Ischemic colitis pathophysiology
|
Ischemic colitis Microchapters |
|
Case Studies |
|
Ischemic colitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ischemic colitis pathophysiology |
|
Risk calculators and risk factors for Ischemic colitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Pathophysiology
Colonic Blood Supply
- The colon receives blood from both the superior and inferior mesenteric arteries. The blood supply from these two major arteries overlap, with abundant collateral circulation. However, there are weak points, or "watershed" areas, at the borders of the territory supplied by each of these arteries. These watershed areas are most vulnerable to ischemia when blood flow decreases, as they have the fewest vascular collaterals.
- The rectum receives blood from both the inferior mesenteric artery and the internal iliac artery; the rectum is rarely involved by colonic ischemia due to this dual blood supply.
Development of Ischemia
- Under ordinary conditions, the colon receives between 10% and 35% of the total cardiac output.[1] If blood flow to the colon drops by more than about 50%, ischemia will develop.
- The arteries feeding the colon are very sensitive to vasoconstrictors; presumably this is an evolutionary adaptation to shunt blood away from the bowel and to the heart and brain in times of stress.[2] As a result, during periods of low blood pressure, the arteries feeding the colon clamp down vigorously.
- A similar process can result from vasoconstricting drugs such as ergotamine, cocaine, or vasopressors. This vasoconstriction can result in non-occlusive ischemic colitis.
Microscopic Pathology
- A range of pathologic findings are seen in ischemic colitis, corresponding to the spectrum of clinical severity.
- In its mildest form, mucosal and submucosal hemorrhage and edema are seen, possibly with mild necrosis or ulceration.
- With more severe ischemia, a pathologic picture resembling inflammatory bowel disease (i.e. chronic ulcerations, crypt abscesses and pseudopolyps) may be seen.[3]
- In the most severe cases, transmural infarction with resulting perforation may be seen.
- After recovery, the muscularis propria may be replaced by fibrous tissue, resulting in a stricture.
- Following restoration of normal blood flow, reperfusion injury may also contribute to the damage to the colon.[4]
Images
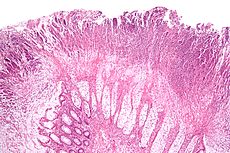
Micrograph of a colonic pseudomembrane, a finding that may be associated with ischemic colitis. H&E stain.
Videos
{{#ev:youtube|LCwMQU7ylYg}}
References
- ↑ UpToDate, Colonic ischemia, accessed 2 September 2006.
- ↑ Rosenblum J, Boyle C, Schwartz L (1997). "The mesenteric circulation. Anatomy and physiology". Surg Clin North Am. 77 (2): 289–306. PMID 9146713.
- ↑ Brandt LJ, Boley SJ, Goldberg L, et al: Colitis in the elderly. Am J Gastroenterol 76:239, 1981.
- ↑ Granger D, Rutili G, McCord J (1981). "Superoxide radicals in feline intestinal ischemia". Gastroenterology. 81 (1): 22–9. PMID 6263743.