Giardia lamblia: Difference between revisions
Gerald Chi- (talk | contribs) m (→Microscopy) |
Ahmed Younes (talk | contribs) |
||
| (8 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{Giardiasis}} | |||
{{Taxobox | {{Taxobox | ||
| color = khaki | | color = khaki | ||
| Line 15: | Line 16: | ||
| binomial_authority = (Kunstler, 1882) | | binomial_authority = (Kunstler, 1882) | ||
}} | }} | ||
{{ | __NOTOC__ | ||
{{About0|Giardiasis}} | |||
{{CMG}} | |||
==Overview== | ==Overview== | ||
'''''Giardia lamblia''''' (synonymous with '''''Lamblia intestinalis''''' and '''''Giardia duodenalis''''') is a [[flagellate]]d [[protozoa]]n [[parasite]] that is responsible for the development of giardiasis. | |||
''''' | ==Higher Order Classification== | ||
''Eukaryota'', ''Diplomonadida'' group, ''Diplomonadida'', ''Hexamitidae'', ''Giardiinae'', ''Giardia'', ''G. lamblia'' | |||
==Natural Reservoir== | |||
*Giardia affects humans and animals, such as cats, dogs, cows, beavers, deer, and sheep. | |||
== | ==Microbiological Characteristicsc== | ||
Giardia | *''Giardia lamblia'' is a flagellated, microaerophilic parasite. | ||
*The trophozoite form of G. lamblia is pear-shaped and has a unique morphology that includes two identical nuclei, a ventral disc for adhesion to the host intestine, and flagella. | |||
==Genome== | |||
*''G. lamblia'' genome consists of 1.2 million base pairs (average GC content: 46%).<ref name="pmid1840670">{{cite journal| author=Le Blancq SM, Kase RS, Van der Ploeg LH| title=Analysis of a Giardia lamblia rRNA encoding telomere with [TAGGG]n as the telomere repeat. | journal=Nucleic Acids Res | year= 1991 | volume= 19 | issue= 20 | pages= 5790 | pmid=1840670 | doi= | pmc=PMC328996 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1840670 }} </ref> | |||
*The genome pairs are distributed across five linear chromosomes.<ref name="pmid1840670">{{cite journal| author=Le Blancq SM, Kase RS, Van der Ploeg LH| title=Analysis of a Giardia lamblia rRNA encoding telomere with [TAGGG]n as the telomere repeat. | journal=Nucleic Acids Res | year= 1991 | volume= 19 | issue= 20 | pages= 5790 | pmid=1840670 | doi= | pmc=PMC328996 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1840670 }} </ref> | |||
*Similar to other eukaryotes, each chromosome is flanked by the telomere sequence (5’TAGGG3’).<ref name="pmid1840670">{{cite journal| author=Le Blancq SM, Kase RS, Van der Ploeg LH| title=Analysis of a Giardia lamblia rRNA encoding telomere with [TAGGG]n as the telomere repeat. | journal=Nucleic Acids Res | year= 1991 | volume= 19 | issue= 20 | pages= 5790 | pmid=1840670 | doi= | pmc=PMC328996 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1840670 }} </ref> | |||
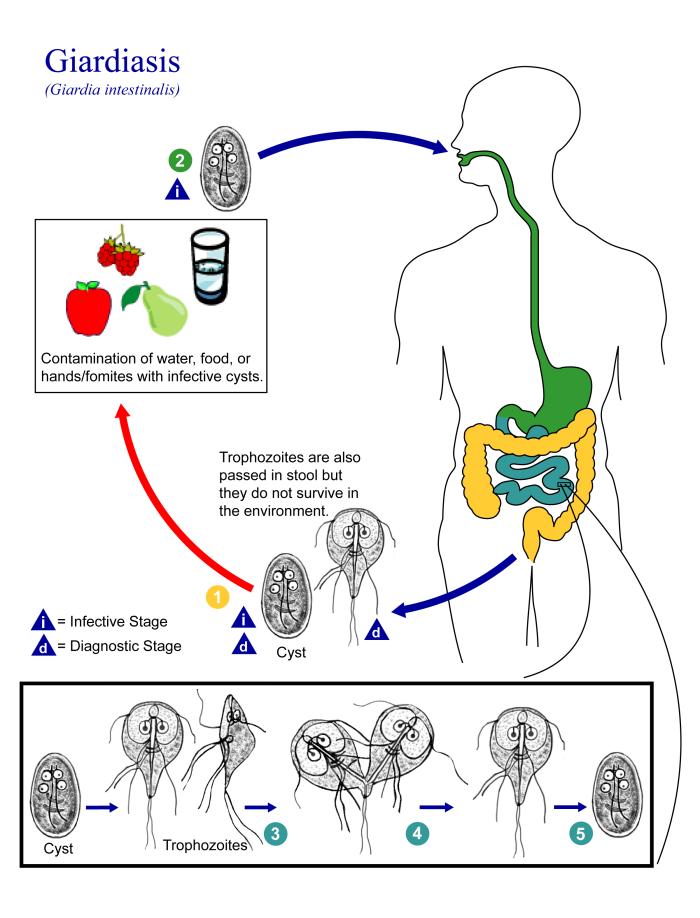
==Life cycle== | ==Life cycle== | ||
[[Image:Giardia lamblia life cycle.jpg| | [[Image:Giardia lamblia life cycle.jpg|right|thumb|Parasite life cycle.]] | ||
''Giardia'' belongs among the [[diplomonad]]s. | ''Giardia'' belongs among the [[diplomonad]]s. | ||
===Non-infective Cyst=== | |||
*The life cycle begins with a noninfective cyst being excreted with faeces of an infected individual. Once out in the environment, the cyst becomes infective. | |||
*A distinguishing characteristic of the cyst is 4 nuclei and a retracted cytoplasm. | |||
===Trophozoite=== | |||
*Once ingested by a host, the trophozoite emerges to an active state of feeding and motility. | |||
*After the feeding stage, the trophozoite undergoes asexual replication through longitudinal binary fission. | |||
*The resulting trophozoites and cysts then pass through the digestive system in the feces. | |||
*While the trophozoites may be found in the feces, only the cysts are capable of surviving outside of the host. | |||
*Distinguishing features of the trophozoites are large karyosomes and lack of peripheral chromatin, giving the two nuclei a halo appearance. | |||
<gallery> | |||
Giardia | Image: Giardiasis09.jpeg| SEM depicts the dorsal surface of a Giardia protozoan, isolated from a rat’s intestine. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Giardiasis08.jpeg| SEM depicts the mucosal surface of the small intestine of a gerbil infested with Giardia sp. protozoa. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
Image: Giardiasis07.jpeg| SEM depicts a Giardia lamblia protozoan in a late stage of cell division that was about to become two separate organisms, producing a heart-shaped form. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
Image: Giardiasis06.jpeg| SEM depicts the ventral surface of a Giardia muris trophozoite. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
== | Image: Giardiasis05.jpeg| SEM depicts dorsal surface of a Giardia protozoan, isolated from a rat’s intestine. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Giardiasis04.jpeg|SEM depicts some of the ultrastructural morphologic details of an oblong-shaped Giardia sp. protozoan cyst. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
Image: Giardiasis03.jpeg|SEM depicts the ventral surface of a Giardia muris trophozoite that had settled atop the mucosal surface of a rat’s intestine. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
Image: Giardiasis02.jpeg|SEM depicts a Giardia lamblia protozoan that was about to become two separate organisms, as it was caught in a late stage of cell division. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
Image: Giardiasis01.jpeg|SEM depicts a Giardia muris protozoan adhering itself to the microvillous border of an intestinal epithelial cell. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
Image: Giardiasis10.jpeg| This photomicrograph depicts Giardia lamblia parasites using indirect immunofluorescence test for giardiasis. <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp From Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | |||
</gallery> | |||
==Differential diagnosis== | |||
Giardia lamblia infection must be differentiated from other causes of viral, bacterial, and parasitic gastroentritis. | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | |||
! colspan="3" rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Organism | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Age predilection | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Travel History | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Incubation Size (cell) | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Incubation Time | |||
! colspan="3" align="center" style="background:#4479BA; color: #FFFFFF;"|History and Symptoms | |||
! colspan="4" align="center" style="background:#4479BA; color: #FFFFFF;"|Diarrhea type8 | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Food source | |||
! rowspan="2" align="center" style="background:#4479BA; color: #FFFFFF;"|Specific consideration | |||
|- | |||
!style="background:#4479BA; color: #FFFFFF|Fever | |||
!style="background:#4479BA; color: #FFFFFF|N/V | |||
!style="background:#4479BA; color: #FFFFFF|Cramping Abd Pain | |||
!style="background:#4479BA; color: #FFFFFF|Small Bowel | |||
!style="background:#4479BA; color: #FFFFFF|Large Bowel | |||
!style="background:#4479BA; color: #FFFFFF|Inflammatory | |||
!style="background:#4479BA; color: #FFFFFF|Non-inflammatory | |||
|- | |||
| rowspan="4" align="center" style="background:#4479BA; color: #FFFFFF;"|'''Viral''' | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Rotavirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<2 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<10<sup>2</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Mostly in day cares, most common in winter. | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Norovirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any age | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10 -10<sup>3</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24-48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Most common cause of gastroenteritis, abdominal tenderness, | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Adenoviridae|Adenovirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<2 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>5</sup> -10<sup>6</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |8-10 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |No seasonality | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Astrovirus]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<5 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |72-96 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Seafood | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Mostly during winter | |||
|- | |||
| rowspan="11" align="center" style="background:#4479BA; color: #FFFFFF;"|'''Bacterial''' | |||
| rowspan="5" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Escherichia coli]]'' | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[ETEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any age | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>8</sup> -10<sup>10</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Causes travelers diarrhea, contains heat-labile toxins (LT) and heat-stable toxins (ST) | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EPEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<1 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>†</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |6-12 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Raw beef and chicken | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EIEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>†</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Hamburger meat and unpasteurized milk | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Similar to [[shigellosis]], can cause bloody diarrhea | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EHEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10 | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |3-4 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked or raw hamburger (ground beef) | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Known as ''[[Escherichia coli O157:H7|E. coli]]'' [[Escherichia coli O157:H7|O157:H7]], can cause [[Hemolytic-uremic syndrome|HUS]]/[[TTP]]. | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[EAEC]] | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>10</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |8-18 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause prolonged or persistent diarrhea in children | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Salmonella|Salmonella sp.]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |6 to 72 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Meats, poultry, eggs, milk and dairy products, fish, shrimp, spices, yeast, coconut, sauces, freshly prepared salad. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Can cause [[salmonellosis]] or [[typhoid fever]]. | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Shigella|Shigella sp.]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10 - 200 | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |8-48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Raw foods, for example, lettuce, salads (potato, tuna, shrimp, macaroni, and chicken) | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Some strains produce enterotoxin and Shiga toxin similar to those produced by E. coli O157:H7 | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Campylobacter|Campylobacter sp.]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<5 y, 15-29 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>4</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-5 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked poultry products, unpasteurized milk and cheeses made from unpasteurized milk, vegetables, seafood and contaminated water. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause [[bacteremia]], [[Guillain-Barré syndrome]] (GBS), [[Hemolytic-uremic syndrome|hemolytic uremic syndrome]] (HUS) and recurrent [[colitis]] | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Yersinia enterocolitica]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<10 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>4</sup> -10<sup>6</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1-11 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Meats (pork, beef, lamb, etc.), oysters, fish, crabs, and raw milk. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause [[reactive arthritis]]; [[glomerulonephritis]]; [[endocarditis]]; [[erythema nodosum]]. | |||
can mimic [[appendicitis]] and mesenteric [[lymphadenitis]]. | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Clostridium perfringens]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |> 10<sup>6</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |16 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Meats (especially beef and poultry), meat-containing products (e.g., gravies and stews), and Mexican foods. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Can survive high heat, | |||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Vibrio cholerae]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10<sup>6</sup>-10<sup>10</sup> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |24-48 h | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Seafoods, including molluscan shellfish (oysters, mussels, and clams), crab, lobster, shrimp, squid, and finfish. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Hypotension]], [[tachycardia]], decreased [[Turgor|skin turgor]]. Rice-water stools | |||
|- | |||
| rowspan="7" align="center" style="background:#4479BA; color: #FFFFFF;"|'''Parasites''' | |||
| rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Protozoa | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Giardia lamblia]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-5 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 cyst | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1-2 we | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Contaminated water | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause [[malabsorption syndrome]] and severe [[weight loss]] | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Entamoeba histolytica]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |4-11 y | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |<10 cysts | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-4 we | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Contaminated water and raw foods | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause intestinal amebiasis and amebic liver abscess | |||
|- | |||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Cryptosporidium parvum]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10-100 oocysts | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |7-10 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Juices and milk | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause copious diarrhea and [[dehydration]] in patients with [[AIDS]] especially with 180 > [[CD4|CD<sub>4</sub>]] | |||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Cyclospora cayetanensis]]'' | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |10-100 oocysts | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |7-10 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Fresh produce, such as raspberries, basil, and several varieties of lettuce. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |More common in rainy areas | |||
|- | |- | ||
| | | rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Helminths | ||
| | |style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Trichinella]]'' [[Trichinella|spp]] | ||
| | |style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Two viable larvae (male and female) | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1-4 we | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked meats | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |More common in hunters or people who eat traditionally uncooked meats | |||
|- | |- | ||
| | |style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Taenia (tapeworm)|Taenia]]'' [[Taenia (tapeworm)|spp]] | ||
| | |style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | ||
| | |style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 larva or egg | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |2-4 m | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Undercooked beef and pork | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Neurocysticercosis]]: Cysts located in the brain may be asymptomatic or [[seizures]], increased [[intracranial pressure]], [[headache]]. | |||
|- | |- | ||
| | |style="padding: 5px 5px; background: #DCDCDC;" align="center" |''[[Diphyllobothrium|Diphyllobothrium latum]]'' | ||
| | |style="padding: 5px 5px; background: #F5F5F5;" align="center" |Any ages | ||
| | |style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |1 larva | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |15 d | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |- | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Raw or undercooked fish. | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |May cause vitamin B<sub>12</sub> deficiency | |||
|} | |} | ||
<br><br> | |||
<small><small> | |||
8'''Small bowel diarrhea''': watery, voluminous with less than 5 WBC/high power field | |||
'''Large bowel diarrhea''': Mucousy and/or bloody with less volume and more than 10 WBC/high power field<br> | |||
† It could be as high as 1000 based on patient's immunity system. | |||
</small></small> | |||
== | '''The table below summarizes the findings that differentiate inflammatory causes of chronic diarrhea'''<ref name="pmid8209928">{{cite journal| author=Konvolinka CW| title=Acute diverticulitis under age forty. | journal=Am J Surg | year= 1994 | volume= 167 | issue= 6 | pages= 562-5 | pmid=8209928 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8209928 }} </ref><ref name="pmid16151544">{{cite journal| author=Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR et al.| title=Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. | journal=Can J Gastroenterol | year= 2005 | volume= 19 Suppl A | issue= | pages= 5A-36A | pmid=16151544 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16151544 }} </ref><ref name="pmid16698746">{{cite journal| author=Satsangi J, Silverberg MS, Vermeire S, Colombel JF| title=The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. | journal=Gut | year= 2006 | volume= 55 | issue= 6 | pages= 749-53 | pmid=16698746 | doi=10.1136/gut.2005.082909 | pmc=1856208 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16698746 }} </ref><ref name="pmid12700377">{{cite journal| author=Haque R, Huston CD, Hughes M, Houpt E, Petri WA| title=Amebiasis. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 16 | pages= 1565-73 | pmid=12700377 | doi=10.1056/NEJMra022710 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12700377 }} </ref><ref name="pmid12700377">{{cite journal| author=Haque R, Huston CD, Hughes M, Houpt E, Petri WA| title=Amebiasis. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 16 | pages= 1565-73 | pmid=12700377 | doi=10.1056/NEJMra022710 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12700377 }} </ref> | ||
{| class="wikitable" | |||
!Cause | |||
!History | |||
!Laboratory findings | |||
!Diagnosis | |||
!Treatment | |||
|- | |||
|[[Diverticulitis]] | |||
| | |||
* [[Bloody diarrhea]] | |||
* Left lower quadrant [[abdominal pain]] | |||
* [[Abdominal tenderness]] on [[physical examination]] | |||
* Low grade [[fever]] | |||
| | |||
* [[Leukocytosis]] | |||
* Elevated serum [[amylase]] and [[lipase]] | |||
* [[Sterile]] [[pyuria]] on [[urinalysis]] | |||
|Abdominal [[CT scan]] with oral and intravenous [[Contrast medium|(IV) contrast]] | |||
|bowel rest, [[Intravenous fluids|IV fluid]] resuscitation, and [[Broad-spectrum antibiotic|broad-spectrum antimicrobial therapy]] which covers [[Anaerobic organism|anaerobic]] [[bacteria]] and [[gram-negative]] [[Bacteria|rods]] | |||
|- | |||
|[[Ulcerative colitis]] | |||
| | |||
* [[Diarrhea]] mixed with blood and [[mucus]], of gradual onset. | |||
* Signs of [[weight loss]] | |||
* [[Rectal pain|Rectal urgency]] | |||
* [[Tenesmus]] | |||
* [[Blood]] is often noticed on underwear | |||
* Different degrees of [[abdominal pain]] | |||
| | |||
* [[Anemia]] | |||
* [[Thrombocytosis]] | |||
* A high [[platelet]] count | |||
* Elevated [[ESR]] (>30mm/hr) | |||
* Low [[albumin]] | |||
|[[Endoscopy]] | |||
|Induction of [[Remission (medicine)|remission]] with [[mesalamine]] and [[corticosteroids]] followed by the administration of [[sulfasalazine]] and [[Mercaptopurine|6-Mercaptopurine]] depending on the severity of the [[disease]]. | |||
|- | |||
|[[Entamoeba histolytica]] | |||
| | |||
* [[Abdominal cramps]] | |||
* [[Diarrhea]] | |||
** Passage of 3 - 8 semiformed [[stools]] per day | |||
** Passage of soft [[stools]] with [[mucus]] and occasional [[blood]] | |||
* [[Fatigue]] | |||
* [[Intestinal]] gas (excessive [[flatus]]) | |||
* [[Rectal pain]] while having a [[bowel movement]] ([[tenesmus]]) | |||
* Unintentional [[weight loss]] | |||
|cysts shed with the stool | |||
|detects ameba [[DNA]] in feces | |||
|[[Amebic dysentery]] | |||
* [[Metronidazole]] 500-750mg three times a day for 5-10 days | |||
* [[Tinidazole]] 2g once a day for 3 days is an alternative to [[metronidazole]] | |||
Luminal amebicides for ''[[E. histolytica]]'' in the [[colon]]: | |||
* [[Paromomycin]] 500mg three times a day for 10 days | |||
* [[Diloxanide furoate]] 500mg three times a day for 10 days | |||
* [[Iodoquinol]] 650mg three times a day for 20 days | |||
For [[Amoebiasis|amebic liver abscess]]: | |||
* [[Metronidazole]] 400mg three times a day for 10 days | |||
* [[Tinidazole]] 2g once a day for 6 days is an alternative to [[metronidazole]] | |||
* [[Diloxanide furoate]] 500mg three times a day for 10 days must always be given afterwards. | |||
|} | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Infectious Disease Project]] | |||
[[Category:Metamonads]] | [[Category:Metamonads]] | ||
[[Category:Parasites]] | [[Category:Parasites]] | ||
| Line 127: | Line 516: | ||
[[Category:Conditions diagnosed by stool test]] | [[Category:Conditions diagnosed by stool test]] | ||
[[Category:Veterinary protozoology]] | [[Category:Veterinary protozoology]] | ||
Latest revision as of 21:01, 11 September 2017
|
Giardiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Giardia lamblia On the Web |
|
American Roentgen Ray Society Images of Giardia lamblia |
| Giardia lamblia | ||||||||
|---|---|---|---|---|---|---|---|---|
 Giardia cell, SEM
| ||||||||
| Scientific classification | ||||||||
| ||||||||
| Binomial name | ||||||||
| Giardia lamblia (Kunstler, 1882) |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Giardia lamblia (synonymous with Lamblia intestinalis and Giardia duodenalis) is a flagellated protozoan parasite that is responsible for the development of giardiasis.
Higher Order Classification
Eukaryota, Diplomonadida group, Diplomonadida, Hexamitidae, Giardiinae, Giardia, G. lamblia
Natural Reservoir
- Giardia affects humans and animals, such as cats, dogs, cows, beavers, deer, and sheep.
Microbiological Characteristicsc
- Giardia lamblia is a flagellated, microaerophilic parasite.
- The trophozoite form of G. lamblia is pear-shaped and has a unique morphology that includes two identical nuclei, a ventral disc for adhesion to the host intestine, and flagella.
Genome
- G. lamblia genome consists of 1.2 million base pairs (average GC content: 46%).[1]
- The genome pairs are distributed across five linear chromosomes.[1]
- Similar to other eukaryotes, each chromosome is flanked by the telomere sequence (5’TAGGG3’).[1]
Life cycle
Giardia belongs among the diplomonads.
Non-infective Cyst
- The life cycle begins with a noninfective cyst being excreted with faeces of an infected individual. Once out in the environment, the cyst becomes infective.
- A distinguishing characteristic of the cyst is 4 nuclei and a retracted cytoplasm.
Trophozoite
- Once ingested by a host, the trophozoite emerges to an active state of feeding and motility.
- After the feeding stage, the trophozoite undergoes asexual replication through longitudinal binary fission.
- The resulting trophozoites and cysts then pass through the digestive system in the feces.
- While the trophozoites may be found in the feces, only the cysts are capable of surviving outside of the host.
- Distinguishing features of the trophozoites are large karyosomes and lack of peripheral chromatin, giving the two nuclei a halo appearance.
-
SEM depicts the dorsal surface of a Giardia protozoan, isolated from a rat’s intestine. From Public Health Image Library (PHIL). [2]
-
SEM depicts the mucosal surface of the small intestine of a gerbil infested with Giardia sp. protozoa. From Public Health Image Library (PHIL). [2]
-
SEM depicts a Giardia lamblia protozoan in a late stage of cell division that was about to become two separate organisms, producing a heart-shaped form. From Public Health Image Library (PHIL). [2]
-
SEM depicts the ventral surface of a Giardia muris trophozoite. From Public Health Image Library (PHIL). [2]
-
SEM depicts dorsal surface of a Giardia protozoan, isolated from a rat’s intestine. From Public Health Image Library (PHIL). [2]
-
SEM depicts some of the ultrastructural morphologic details of an oblong-shaped Giardia sp. protozoan cyst. From Public Health Image Library (PHIL). [2]
-
SEM depicts the ventral surface of a Giardia muris trophozoite that had settled atop the mucosal surface of a rat’s intestine. From Public Health Image Library (PHIL). [2]
-
SEM depicts a Giardia lamblia protozoan that was about to become two separate organisms, as it was caught in a late stage of cell division. From Public Health Image Library (PHIL). [2]
-
SEM depicts a Giardia muris protozoan adhering itself to the microvillous border of an intestinal epithelial cell. From Public Health Image Library (PHIL). [2]
-
This photomicrograph depicts Giardia lamblia parasites using indirect immunofluorescence test for giardiasis. From Public Health Image Library (PHIL). [2]
Differential diagnosis
Giardia lamblia infection must be differentiated from other causes of viral, bacterial, and parasitic gastroentritis.
| Organism | Age predilection | Travel History | Incubation Size (cell) | Incubation Time | History and Symptoms | Diarrhea type8 | Food source | Specific consideration | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fever | N/V | Cramping Abd Pain | Small Bowel | Large Bowel | Inflammatory | Non-inflammatory | |||||||||
| Viral | Rotavirus | <2 y | - | <102 | <48 h | + | + | - | + | + | - | Mostly in day cares, most common in winter. | |||
| Norovirus | Any age | - | 10 -103 | 24-48 h | + | + | + | + | + | - | Most common cause of gastroenteritis, abdominal tenderness, | ||||
| Adenovirus | <2 y | - | 105 -106 | 8-10 d | + | + | + | + | + | - | No seasonality | ||||
| Astrovirus | <5 y | - | 72-96 h | + | + | + | + | + | Seafood | Mostly during winter | |||||
| Bacterial | Escherichia coli | ETEC | Any age | + | 108 -1010 | 24 h | - | + | + | + | + | - | Causes travelers diarrhea, contains heat-labile toxins (LT) and heat-stable toxins (ST) | ||
| EPEC | <1 y | - | 10† | 6-12 h | - | + | + | + | + | Raw beef and chicken | - | ||||
| EIEC | Any ages | - | 10† | 24 h | + | + | + | + | + | Hamburger meat and unpasteurized milk | Similar to shigellosis, can cause bloody diarrhea | ||||
| EHEC | Any ages | - | 10 | 3-4 d | - | + | + | + | + | Undercooked or raw hamburger (ground beef) | Known as E. coli O157:H7, can cause HUS/TTP. | ||||
| EAEC | Any ages | + | 1010 | 8-18 h | - | - | + | + | + | - | May cause prolonged or persistent diarrhea in children | ||||
| Salmonella sp. | Any ages | + | 1 | 6 to 72 h | + | + | + | + | + | Meats, poultry, eggs, milk and dairy products, fish, shrimp, spices, yeast, coconut, sauces, freshly prepared salad. | Can cause salmonellosis or typhoid fever. | ||||
| Shigella sp. | Any ages | - | 10 - 200 | 8-48 h | + | + | + | + | + | Raw foods, for example, lettuce, salads (potato, tuna, shrimp, macaroni, and chicken) | Some strains produce enterotoxin and Shiga toxin similar to those produced by E. coli O157:H7 | ||||
| Campylobacter sp. | <5 y, 15-29 y | - | 104 | 2-5 d | + | + | + | + | + | Undercooked poultry products, unpasteurized milk and cheeses made from unpasteurized milk, vegetables, seafood and contaminated water. | May cause bacteremia, Guillain-Barré syndrome (GBS), hemolytic uremic syndrome (HUS) and recurrent colitis | ||||
| Yersinia enterocolitica | <10 y | - | 104 -106 | 1-11 d | + | + | + | + | + | Meats (pork, beef, lamb, etc.), oysters, fish, crabs, and raw milk. | May cause reactive arthritis; glomerulonephritis; endocarditis; erythema nodosum.
can mimic appendicitis and mesenteric lymphadenitis. | ||||
| Clostridium perfringens | Any ages | > 106 | 16 h | - | - | + | + | + | Meats (especially beef and poultry), meat-containing products (e.g., gravies and stews), and Mexican foods. | Can survive high heat, | |||||
| Vibrio cholerae | Any ages | - | 106-1010 | 24-48 h | - | + | + | + | + | Seafoods, including molluscan shellfish (oysters, mussels, and clams), crab, lobster, shrimp, squid, and finfish. | Hypotension, tachycardia, decreased skin turgor. Rice-water stools | ||||
| Parasites | Protozoa | Giardia lamblia | 2-5 y | + | 1 cyst | 1-2 we | - | - | + | + | + | Contaminated water | May cause malabsorption syndrome and severe weight loss | ||
| Entamoeba histolytica | 4-11 y | + | <10 cysts | 2-4 we | - | + | + | + | + | Contaminated water and raw foods | May cause intestinal amebiasis and amebic liver abscess | ||||
| Cryptosporidium parvum | Any ages | - | 10-100 oocysts | 7-10 d | + | + | + | + | + | Juices and milk | May cause copious diarrhea and dehydration in patients with AIDS especially with 180 > CD4 | ||||
| Cyclospora cayetanensis | Any ages | + | 10-100 oocysts | 7-10 d | - | + | + | + | + | Fresh produce, such as raspberries, basil, and several varieties of lettuce. | More common in rainy areas | ||||
| Helminths | Trichinella spp | Any ages | - | Two viable larvae (male and female) | 1-4 we | - | + | + | + | + | Undercooked meats | More common in hunters or people who eat traditionally uncooked meats | |||
| Taenia spp | Any ages | - | 1 larva or egg | 2-4 m | - | + | + | + | + | Undercooked beef and pork | Neurocysticercosis: Cysts located in the brain may be asymptomatic or seizures, increased intracranial pressure, headache. | ||||
| Diphyllobothrium latum | Any ages | - | 1 larva | 15 d | - | - | - | + | + | Raw or undercooked fish. | May cause vitamin B12 deficiency | ||||
8Small bowel diarrhea: watery, voluminous with less than 5 WBC/high power field
Large bowel diarrhea: Mucousy and/or bloody with less volume and more than 10 WBC/high power field
† It could be as high as 1000 based on patient's immunity system.
The table below summarizes the findings that differentiate inflammatory causes of chronic diarrhea[3][4][5][6][6]
| Cause | History | Laboratory findings | Diagnosis | Treatment |
|---|---|---|---|---|
| Diverticulitis |
|
|
Abdominal CT scan with oral and intravenous (IV) contrast | bowel rest, IV fluid resuscitation, and broad-spectrum antimicrobial therapy which covers anaerobic bacteria and gram-negative rods |
| Ulcerative colitis |
|
|
Endoscopy | Induction of remission with mesalamine and corticosteroids followed by the administration of sulfasalazine and 6-Mercaptopurine depending on the severity of the disease. |
| Entamoeba histolytica |
|
cysts shed with the stool | detects ameba DNA in feces | Amebic dysentery
Luminal amebicides for E. histolytica in the colon:
For amebic liver abscess:
|
References
- ↑ 1.0 1.1 1.2 Le Blancq SM, Kase RS, Van der Ploeg LH (1991). "Analysis of a Giardia lamblia rRNA encoding telomere with [TAGGG]n as the telomere repeat". Nucleic Acids Res. 19 (20): 5790. PMC 328996. PMID 1840670.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 "Public Health Image Library (PHIL)".
- ↑ Konvolinka CW (1994). "Acute diverticulitis under age forty". Am J Surg. 167 (6): 562–5. PMID 8209928.
- ↑ Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR; et al. (2005). "Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology". Can J Gastroenterol. 19 Suppl A: 5A–36A. PMID 16151544.
- ↑ Satsangi J, Silverberg MS, Vermeire S, Colombel JF (2006). "The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications". Gut. 55 (6): 749–53. doi:10.1136/gut.2005.082909. PMC 1856208. PMID 16698746.
- ↑ 6.0 6.1 Haque R, Huston CD, Hughes M, Houpt E, Petri WA (2003). "Amebiasis". N Engl J Med. 348 (16): 1565–73. doi:10.1056/NEJMra022710. PMID 12700377.
![SEM depicts the dorsal surface of a Giardia protozoan, isolated from a rat’s intestine. From Public Health Image Library (PHIL). [2]](/images/b/b7/Giardiasis09.jpeg)
![SEM depicts the mucosal surface of the small intestine of a gerbil infested with Giardia sp. protozoa. From Public Health Image Library (PHIL). [2]](/images/3/36/Giardiasis08.jpeg)
![SEM depicts a Giardia lamblia protozoan in a late stage of cell division that was about to become two separate organisms, producing a heart-shaped form. From Public Health Image Library (PHIL). [2]](/images/2/24/Giardiasis07.jpeg)
![SEM depicts the ventral surface of a Giardia muris trophozoite. From Public Health Image Library (PHIL). [2]](/images/0/05/Giardiasis06.jpeg)
![SEM depicts dorsal surface of a Giardia protozoan, isolated from a rat’s intestine. From Public Health Image Library (PHIL). [2]](/images/e/e5/Giardiasis05.jpeg)
![SEM depicts some of the ultrastructural morphologic details of an oblong-shaped Giardia sp. protozoan cyst. From Public Health Image Library (PHIL). [2]](/images/1/1c/Giardiasis04.jpeg)
![SEM depicts the ventral surface of a Giardia muris trophozoite that had settled atop the mucosal surface of a rat’s intestine. From Public Health Image Library (PHIL). [2]](/images/9/9e/Giardiasis03.jpeg)
![SEM depicts a Giardia lamblia protozoan that was about to become two separate organisms, as it was caught in a late stage of cell division. From Public Health Image Library (PHIL). [2]](/images/2/2e/Giardiasis02.jpeg)
![SEM depicts a Giardia muris protozoan adhering itself to the microvillous border of an intestinal epithelial cell. From Public Health Image Library (PHIL). [2]](/images/f/f4/Giardiasis01.jpeg)
![This photomicrograph depicts Giardia lamblia parasites using indirect immunofluorescence test for giardiasis. From Public Health Image Library (PHIL). [2]](/images/5/55/Giardiasis10.jpeg)