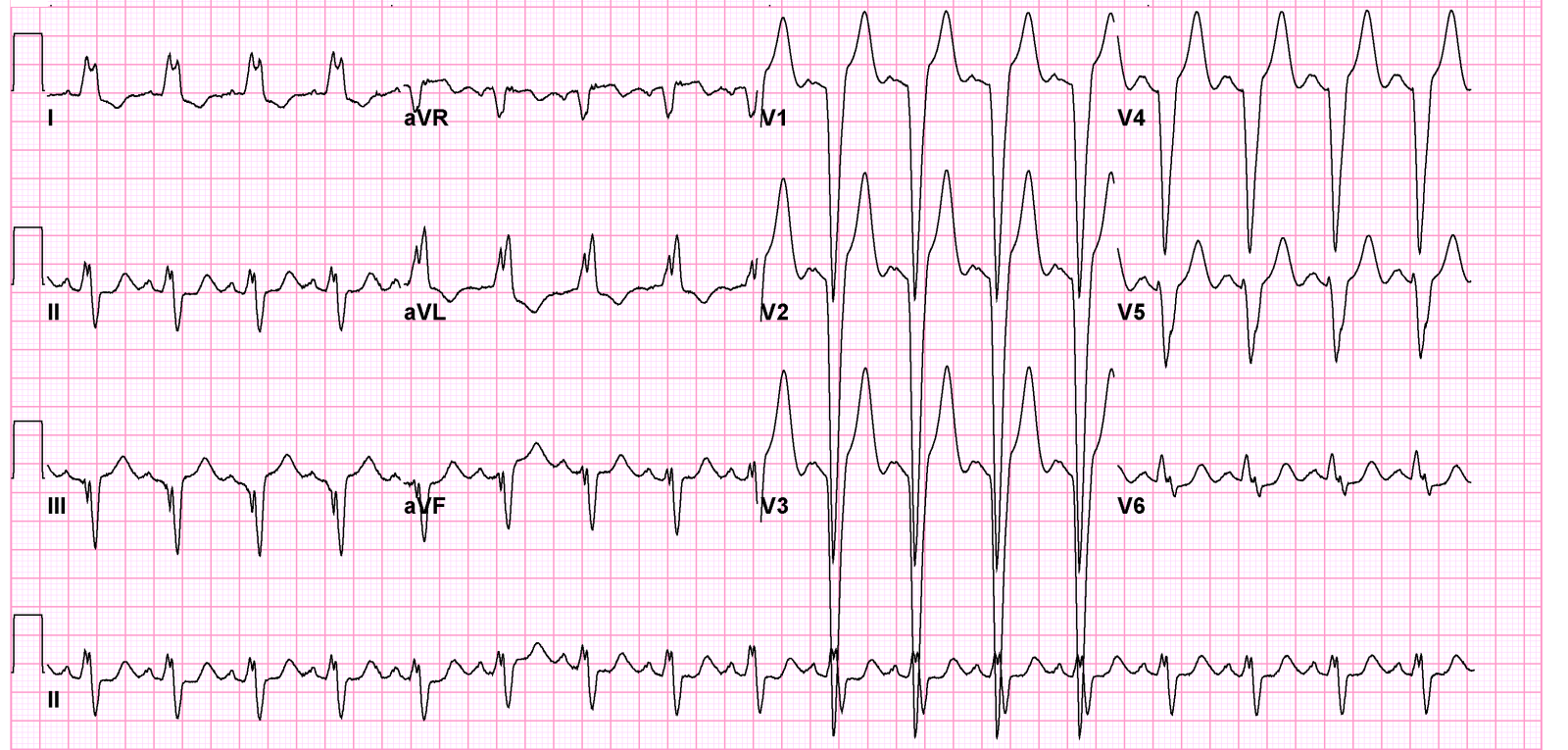
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:12leadLBTB.png
Shown below is an EKG with a left axis deviation and an RsR' pattern (M pattern) throughout the precordium, depicting a left bundle branch block. The EKG also shows wide QRS complexes and a prolonged PR interval.
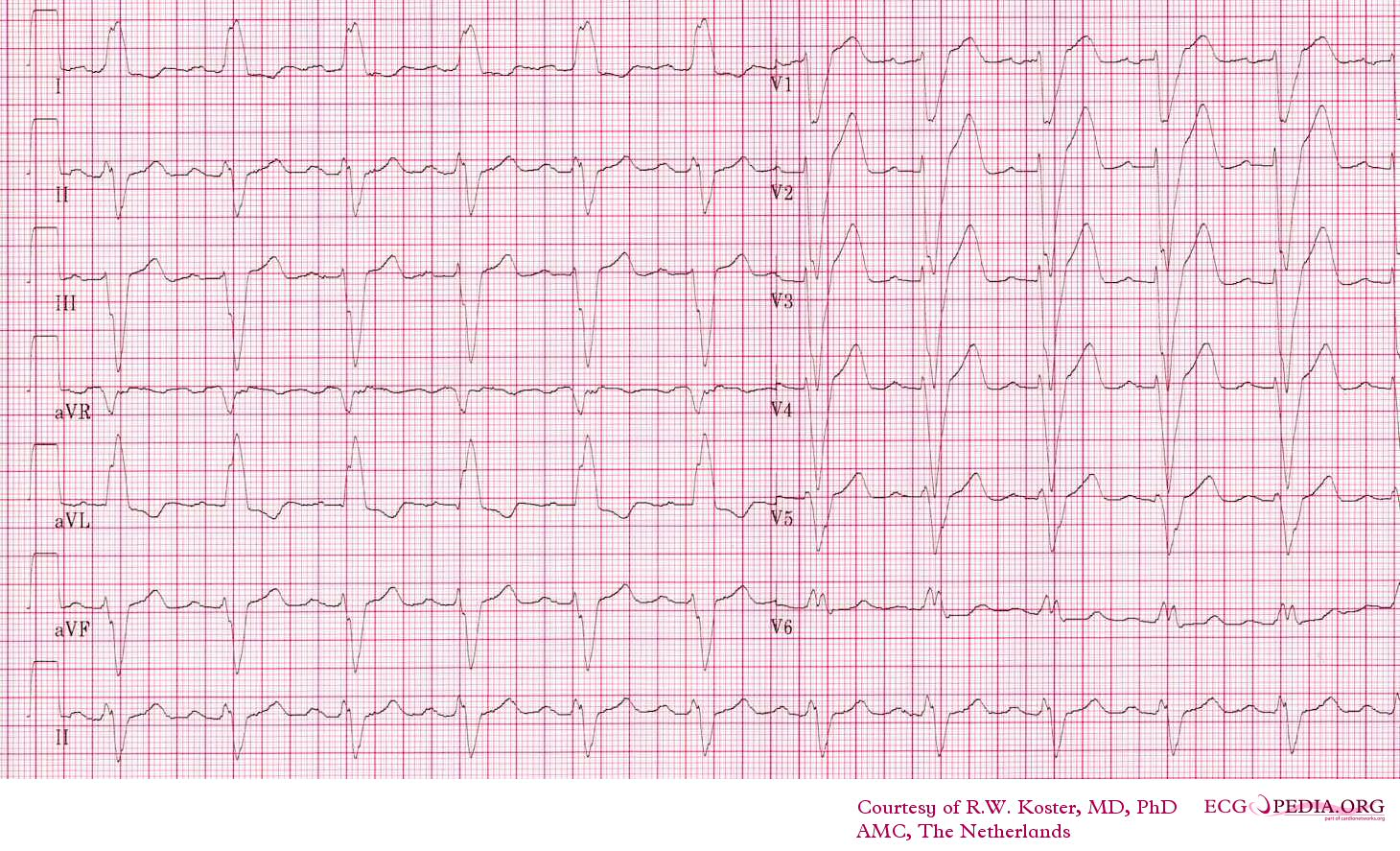
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/File:12leadLBTB002.jpg
EKG Video
{{#ev:youtube|HPLR_lixSpY&feature=related}}
For more EKG examples of First Degree AV Block click here
References
- ↑ Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM, Wagner GS (1996). "Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators". N. Engl. J. Med. 334 (8): 481–7. PMID 8559200. Unknown parameter
|month=ignored (help) - ↑ Myocardial Infarction, Electrocardiographic Differential Dx, Ary L. Goldberger, 3rd ed., Mosby Co., St. Louis, 1984, p.85 93.