Ischemic colitis pathophysiology: Difference between revisions
Hamid Qazi (talk | contribs) No edit summary |
Hamid Qazi (talk | contribs) No edit summary |
||
| Line 14: | Line 14: | ||
**These [[Watershed Area (medical)|watershed]] areas are most vulnerable to [[ischemia]] when [[blood]] flow decreases, as they have the fewest [[vascular]] collaterals. | **These [[Watershed Area (medical)|watershed]] areas are most vulnerable to [[ischemia]] when [[blood]] flow decreases, as they have the fewest [[vascular]] collaterals. | ||
* [[Rectum]] receives [[blood]] from the [[inferior mesenteric artery]] and the [[internal iliac artery]] | * [[Rectum]] receives [[blood]] from the [[inferior mesenteric artery]] and the [[internal iliac artery]] and is rarely affected by colonic [[ischemia]] due to its dual [[blood]] supply. | ||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 21: | Line 20: | ||
===Development of Ischemia=== | ===Development of Ischemia=== | ||
* [[Colon (anatomy)| | * The [[Colon (anatomy)|colon]] receives between 10% and 35% of the total [[cardiac output]]. | ||
*If [[blood]] flow to the colon drops by more than about 50%, [[ischemia]] will develop. | *If [[blood]] flow to the colon drops by more than about 50%, [[ischemia]] will develop. | ||
* The [[Artery|arteries]] feeding the [[Colon (anatomy)|colon]] are very sensitive to [[vasoconstrictors]] | * The [[Artery|arteries]] feeding the [[Colon (anatomy)|colon]] are very sensitive to [[vasoconstrictors|vasoconstrictors and]] during periods of [[hypotension|low blood pressure]] the [[Artery|arteries]] will collapse. | ||
* [[Vasoconstriction|Vasoconstricting]] drugs such as [[ergotamine]], [[cocaine]], or [[vasopressor]]s can also cause colonic [[ischemia]] with results in non-occlusive [[Ischemia|ischemic]] colitis. | * [[Vasoconstriction|Vasoconstricting]] drugs such as [[ergotamine]], [[cocaine]], or [[vasopressor]]s can also cause colonic [[ischemia]] with results in non-occlusive [[Ischemia|ischemic]] colitis. | ||
Revision as of 20:03, 31 January 2018
|
Ischemic colitis Microchapters |
|
Case Studies |
|
Ischemic colitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ischemic colitis pathophysiology |
|
Risk calculators and risk factors for Ischemic colitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Hamid Qazi, MD, BSc [2]
Overview
Ischemic colitis is the result of a sudden reduction in blood flow that is insufficient to meet the metabolic demands of the region of colon. Ischemic change will subsequently extend from the mucosa to the serosa. Mucosal injury will develop in 20 minutes to 1 hour, and transmural infarction occurs within 8 to 16 hours. Reperfusion injury can occur with the release of reactive oxygen species, which cause lipid peroxidation within cell membranes, causing cell necrosis.
Physiology
Colonic Blood Supply
- The physiology of blood supply is as follows:[1]
- Colon receives blood from the superior and inferior mesenteric arteries.
- Blood supply from these arteries overlap, with abundant collateral circulation.
- There are weak points, or "watershed" areas, at the borders of the territory supplied by each of these arteries.
- Rectum receives blood from the inferior mesenteric artery and the internal iliac artery and is rarely affected by colonic ischemia due to its dual blood supply.
Pathophysiology
The pathophysiology of ischemic colitis is as follows:[2][3][4]
Development of Ischemia
- The colon receives between 10% and 35% of the total cardiac output.
- If blood flow to the colon drops by more than about 50%, ischemia will develop.
- The arteries feeding the colon are very sensitive to vasoconstrictors and during periods of low blood pressure the arteries will collapse.
- Vasoconstricting drugs such as ergotamine, cocaine, or vasopressors can also cause colonic ischemia with results in non-occlusive ischemic colitis.
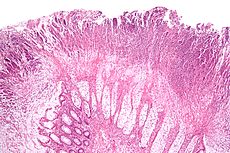
Microscopic Pathology
- A range of pathologic findings are seen in ischemic colitis, corresponding to the spectrum of clinical severity.
- Mildest form, mucosal and submucosal hemorrhage and edema are seen, possibly with mild necrosis or ulceration.
- With more severe ischemia, a pathologic picture resembling inflammatory bowel disease (i.e. chronic ulcerations, crypt abscesses and pseudopolyps) may be seen.
- In the most severe cases, transmural infarction with resulting perforation may be seen.
- After recovery, the muscularis propria may be replaced by fibrous tissue, resulting in a stricture.
- Following restoration of normal blood flow, reperfusion injury may contribute to the damage to the colon.
Images
Videos
{{#ev:youtube|LCwMQU7ylYg}}
References
- ↑ Rosenblum JD, Boyle CM, Schwartz LB (1997). "The mesenteric circulation. Anatomy and physiology". Surg Clin North Am. 77 (2): 289–306. PMID 9146713.
- ↑ Granger DN, Rutili G, McCord JM (1981). "Superoxide radicals in feline intestinal ischemia". Gastroenterology. 81 (1): 22–9. PMID 6263743.
- ↑ Brandt LJ, Boley SJ, Goldberg L, et al: Colitis in the elderly. Am J Gastroenterol 76:239, 1981.
- ↑ Washington, Christopher; Carmichael, Joseph (2012). "Management of Ischemic Colitis". Clinics in Colon and Rectal Surgery. 25 (04): 228–235. doi:10.1055/s-0032-1329534. ISSN 1531-0043.