Glaucoma: Difference between revisions
(→Drugs) |
|||
| Line 18: | Line 18: | ||
==Diagnosis== | ==Diagnosis== | ||
====Cannabis==== | ====Cannabis==== | ||
Revision as of 05:03, 23 August 2012
For patient information click here
| Glaucoma | |
 | |
|---|---|
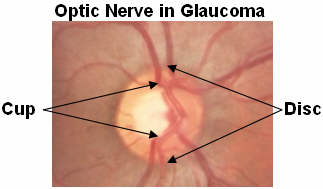
| The pink rim of disc contains nerve fibers. The white cup is a pit with no nerve fibers. As glaucoma advances, the cup enlarges until it occupies most of the disc area. Courtesy AgingEye Times | |
| ICD-10 | H40-H42 |
| ICD-9 | 365 |
| DiseasesDB | 5226 |
| MeSH | D005901 |
|
Glaucoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glaucoma On the Web |
|
American Roentgen Ray Society Images of Glaucoma |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]
Diagnosis
Cannabis
Studies in the 1970s showed that marijuana, when smoked, lowers intraocular pressure.[1] In an effort to determine whether marijuana, or drugs derived from marijuana, might be effective as a glaucoma treatment, the US National Eye Institute supported research studies from 1978 to 1984. These studies demonstrated that some derivatives of marijuana lowered intraocular pressure when administered orally, intravenously, or by smoking, but not when topically applied to the eye. Many of these studies demonstrated that marijuana — or any of its components — could safely and effectively lower intraocular pressure more than a variety of drugs then on the market. In 2003, the American Academy of Ophthalmology released a position statement asserting that "no scientific evidence has been found that demonstrates increased benefits and/or diminished risks of marijuana use to treat glaucoma compared with the wide variety of pharmaceutical agents now available."[1]
The first patient in the United States federal government's Compassionate Investigational New Drug program, Robert Randall, was afflicted with glaucoma and had successfully fought charges of marijuana cultivation because it was deemed a medical necessity (U.S. v. Randall) in 1976.[2]
Surgery
Surgery is the primary therapy for those with congenital glaucoma.[3] Both laser and conventional surgeries are performed. Generally, these operations are a temporary solution, as there is no cure for glaucoma as of yet.
Canaloplasty
Canaloplasty is an advanced, nonpenetrating procedure designed to enhance and restore the eye’s natural drainage system to provide sustained reduction of IOP. Canaloplasty utilizes breakthrough microcatheter technology in a simple and minimally invasive procedure. To perform a canaloplasty, a doctor will create a tiny incision to gain access to a canal in the eye. A microcatheter will circumnavigate the canal around the iris, enlarging the main drainage channel and its smaller collector channels through the injection of a sterile, gel-like material called viscoelastic. The catheter is then removed and a suture is placed within the canal and tightened. By opening the canal, the pressure inside the eye will be relieved.
Laser surgery
Laser trabeculoplasty may be used to treat open angle glaucoma. It is a temporary solution, not a cure. A 50 μm argon laser spot is aimed at the trabecular meshwork to stimulate opening of the mesh to allow more outflow of aqueous fluid. Usually, half of the angle is treated at a time. Traditional laser trabeculoplasty utilizes a thermal argon laser. The procedure is called argon laser trabeculoplasty or ALT. A newer type of laser trabeculoplasty uses a "cold" (non-thermal) laser to stimulate drainage in the trabecular meshwork. This newer procedure is call selective laser trabeculoplasty or SLT. Studies show that SLT is as effective as ALT at lowering eye pressure. In addition, SLT may be repeated three to four times, whereas ALT can usually be repeated only once.
Laser peripheral iridotomy may be used in patients susceptible to or affected by angle closure glaucoma. During laser iridotomy, laser energy is used to make a small full-thickness opening in the iris. This opening equalizes the pressure between the front and back of the iris, causing the iris to move backward. This uncovers the trabecular meshwork. In some cases of intermittent or short-term angle closure this may lower the eye pressure. Laser iridotomy reduces the risk of developing an attack of acute angle closure. In most cases it also reduces the risk of developing chronic angle closure or gradual adhesion of the iris to the trabecular meshwork.
Trabeculectomy
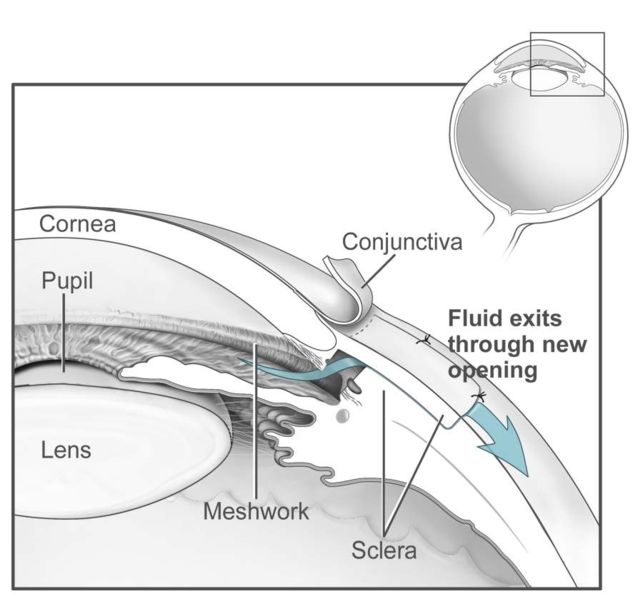
The most common conventional surgery performed for glaucoma is the trabeculectomy. Here, a partial thickness flap is made in the scleral wall of the eye, and a window opening made under the flap to remove a portion of the trabecular meshwork. The scleral flap is then sutured loosely back in place. This allows fluid to flow out of the eye through this opening, resulting in lowered intraocular pressure and the formation of a bleb or fluid bubble on the surface of the eye. Scarring can occur around or over the flap opening, causing it to become less effective or lose effectiveness altogether. One person can have multiple surgical procedures of the same or different types.
Glaucoma drainage implants
There are also several different glaucoma drainage implants. These include the original Molteno implant (1966), the Baerveldt tube shunt, or the valved implants, such as the Ahmed glaucoma valve implant and the later generation pressure ridge Molteno implants. These are indicated for glaucoma patients not responding to maximal medical therapy, with previous failed guarded filtering surgery (trabeculectomy). The flow tube is inserted into the anterior chamber of the eye and the plate is implanted underneath the conjunctiva to allow flow of aqueous fluid out of the eye into a chamber called a bleb. The Express mini-implant is currently being used as a modification of the standard trabeculectomy technique, and is a non-valved conduit between the anterior chamber and the space under the scleral flap[4].
- The first-generation Molteno and other non-valved implants sometimes require the ligation of the tube until the bleb formed is mildly fibrosed and water-tight[5]This is done to reduce postoperative hypotony -- sudden drops in postoperative intraocular pressure (IOP).
- Valved implants such as the Ahmed glaucoma valve attempt to control postoperative hypotony by using a mechanical valve. Studies show that in severe cases of glaucoma, double plate Molteno implants are associated with lower mean IOP in the long term compared to the Ahmed glaucoma valve [6]
- Second and third generation Molteno implants incorporate a biological valve and studies show considerable improvement in postoperative outcome over the older style Ahmed and Molteno implants.
The ongoing scarring over the conjunctival dissipation segment of the shunt may become too thick for the aqueous humor to filter through. This may require preventive measures using anti-fibrotic medication like 5-fluorouracil (5-FU) or mitomycin-C (during the procedure), or additional surgery.
Major studies
- Advanced Glaucoma Intervention Study (AGIS) - large American National Eye Institute (NEI) sponsored study designed "to assess the long-range outcomes of sequences of interventions involving trabeculectomy and argon laser trabeculoplasty in eyes that have failed initial medical treatment for glaucoma." It recommends different treatments based on race.
- Early Manifest Glaucoma Trial (EMGT) -Another NEI study found that immediately treating people who have early stage glaucoma can delay progression of the disease.
- Ocular Hypertension Treatment Study (OHTS) -NEI study findings: "...Topical ocular hypotensive medication was effective in delaying or preventing onset of Primary Open Angle Glaucoma (POAG) in individuals with elevated Intraocular Pressure (IOP). Although this does not imply that all patients with borderline or elevated IOP should receive medication, clinicians should consider initiating treatment for individuals with ocular hypertension who are at moderate or high risk for developing POAG."
- Blue Mountains Eye Study "The Blue Mountains Eye Study was the first large population-based assessment of visual impairment and common eye diseases of a representative older Australian community sample." Risk factors for glaucoma and other eye disease were determined.
See also
- List of eye diseases and disorders
- Ocular hypertension
- Glaucoma valves
- Mansour F. Armaly
- Laszlo Z. Bito
- Charles D. Phelps
- American Glaucoma Society
References
- ↑ 1.0 1.1 American Academy of Ophthalmology. Complementary Therapy Assessment: Marijuana in the Treatment of Glaucoma. Retrieved August 2, 2006.
- ↑ http://blogs.salon.com/0002762/stories/2005/02/18/irvRosenbergAndTheCompassi.html
- ↑ "Glaucoma, Congenital: GLC3 Buphthalmos." OMIM - Online Mendelian Inheritance in Man. Accessed October 17, 2006.
- ↑ Maris PJ, Jr., Ishida K, Netland PA. Comparison of trabeculectomy with Ex-PRESS miniature glaucoma device implanted under scleral flap. J Glaucoma 2007 January;16(1):14-9
- ↑ Molteno AC, Polkinghorne PJ, Bowbyes JA. The vicryl tie technique for inserting a draining implant in the treatment of secondary glaucoma. Aust N Z J Ophthalmol. 1986 Nov;14(4):343-54 [1]
- ↑ Ayyala RS, Zurakowski D et al. Comparison of double-plate Molteno and Ahmed glaucoma valve in patients with advanced uncontrolled glaucoma. Ophthalmic Surg Lasers. 2002 Mar-Apr;33(2):94-101.[2].
External links
- International Glaucoma Association A charity for people with glaucoma.
- Glaucoma Resource Guide from the National Eye Institute (NEI).
- Global Association of International Glaucoma Societies - featuring a hymn about the successful treatment of glaucoma
- Glaucoma Research Foundation
- "Glaucoma - What is Glaucoma?". NLM. Retrieved 2007-04-21. video
- Nonprofit Foundation for Glaucoma
- National Glaucoma Research
- DJO | Digital Journal of Ophthalmology
- Lions Eye Institute, Perth, Australia
- Improving Glaucoma Naturally
ca:Glaucoma da:Grøn stær de:Glaukom eo:Glaŭkomo hr:Glaukom it:Glaucoma (medicina) he:גלאוקומה ms:Glaukoma nl:Glaucoom no:Glaukom sr:Глауком fi:Glaukooma sv:Glaukom