Group B streptococcal infection causes: Difference between revisions
No edit summary |
m (Changes made per Mahshid's request) |
||
| (3 intermediate revisions by one other user not shown) | |||
| Line 57: | Line 57: | ||
==Antimicrobial therapy== | ==Antimicrobial therapy== | ||
Streptococcus agalactiae treatment <ref>{{cite | :*'''Streptococcus agalactiae treatment''' (GBS-group B Streptococcus) | ||
::* 1. '''Early onset group B streptococcal infections'''<ref>{{cite web|title=group B Streptococcus infections|url=http://redbook.solutions.aap.org/book.aspx?bookid=1484}}</ref> | |||
:::* Preferred regimen: [[Penicillin G]] | :::* 1.1 '''Bacteremia or sepsis or pneumonia''' | ||
::::* 1.1.1 '''Empiric therapy''' | |||
::* | :::::* Preferred regimen: [[Ampicillin]] 150 mg/kg IV q12h for 10 days {{and}} [[Gentamicin]] 4 mg/kg IV q12h for 10 days-for infants born at ≥ 35 weeks gestation; [[Gentamicin]] 3 mg/kg IV q24h for 10 days-for infants born at < 35 weeks gestation | ||
:::* Preferred regimen: [[Penicillin G]] | ::::* 1.1.2 '''Definitive therapy''' | ||
:::::* Preferred regimen: [[Penicillin G]] 50,000-100,000 units/kg per day IV divided q12h for 10 days | |||
::* (3 | :::* 1.2 '''Meningitis''' | ||
:::* Preferred regimen: [[Penicillin G]] | ::::* 1.2.1 '''Empiric therapy''' | ||
:::::* Preferred regimen: [[Ampicillin]] 100-150 mg/kg IV q8h for 14-21 days {{and}} [[Gentamicin]] 4 mg/kg IV q24h for 14-21 days-for infants born at ≥ 35 weeks gestation; [[Gentamicin]] 3 mg/kg IV q24h for 14-21 days-for infants born at < 35 weeks gestation | |||
::* | ::::* 1.2.2 '''Definitive therapy''' | ||
:::* Preferred regimen: [[ | :::::* Preferred regimen: [[Penicillin G]] 250,000-450,000 units/kg per day IV divided q8h for 14-21 days | ||
::::::* Note: Cellulitis is the most frequent clinical manifestation of GBS-associated skin and soft tissue infections. | |||
:::: | ::* 2. '''Late onset group b streptococcus infections in neonates and young infants (age > 1 week and body weight ≥ 1 kg with normal renal function)'''<ref>{{cite web|title=group B Streptococcus infections|url=http://redbook.solutions.aap.org/book.aspx?bookid=1484}}</ref> | ||
:::: | :::* 2.1 Bacteremia without a focus | ||
:::: | ::::* 2.1.1 '''Empiric therapy''' | ||
:::: | :::::* Preferred regimen: [[Ampicillin]] IV for 10 days, [[Nafcillin]] IV for 10 days, ({{or}} [[Vancomycin]] IV for 10 days) {{and}} [[Gentamicin]] IV for 10 days ({{or}} [[Cefotaxime]] IV for 10 days) | ||
::::* 2.1.2 '''Definitive therapy''' | |||
:::::* Preferred regimen: [[Penicillin-G]] 75,000-150,000 units/kg per day IV divided q8h for 10 days | |||
:::* 2.2 '''Meningitis''' | |||
::::* 2.2.1 '''Empiric therapy''' | |||
:::::* Preferred regimen: [[Ampicillin]] IV for 14-21 days with or without [[Vancomycin]] IV for 14-21 day {{and}} [[Gentamicin]] IV for 14-21 days {{or}} [[Cefotaxime]] IV for 14-21 day | |||
::::* 2.2.2 '''Definitive therapy''' | |||
:::::* Preferred regimen: [[Penicillin-G]] 450,000-500,000 units/kg per day IV divided q6h for 14-21 days | |||
:::* 2.3 '''Cellulitis or adenitis''' | |||
::::* 2.3.1 '''Empiric therapy''' | |||
:::::* Preferred regimen: [[Nafcillin]] IV for 10-14 days ({{or}} [[Vancomycin IV for 10-14 days) {{and}} [[Gentamicin]] IV for 10-14 days ({{or}} [[Cefotaxime]] IV for 10-14 days) | |||
::::* 2.3.2 '''Definitive therapy''' | |||
:::::* Preferred regimen: [[Penicillin-G]] 75,000-150,000 units/kg per day IV divided q8h for 10-14 days | |||
:::* 2.4 '''Septic arthritis''' | |||
::::* 2.4.1 '''Empiric therapy''' | |||
:::::* Preferred regimen: [[Nafcillin]] IV for 14-21 days {{or}} [[Vancomycin]] IV for 14-21 days {{and}} [[Cefotaxime]] IV for 14-21 days | |||
::::* 2.4.2 '''Definitive therapy''' | |||
:::::* Preferred regimen: [[Penicillin-G]] 75,000-150,000 units/kg per day IV divided q8h for 14-21 days | |||
:::* 2.5 Osteomyelitis | |||
::::* 2.5.1 '''Empiric therapy''' | |||
:::::* Preferred regimen: [[Nafcillin]] IV for 21-28 days {{or}} [[Vancomycin]] IV for 21-28 days {{and}} [[Cefotaxime]] IV for 21-28 days | |||
::::* 2.5.2 '''Definitive therapy''' | |||
:::::* Preferred regimen: [[Penicillin-G]] 75,000-150,000 units/kg per day IV divided q8h for 21-28 days | |||
:::* 2.6 Urinary tract infection | |||
::::* 2.6.1 '''Empiric therapy''' | |||
:::::* Preferred regimen: [[Ampicillin]] IV for 10 days, [[Nafcillin]] IV for 10 days, ({{or}} [[Vancomycin]] IV for 10 days) {{and}} [[Gentamicin]] IV for 10 days ({{or}} [[Cefotaxime]] IV for 10 days) | |||
::::* 2.6.2 '''Definitive therapy''' | |||
:::::* Preferred regimen: [[Penicillin-G]] 75,000-150,000 units/kg per day IV divided q8h for 10 days | |||
:* '''Neonatal prophylaxis'''<ref name="pmid24446442">{{cite journal| author=Mukhopadhyay S, Dukhovny D, Mao W, Eichenwald EC, Puopolo KM| title=2010 perinatal GBS prevention guideline and resource utilization. | journal=Pediatrics | year= 2014 | volume= 133 | issue= 2 | pages= 196-203 | pmid=24446442 | doi=10.1542/peds.2013-1866 | pmc=PMC3904275 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24446442 }} </ref> | |||
::* Group B streptococcus infection (maternal dose for neonatal prophylaxis) | |||
:::* Preferred regimen: [[Penicillin-G]], [[Ampicillin]] 2 g IV initial dose, {{then}} 1 g q4h until delivery, [[Cefazolin]] ≥ 4h prior to delivery. | |||
==References== | ==References== | ||
| Line 85: | Line 111: | ||
[[Category:Streptococcaceae]] | [[Category:Streptococcaceae]] | ||
[[Category:Obstetrics]] | [[Category:Obstetrics]] | ||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
[[Category:Pediatrics]] | [[Category:Pediatrics]] | ||
[[Category:Neonatology]] | [[Category:Neonatology]] | ||
[[Category:Infectious Disease Project]] | |||
Latest revision as of 17:51, 18 September 2017
|
Group B Streptococcal Infection Microchapters |
|
Differentiating Group B Streptococcal Infection from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Group B streptococcal infection causes On the Web |
|
American Roentgen Ray Society Images of Group B streptococcal infection causes |
|
Directions to Hospitals Treating Group B streptococcal infection |
|
Risk calculators and risk factors for Group B streptococcal infection causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2]
Overview
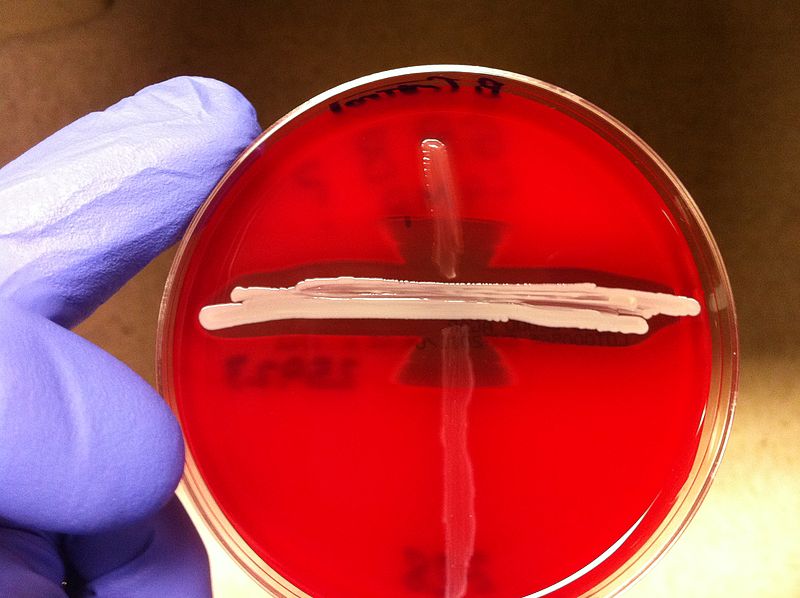
Group B Streptococcus (GBS) disease is caused by the infection with the bacterium GBS which is a beta hemolytic gram-positive streptococcus characterized by the presence of group B Lancefield antigen. GBS displays beta-hemolysis when cultured on a blood agar plate and produces zones of hemolysis that are only slightly larger than the colonies themselves. The species other name S. agalactiae, where "agalactiae" means "no milk", alludes to this. GBS hydrolyzes sodium hippurate and gives a positive response in the CAMP test. GBS is also sensitive to bile and will lyse in its presence. GBS is a species of the normal flora of the gut and female urogenital tract. The polysaccharide antiphagocytic capsule is this bacterium's main virulence factor.
Taxonomy
Cellular organisms; Bacteria; Firmicutes; Bacilli; Lactobacillales; Streptococcaceae; Streptococcus
Biology
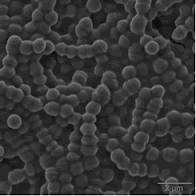
GBS is characterized by the following features:
- Gram-positive
- Cocci in pairs and short chains
- Group B Lancefield antigen
- Non-motile
- Catalase-negative
- Non-spore forming
- Polysaccharide antiphagocytic capsule (main virulence factor)
- Surface proteins
- Beta hemolysis
Identification
The CAMP test is an important test for identification. GBS are screened through this test. It is characterized by the presence of Lancefield antigen and by its ability to hydrolyze sodium hippurate.
GBS is also sensitive to bile, and will lyse in its presence.
Shown below is an image depicting an example of a positive CAMP test proving that GBS is present. The arrowhead formation on the Blood agarose gel, BAP (5% sheep blood) indicates that this bacteria is GBS.
Shown below is an image depicting colonies of GBS under microscope.
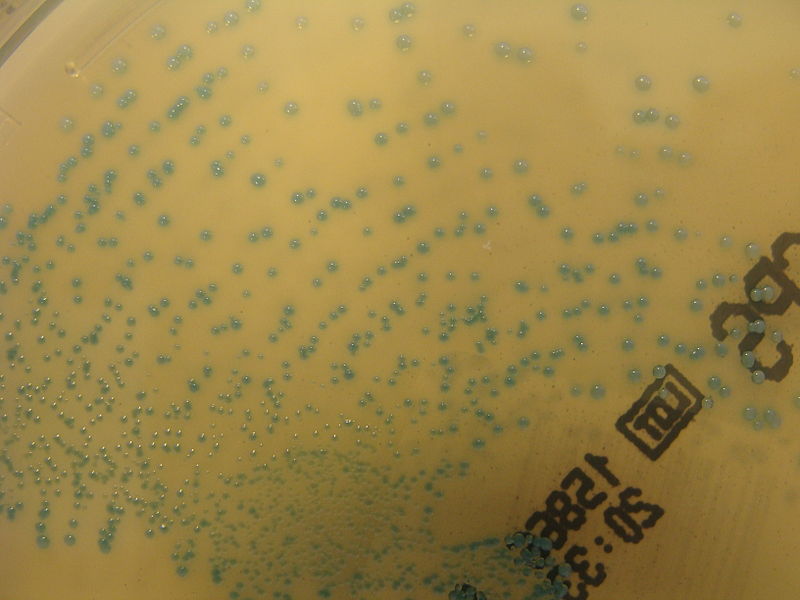
Shown below is an image depicting the growth of colonies of GBS on ChromID CPS chromogenic agar.
Shown below is an image depicting the growth of colonies of GBS on Columbia horse blood agar.
Gallery
-
Right elbow of a patient with group B Streptococcus (GBS) bacteremia, with localized edema and erythema. From Public Health Image Library (PHIL). [1]
-
Group-B streptococci (GBS) identified by CAMP test, which takes advantage of the capacity of GBS to produce this CAMP factor that most other hemolytic streptococci do not produce. From Public Health Image Library (PHIL). [1]
-
Quantitative difference in hemolytic reactivity seen on BAP with group-D Streptococci (left wedge), group-B Streptococci (middle wedge), and group-A Streptococci (right wedge) bacteria. From Public Health Image Library (PHIL). [1]
-
Clindamycin-resistant Group-B Streptococcus (GBS), also known as S. agalactiae. From Public Health Image Library (PHIL). [1]
Treatment
Antimicrobial therapy
- Streptococcus agalactiae treatment (GBS-group B Streptococcus)
- 1. Early onset group B streptococcal infections[2]
- 1.1 Bacteremia or sepsis or pneumonia
- 1.1.1 Empiric therapy
- Preferred regimen: Ampicillin 150 mg/kg IV q12h for 10 days AND Gentamicin 4 mg/kg IV q12h for 10 days-for infants born at ≥ 35 weeks gestation; Gentamicin 3 mg/kg IV q24h for 10 days-for infants born at < 35 weeks gestation
- 1.1.2 Definitive therapy
- Preferred regimen: Penicillin G 50,000-100,000 units/kg per day IV divided q12h for 10 days
- 1.2 Meningitis
- 1.2.1 Empiric therapy
- Preferred regimen: Ampicillin 100-150 mg/kg IV q8h for 14-21 days AND Gentamicin 4 mg/kg IV q24h for 14-21 days-for infants born at ≥ 35 weeks gestation; Gentamicin 3 mg/kg IV q24h for 14-21 days-for infants born at < 35 weeks gestation
- 1.2.2 Definitive therapy
- Preferred regimen: Penicillin G 250,000-450,000 units/kg per day IV divided q8h for 14-21 days
- Note: Cellulitis is the most frequent clinical manifestation of GBS-associated skin and soft tissue infections.
- 2. Late onset group b streptococcus infections in neonates and young infants (age > 1 week and body weight ≥ 1 kg with normal renal function)[3]
- 2.1 Bacteremia without a focus
- 2.1.1 Empiric therapy
- Preferred regimen: Ampicillin IV for 10 days, Nafcillin IV for 10 days, (OR Vancomycin IV for 10 days) AND Gentamicin IV for 10 days (OR Cefotaxime IV for 10 days)
- 2.1.2 Definitive therapy
- Preferred regimen: Penicillin-G 75,000-150,000 units/kg per day IV divided q8h for 10 days
- 2.2 Meningitis
- 2.2.1 Empiric therapy
- Preferred regimen: Ampicillin IV for 14-21 days with or without Vancomycin IV for 14-21 day AND Gentamicin IV for 14-21 days OR Cefotaxime IV for 14-21 day
- 2.2.2 Definitive therapy
- Preferred regimen: Penicillin-G 450,000-500,000 units/kg per day IV divided q6h for 14-21 days
- 2.3 Cellulitis or adenitis
- 2.3.1 Empiric therapy
- Preferred regimen: Nafcillin IV for 10-14 days (OR [[Vancomycin IV for 10-14 days) AND Gentamicin IV for 10-14 days (OR Cefotaxime IV for 10-14 days)
- 2.3.2 Definitive therapy
- Preferred regimen: Penicillin-G 75,000-150,000 units/kg per day IV divided q8h for 10-14 days
- 2.4 Septic arthritis
- 2.4.1 Empiric therapy
- Preferred regimen: Nafcillin IV for 14-21 days OR Vancomycin IV for 14-21 days AND Cefotaxime IV for 14-21 days
- 2.4.2 Definitive therapy
- Preferred regimen: Penicillin-G 75,000-150,000 units/kg per day IV divided q8h for 14-21 days
- 2.5 Osteomyelitis
- 2.5.1 Empiric therapy
- Preferred regimen: Nafcillin IV for 21-28 days OR Vancomycin IV for 21-28 days AND Cefotaxime IV for 21-28 days
- 2.5.2 Definitive therapy
- Preferred regimen: Penicillin-G 75,000-150,000 units/kg per day IV divided q8h for 21-28 days
- 2.6 Urinary tract infection
- 2.6.1 Empiric therapy
- Preferred regimen: Ampicillin IV for 10 days, Nafcillin IV for 10 days, (OR Vancomycin IV for 10 days) AND Gentamicin IV for 10 days (OR Cefotaxime IV for 10 days)
- 2.6.2 Definitive therapy
- Preferred regimen: Penicillin-G 75,000-150,000 units/kg per day IV divided q8h for 10 days
- Neonatal prophylaxis[4]
- Group B streptococcus infection (maternal dose for neonatal prophylaxis)
- Preferred regimen: Penicillin-G, Ampicillin 2 g IV initial dose, THEN 1 g q4h until delivery, Cefazolin ≥ 4h prior to delivery.
References
- ↑ 1.0 1.1 1.2 1.3 "Public Health Image Library (PHIL)".
- ↑ "group B Streptococcus infections".
- ↑ "group B Streptococcus infections".
- ↑ Mukhopadhyay S, Dukhovny D, Mao W, Eichenwald EC, Puopolo KM (2014). "2010 perinatal GBS prevention guideline and resource utilization". Pediatrics. 133 (2): 196–203. doi:10.1542/peds.2013-1866. PMC 3904275. PMID 24446442.

![Right elbow of a patient with group B Streptococcus (GBS) bacteremia, with localized edema and erythema. From Public Health Image Library (PHIL). [1]](/images/5/58/Group_A_streptococcus28.jpeg)
![Group-B streptococci (GBS) identified by CAMP test, which takes advantage of the capacity of GBS to produce this CAMP factor that most other hemolytic streptococci do not produce. From Public Health Image Library (PHIL). [1]](/images/5/57/Group_A_streptococcus05.jpeg)
![Quantitative difference in hemolytic reactivity seen on BAP with group-D Streptococci (left wedge), group-B Streptococci (middle wedge), and group-A Streptococci (right wedge) bacteria. From Public Health Image Library (PHIL). [1]](/images/f/f5/Group_A_streptococcus04.jpeg)
![Clindamycin-resistant Group-B Streptococcus (GBS), also known as S. agalactiae. From Public Health Image Library (PHIL). [1]](/images/b/bb/Group_A_streptococcus01.jpeg)