Hepatitis B epidemiology and demographics
|
Hepatitis B |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hepatitis B epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Hepatitis B epidemiology and demographics |
|
Risk calculators and risk factors for Hepatitis B epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Epidemiology and Demographics
Chronic Hepatitis B is a global public health issue. 350 million people worldwide are living with chronic Hepatitis B, including 1.2 million in the United States. The hepatitis B virus is very infectious; it is 50-100 times more infectious than the HIV virus.
Approximately 15%-25% of people with chronic Hepatitis B develop serious liver problems, which can include liver damage, cirrhosis, liver failure, or liver cancer.
Hepatitis B is caused by a virus that attacks the liver. The virus, which is called hepatitis B virus (HBV), can cause lifelong infection, cirrhosis (scarring) of the liver, liver cancer, liver failure, and death. In 2003, an estimated 73,000 people were infected with HBV. People of all ages get hepatitis B and about 5,000 die per year of sickness caused by HBV. HBV is spread when blood from an infected person enters the body of a person who is not infected. Healthcare personnel who have received hepatitis B vaccine and developed immunity to the virus are at virtually no risk for infection. For a susceptible person, the risk from a single needlestick or cut exposure to HBV-infected blood ranges from 6-30%. The annual number of occupational infections has decreased 95% since hepatitis B vaccine became available in 1982, from >10,000 in 1983 to <400 in 2001.
- Number of new infections per year has declined from an average of 260,000 in the 1980s to about 60,000 in 2004.
- Highest rate of disease occurs in 20-49-year-olds.
- Greatest decline has happened among children and adolescents due to routine hepatitis B vaccination.
- Estimated 1.25 million chronically infected Americans, of whom 20-30% acquired their infection in childhood.
In the United States, Asian and Pacific Islanders (APIs) make up less than 5% of the total population, but account for more than 50% of Americans living with chronic Hepatitis B. Despite the high rates of infection, many APIs are not tested for Hepatitis B and are unaware of their infection. As a result, chronic Hepatitis B and associated liver cancer in APIs is one of the most serious health disparities in the United States.
- In the United States, nearly 70% of APIs were born or have parents born in countries where Hepatitis B is common.
- Hepatitis B-related liver cancer incidence is highest among APIs and is a leading cause of cancer deaths in this population.
- The death rate from Hepatitis B among APIs is 7 times greater than deaths among whites.
- Knowledge of Hepatitis B varies greatly in the API community and many misconceptions exist. The lack of knowledge and awareness of the disease significantly contributes to the low testing rates in the API population.
- Limited English proficiency can be a significant barrier to seeking and receiving Hepatitis B related care and services.
Modes of Transmission
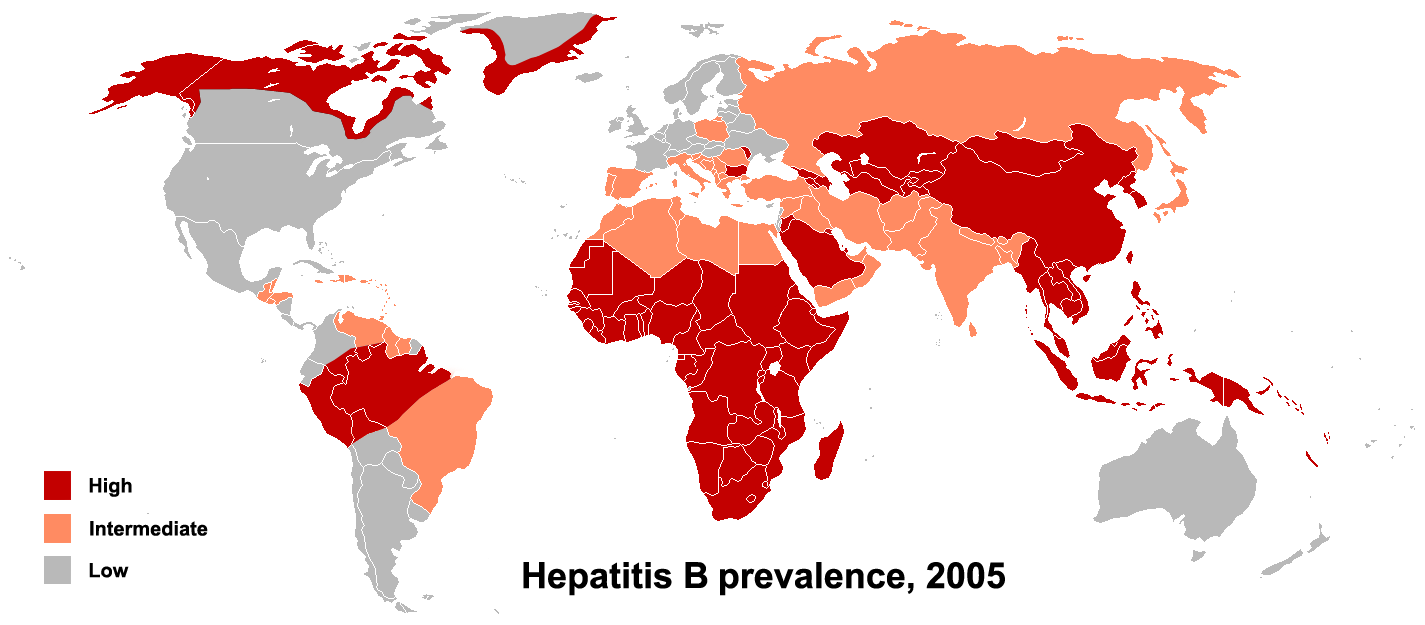
The primary method of transmission reflects the prevalence of chronic HBV infection in a given area. In low prevalence areas such as the continental United States and Western Europe, where less than 2% of the population is chronically infected, injection drug abuse and unprotected sex are the primary methods, although other factors may be important.[1] In moderate prevalence areas, which include Eastern Europe, Russia, and Japan, where 2-7% of the population is chronically infected, the disease is predominantly spread among children. In high prevalence areas such as China and South East Asia, transmission during childbirth is most common, although in other areas of high endemicity such as Africa, transmission during childhood is also a significant factor.[2] The prevalence of chronic HBV infection in areas of high endemicity is at least 8%.
Roughly 16-40% of unimmunized sexual partners of individuals with hepatitis B will be infected through sexual contact. The risk of transmission is closely related to the rate of viral replication in the infected individual at the time of exposure.
References
- ↑ Redd JT, Baumbach J, Kohn W; et al. (2007). "Patient-to-patient transmission of hepatitis B virus associated with oral surgery" (PDF). J Infect Dis. 195 (9): 1311&ndash, 4.
- ↑ name="pmid12616449">Alter MJ (2003). "Epidemiology and prevention of hepatitis B". Semin. Liver Dis. 23 (1): 39–46. doi:10.1055/s-2003-37583. PMID 12616449.