Hyperkalemia electrocardiogram
| Resident Survival Guide |
|
Hyperkalemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hyperkalemia electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Hyperkalemia electrocardiogram |
|
Risk calculators and risk factors for Hyperkalemia electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.B.B.S. [2]
Overview
Extreme degrees of hyperkalemia are considered a medical emergency due to the risk of potentially fatal arrhythmias. The EKG is an important tool in evaluating a patient who has hyperkalemia as well as in diagnosing hyperkalemia. However, EKG changes do not always correlate with the degree of hyperkalemia. Some of the EKG changes that can be seen associated with hyperkalemia include peaked T waves, PR interval prolongation, QRS complex widening, absence of P waves, sine wave pattern and sinus arrest.
Electrocardiogram
Elevated potassium increases the activity of some potassium channels and speeds membrane repolarization. Hyperkalemia causes an overall membrane repolarization that inactivates many sodium channels. While the fast repolarization of the cardiac action potential causes the tenting of the T waves, the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS complex. With moderate hyperkalemia, there is reduction of the size of the P wave and development of tent-shaped T waves. Further hyperkalemia will lead to widening of the QRS complex, and the QRS complex may ultimately become sinusoidal in shape (sine wave pattern). Bradyarrhythmias, tachyarrhythmias and atrioventricular conduction defects can occur in severe hyperkalemia. ST segment changes consistent with current of injury that resemble ST segment changes in STEMI and pericarditis have been reported. These changes noted in the artificial kidney were reversible with dialysis.[1]
EKG Changes in Chronological Order
- Peaked T waves
- PR segment prolongation
- QRS widening
- Loss of P waves
- Accelerated junctional rhythm
- Sine wave pattern
- Ventricular fibrillation
- Asystole[2][3]
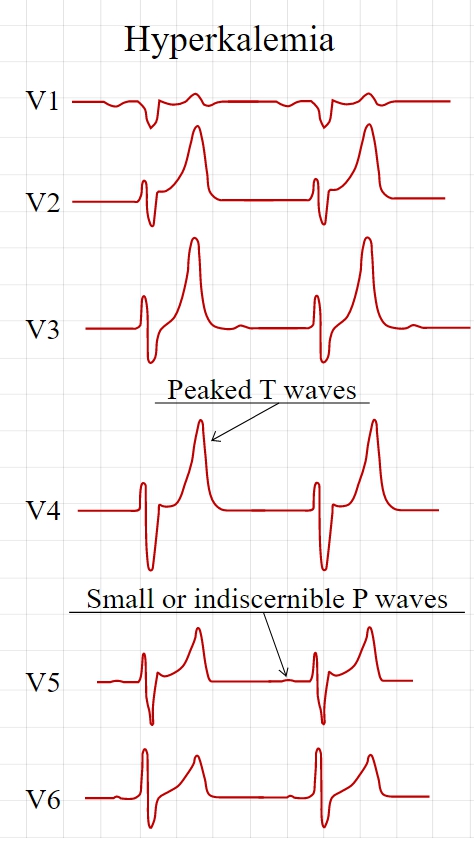
Peaked T waves
- Peaked T waves are the earliest sign of hyperkalemia.
- They occur when K > 5.5 meq/L.
- The differential diagnosis of this EKG change are bradycardia or stroke; however, prominent U waves and QTc prolongation are more consistent with stroke than hyperkalemia.
Intraventricular Conduction Defect
- It is observed when K > 6.5 meq/L.
- Interventricular conduction defect is reflected by wide QRS.
- There is a modest correlation of the QRS duration with serum potassium level.
- As the serum potassium level rises, the QRS complexes may resemble sine waves.
- Generally the widening is diffuse and there is no resemblance of the morphology of wide QRS to that of either LBBB or RBBB.
Decreased P wave Amplitude or Absence of P Wave
- Decreased P wave amplitude occurs when K is > 7.0 meq/L.
- The P wave may be absent when K is > 8.8 meq/L.
- The absence of the P waves can be explained by the fact that the impulses are still being generated in the SA node and are conducted to the ventricles through specialized atrial fibers without depolarizing the atrial muscle.
Sinus Arrest
- Moderate or severe hyperkalemia can cause sinus arrest. [4]
EKG Examples
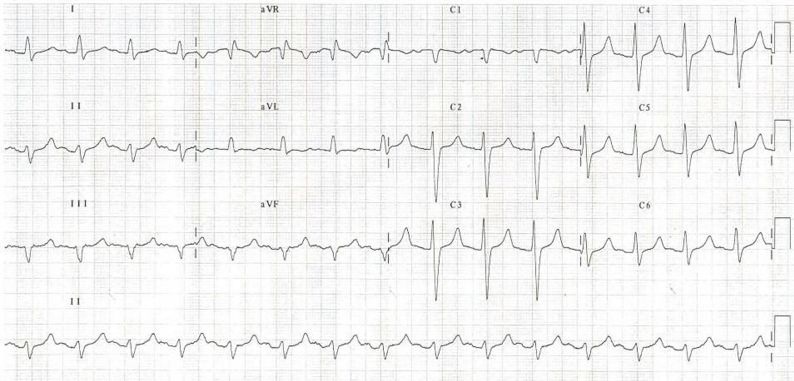
Shown below is an EKG demonstrating peaked T waves, loss of P wave and wide QRS complex depicting hyperkalemia.

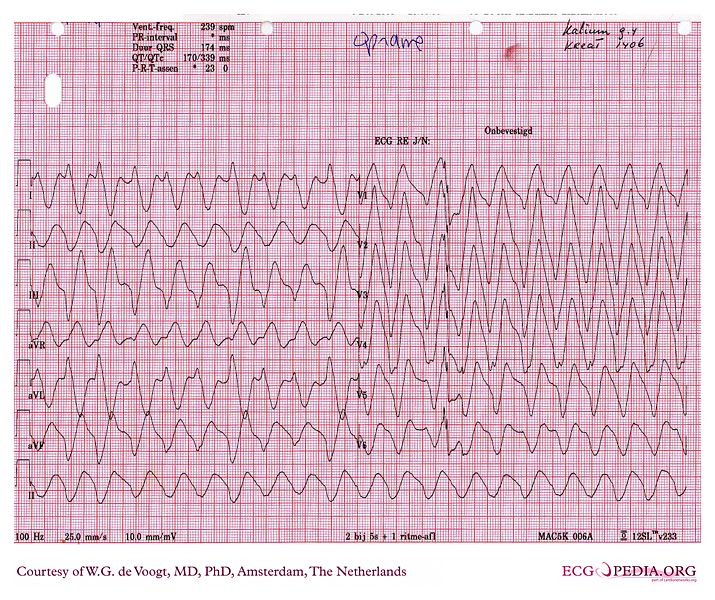
Shown below is an EKG demonstrating wide QRS complexes, tall peaked T waves an fusion of the QRS complex and the T wave.

Shown below is an EKG demonstrating tall, narrow and peaked T waves.

Shown below is an EKG demonstrating tall, narrow and peaked T waves.
Shown below is an EKG demonstrating sine wave pattern depicting severe hyperkalemia.
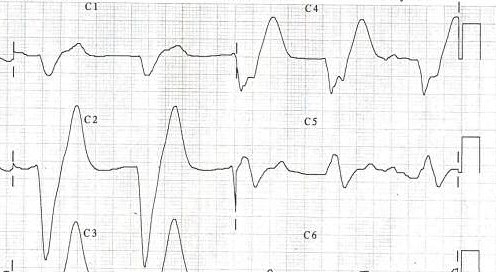
Shown below are a series of EKG images demonstrating interventricular conduction defect before, during and after treatment of hyperkalemia.
- Before treatment
- During treatment
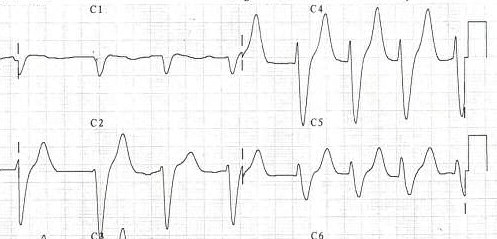
- After treatment
References
- ↑ LEVINE HD, WANZER SH, MERRILL JP (1956). "Dialyzable currents of injury in potassium intoxication resembling acute myocardial infarction or pericarditis". Circulation. 13 (1): 29–36. PMID 13277089.
- ↑ Petrov DB (2012). "Images in clinical medicine. An electrocardiographic sine wave in hyperkalemia". N Engl J Med. 366 (19): 1824. doi:10.1056/NEJMicm1113009. PMID 22571204.
- ↑ Parham WA, Mehdirad AA, Biermann KM, Fredman CS (2006). "Hyperkalemia revisited". Tex Heart Inst J. 33 (1): 40–7. PMC 1413606. PMID 16572868.
- ↑ Bonvini RF, Hendiri T, Anwar A (2006). "Sinus arrest and moderate hyperkalemia". Annales De Cardiologie Et D'angéiologie. 55 (3): 161–3. PMID 16792034. Unknown parameter
|month=ignored (help)