Down syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 369: | Line 369: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Revision as of 13:42, 13 August 2009
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Down syndrome |
|
Articles |
|---|
|
Most recent articles on Down syndrome Most cited articles on Down syndrome |
|
Media |
|
Powerpoint slides on Down syndrome |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Down syndrome at Clinical Trials.gov Trial results on Down syndrome Clinical Trials on Down syndrome at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Down syndrome NICE Guidance on Down syndrome
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Down syndrome Discussion groups on Down syndrome Patient Handouts on Down syndrome Directions to Hospitals Treating Down syndrome Risk calculators and risk factors for Down syndrome
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Down syndrome |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Down syndrome or trisomy 21 (usually Down's Syndrome in British English[1]) is a genetic disorder caused by the presence of all or part of an extra 21st chromosome. It is named after John Langdon Down, the British doctor who described it in 1866. The disorder was identified as a chromosome 21 trisomy by Jérôme Lejeune in 1959. The condition is characterized by a combination of major and minor differences in structure. Often Down syndrome is associated with some impairment of cognitive ability and physical growth as well as facial appearance. Down syndrome can be identified during pregnancy or at birth.
Individuals with Down syndrome can have a lower than average cognitive ability, often ranging from mild to moderate learning disabilities. Developmental disabilities often manifest as a tendency toward concrete thinking or naïveté. A small number have severe to profound mental disability. The incidence of Down syndrome is estimated at 1 per 800 to 1,000 births.
Many of the common physical features of Down syndrome also appear in people with a standard set of chromosomes. They may include a single transverse palmar crease (a single instead of a double crease across one or both palms), an almond shape to the eyes caused by an epicanthic fold of the eyelid, upslanting Palpebral fissures, shorter limbs, poor muscle tone, a larger than normal space between the big and second toes, and protruding tongue. Health concerns for individuals with Down syndrome include a higher risk for congenital heart defects, gastroesophageal reflux disease, recurrent ear infections, obstructive sleep apnea, and thyroid dysfunctions.
Early childhood intervention, screening for common problems, medical treatment where indicated, a conducive family environment, and vocational training can improve the overall development of children with Down syndrome. Although some of the physical genetic limitations of Down syndrome cannot be overcome, education and proper care will improve quality of life.[2]
Characteristics

Individuals with Down syndrome may have some or all of the following physical characteristics: oblique eye fissures with epicanthic skin folds on the inner corner of the eyes, muscle hypotonia (poor muscle tone), a flat nasal bridge, a single palmar fold, a protruding tongue (due to small oral cavity, and an enlarged tongue near the tonsils), a short neck, white spots on the iris known as Brushfield spots,[3] excessive flexibility in joints, congenital heart defects, excessive space between large toe and second toe, a single flexion furrow of the fifth finger, and a higher number of ulnar loop dermatoglyphs. Most individuals with Down syndrome have mental retardation in the mild (IQ 50–70) to moderate (IQ 35–50) range,[4] with scores of children having Mosaic Down syndrome (explained below) typically 10–30 points higher.[5] In addition, individuals with Down syndrome can have serious abnormalities affecting any body system.
Genetics
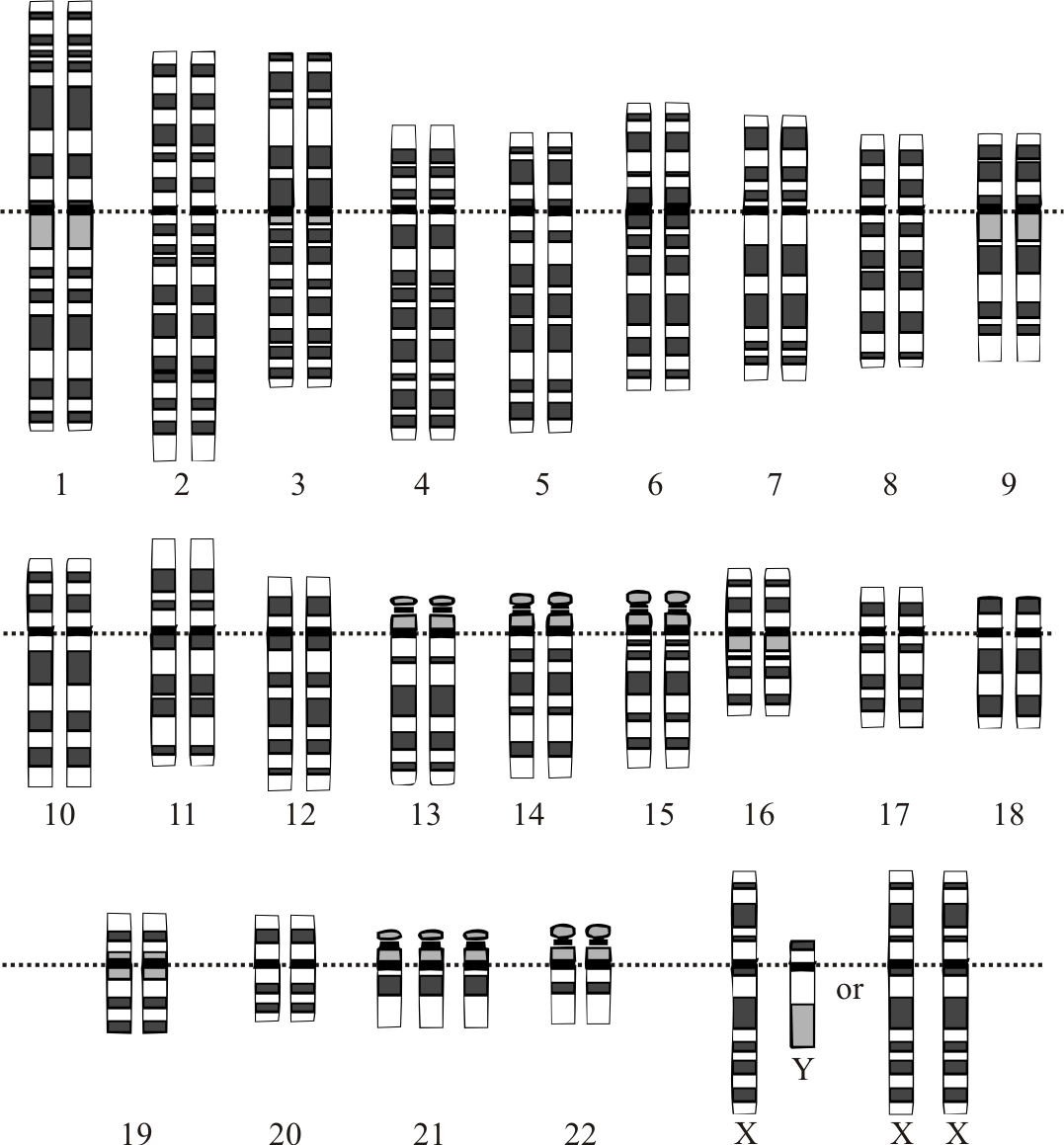
Down syndrome is a chromosomal abnormality characterized by the presence of an extra copy of genetic material on the 21st chromosome, either in whole (trisomy 21) or part (such as due to translocations). The effects of the extra copy vary greatly among individuals, depending on the extent of the extra copy, genetic background, environmental factors, and random chance. Down syndrome occurs in all human populations, and analogous effects have been found in other species such as chimpanzees[6] and mice. Recently, researchers have created transgenic mice with most of human chromosome 21 (in addition to the normal mouse chromosomes).[7] The extra chromosomal material can come about in several distinct ways. A typical human karyotype is designated as 46,XX or 46,XY, indicating 46 chromosomes with an XX arrangement typical of females and 46 chromosomes with an XY arrangement typical of males.[8]
Trisomy 21
Trisomy 21 (47,XX,+21) is caused by a meiotic nondisjunction event. With nondisjunction, a gamete (i.e., a sperm or egg cell) is produced with an extra copy of chromosome 21; the gamete thus has 24 chromosomes. When combined with a normal gamete from the other parent, the embryo now has 47 chromosomes, with three copies of chromosome 21. Trisomy 21 is the cause of approximately 95% of observed Down syndromes, with 88% coming from nondisjunction in the maternal gamete and 8% coming from nondisjunction in the paternal gamete.[9]
Mosaicism
Trisomy 21 is caused prior to conception, and all cells in the body are affected. However, when some of the cells in the body are normal and other cells have trisomy 21, it is called Mosaic Down syndrome (46,XX/47,XX,+21).[10] This can occur in one of two ways: A nondisjunction event during an early cell division in a normal embryo leads to a fraction of the cells with trisomy 21; or a Down syndrome embryo undergoes nondisjunction and some of the cells in the embryo revert to the normal chromosomal arrangement. There is considerable variability in the fraction of trisomy 21, both as a whole and among tissues. This is the cause of 1–2% of the observed Down syndromes.[9]
Robertsonian translocation
The extra chromosome 21 material that causes Down syndrome may be due to a Robertsonian translocation. In this case, the long arm of chromosome 21 is attached to another chromosome, often chromosome 14 (45,XX, t(14;21q)) or itself (called an isochromosome, 45,XX, t(21q;21q)). Normal disjunctions leading to gametes have a significant chance of creating a gamete with an extra chromosome 21. Translocation Down syndrome is often referred to as familial Down syndrome. It is the cause of 2–3% of observed cases of Down syndrome.[9] It does not show the maternal age effect, and is just as likely to have come from fathers as mothers.
Duplication of a portion of chromosome 21
Rarely, a region of chromosome 21 will undergo a duplication event. This will lead to extra copies of some, but not all, of the genes on chromosome 21 (46,XX, dup(21q)).[11] If the duplicated region has genes that are responsible for Down syndrome physical and mental characteristics, such individuals will show those characteristics. This cause is very rare and no rate estimates are available.
Incidence
The incidence of Down syndrome is estimated at 1 per 800 to 1 per 1000 births.[12] In 2006, the Center for Disease Control estimated the rate as 1 per 733 live births in the United States (5429 new cases per year).[13] Approximately 95% of these are trisomy 21. Down syndrome occurs in all ethnic groups and among all economic classes.
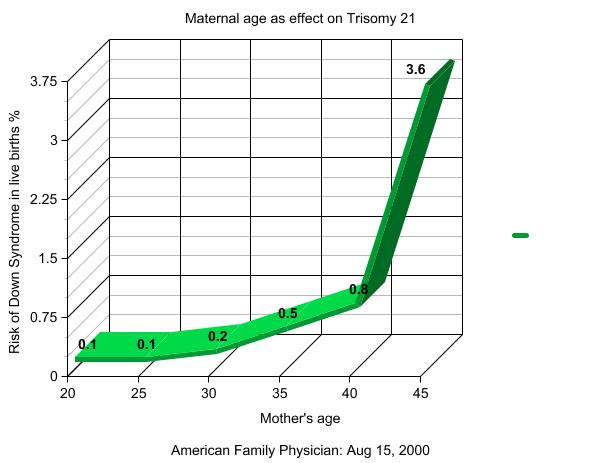
Maternal age influences the chances of conceiving a baby with Down syndrome. At maternal age 20 to 24, the probability is 1/1490; at age 40 the probability is 1/60, and at age 49 the probability is 1/11.[14] Although the probability increases with maternal age, 80% of children with Down syndrome are born to women under the age of 35,[15] reflecting the overall fertility of that age group. Recent data also suggest that paternal age also increases the risk of Down Syndrome manifesting in pregnancies in older mothers.[16]
Prenatal screening
Pregnant women can be screened for various complications during pregnancy. Many standard prenatal screens can discover Down syndrome. Genetic counseling along with genetic testing, such as amniocentesis, chorionic villus sampling (CVS), or percutaneous umbilical blood sampling (PUBS) are usually offered to families who may have an increased chance of having a child with Down syndrome, or where normal prenatal exams indicate possible problems. Genetic screens are often performed on pregnant women older than 30 or 35.
Amniocentesis and CVS are considered invasive procedures, in that they involve inserting instruments into the uterus, and therefore carry a small risk of causing fetal injury or miscarriage. There are several common non-invasive screens that can indicate a fetus with Down syndrome. These are normally performed in the late first trimester or early second trimester. Due to the nature of screens, each has a significant chance of a false positive, suggesting a fetus with Down syndrome when, in fact, the fetus does not have this genetic abnormality. Screen positives must be verified before a Down syndrome diagnosis is made. Common screening procedures for Down syndrome are given in Table 1.
| Screen | When performed (weeks gestation) | Detection rate | False positive rate | Description |
|---|---|---|---|---|
| Triple screen | 15–20 | 75% | 8.5% | This test measures the maternal serum alpha feto protein (a fetal liver protein), estriol (a pregnancy hormone), and human chorionic gonadotropin (hCG, a pregnancy hormone).[17] |
| Quad screen | 15–20 | 79% | 7.5% | This test measures the maternal serum alpha feto protein (a fetal liver protein), estriol (a pregnancy hormone), human chorionic gonadotropin (hCG, a pregnancy hormone), and high inhibin-Alpha (INHA).[17] |
| AFP/free beta screen | 13–22 | 80% | 2.8% | This test measures the alpha feto protein, produced by the fetus, and free beta hCG, produced by the placenta. |
| Nuchal translucency/free beta/PAPPA screen | 10–13.5 | 91%[18] | 5%[18] | Uses ultrasound to measure Nuchal Translucency in addition to the freeBeta hCG and PAPPA (pregnancy-associated plasma protein A). NIH has confirmed that this first trimester test is more accurate than second trimester screening methods.[19] |

Even with the best non-invasive screens, the detection rate is 90%–95% and the rate of false positive is 2%–5%. False positives can be caused by undetected multiple fetuses (very rare with the ultrasound tests), incorrect date of pregnancy, or normal variation in the proteins.
Confirmation of screen positive is normally accomplished with amniocentesis. This is an invasive procedure and involves taking amniotic fluid from the mother and identifying fetal cells. The lab work can take several weeks but will detect over 99.8% of all numerical chromosomal problems with a very low false positive rate. [20]
Due to the low incidence of Down syndrome, a vast majority of early screen positives are false.[21] Since false positives typically prompt an amniocentesis to confirm the result, and the amniocentesis carries a small risk of inducing miscarriage, there is a slight risk of miscarrying a healthy fetus. (The added miscarriage risk from an amniocentesis is traditionally quoted as 0.5%, but recent studies suggest that it may be considerably smaller (0.06% with a 95% CI of 0 to 0.5%).[22])
A 2002 literature review of elective abortion rates found that 91–93% of pregnancies with a diagnosis of Down syndrome were terminated.[23] Physicians and ethicists are concerned about the ethical ramifications,[24] with some commentators calling it "eugenics by abortion".[25] Many members of the disability rights movement "believe that public support for prenatal diagnosis and abortion based on disability contravenes the movement's basic philosophy and goals."[26]
Cognitive development
Cognitive development in children with Down syndrome is quite variable. It is not currently possible at birth to predict the capabilities of any individual reliably, nor are the number or appearance of physical features predictive of future ability. The identification of the best methods of teaching each particular child ideally begins soon after birth through early intervention programs.[27] Since children with Down syndrome have a wide range of abilities, success at school can vary greatly, which stresses the importance of evaluating children individually. The cognitive problems that are found among children with Down syndrome can also be found among typical children. Therefore, parents can use general programs that are offered through the schools or other means. Language skills show a difference between understanding speech and expressing speech. It is not uncommon for children with Down Syndrome to have a speech delay, although it is common for them to need speech therapy to help with expressive language.[28] Fine motor skills are delayed[29] and often lag behind gross motor skills and can interfere with cognitive development. Gross Motor Skills can be affected anywhere from minor to major. Some children will walk at around 2 while others around 4. A physical therapist or APE will help a child with this. [30]
Speech therapy is usually performed because of the enlarged tongue which many children with Down Syndrome have, which makes clear speech difficult. Speech therapy and immersion in social situations where conversation is common and extended can result in excellent language development. Unfortunately, relatively little is done in early intervention programs to foster cognitive development. A good Montessori school may be an excellent environment for fostering learning in individuals with Down Syndrome. [31] [32] Significant work on cognitive development has been done by Dr. Raymundo Veras of Brazil. Dr. Veras worked from the model of early childhood education established by Glenn Doman of the Institutes for the Achievement of Human Potential, in Philadelphia. As a result of his work, he wrote a book entitled Children of Dreams, Children of Hope, in which he recounts demonstrating to Mr. Doman a preschool age girl who was able to read in four languages and play the violin. [33] [34] Children with Down Syndrome often have an enhanced ability to memorize songs, stories, vocabulary, and other language material, which can be capitalized upon. [35]
In education, mainstreaming of children with Down syndrome is becoming less controversial in many countries. For example, there is a presumption of mainstream in many parts of the UK. Mainstreaming is the process whereby students of differing abilities are placed in classes with their chronological peers. Children with Down syndrome may not age emotionally/socially and intellectually at the same rates as children without Down syndrome, so over time the intellectual and emotional gap between children with and without Down syndrome may widen. Complex thinking as required in sciences but also in history, the arts, and other subjects can often be beyond the abilities of some, or achieved much later than in other children. Therefore, children with Down syndrome may benefit from mainstreaming provided that some adjustments are made to the curriculum.[36]
Some European countries such as Germany and Denmark advise a two-teacher system, whereby the second teacher takes over a group of children with disabilities within the class. A popular alternative is cooperation between special schools and mainstream schools. In cooperation, the core subjects are taught in separate classes, which neither slows down the typical students nor neglects the students with disabilities. Social activities, outings, and many sports and arts activities are performed together, as are all breaks and meals.[37]
Health
The medical consequences of the extra genetic material in Down syndrome are highly variable and may affect the function of any organ system or bodily process. The health aspects of Down syndrome encompass anticipating and preventing effects of the condition, recognizing complications of the disorder, managing individual symptoms, and assisting the individual and his/her family in coping and thriving with any related disability or illnesses.[38]
The most common manifestations of Down syndrome are the characteristic facial features, cognitive impairment, congenital heart disease (typically a ventricular septal defect), hearing deficits (maybe due to sensory-neural factors, or chronic serous otitis media, also known as Glue-ear), short stature, thyroid disorders, and Alzheimer's disease. Other less common serious illnesses include leukemia, immune deficiencies, and epilepsy. However, health benefits of Down syndrome include greatly reduced incidence of many common malignancies except leukemia and testicular cancer[39] — although it is, as yet, unclear whether the reduced incidence of various fatal cancers among people with Down syndrome is as a direct result of tumor-suppressor genes on chromosome 21, because of reduced exposure to environmental factors that contribute to cancer risk, or some other as-yet unspecified factor. Down syndrome can result from several different genetic mechanisms. This results in a wide variability in individual symptoms due to complex gene and environment interactions. Prior to birth, it is not possible to predict the symptoms that an individual with Down syndrome will develop. Some problems are present at birth, such as certain heart malformations. Others become apparent over time, such as epilepsy.
These factors can contribute to a significantly shorter lifespan for people with Down syndrome. One study, carried out in the United States in 2002, showed an average lifespan of 49 years, with considerable variations between different ethnic and socio-economic groups.[40]
Fertility amongst both males and females is reduced,[41] with only three recorded instances of males with Down syndrome fathering children.[42][43]
Genetic research
Down syndrome is “a developmental abnormality characterized by trisomy of human chromosome 21 (Nelson 619). The extra copy of chromosome-21 leads to an over expression of certain genes located on chromosome-21.
Research by Arron et al shows that some of the phenotypes (displayed genetic characteristics), associated with Down Syndrome can be related to the dysregulation of gene-regulating proteins (596). The gene-regulating proteins bind to DNA and initiate certain segments of DNA to be replicated for the production of a certain protein (Arron et al. 596). The gene-regulator in interest is called NFATc. Its activities are controlled by two proteins, DSCR1 and DYRK1A; these genes are located on chromosome-21 (Epstein 582). In people with Down Syndrome, these proteins have 1.5 times greater concentration than normal (Arron et al. 597). The elevated levels of DSCR1 and DYRK1A mean that most of the NFATc is located in the cytoplasm rather than in the nucleus promoting DNA replication which will produce vital proteins (Epstein 583).
This dysregulation was discovered by testing in transgenic mice. The mice had segments of their chromosomes duplicated to simulate a human chromosme-21 trisomy (Arron et al. 597). A common characteristic of Down Syndrome is poor muscle tone, so a test involving the grip strength of the mice showed that the genetically modified mice had a significantly weaker grip (Arron et al. 596). The mice squeezed a probe with a paw; the modified mice displayed a .2 Newton (measurement of force) weaker grip (Arron et al. 596). Down syndrome is also characterized by increased socialization. Both modified and unmodified mice were observed for social interaction. The modified mice showed as many as 25% more interactions per time period as the unmodified mice (Arron et al. 596).
The genes that may be responsible for the phenotypes associated may be located proximal to 21q22.3. Testing by Olson et al, in transgenic mice show the duplicated genes presumed to cause the phenotypes are not enough to cause the exact features. While the mice had sections of multiple genes duplicated to approximate a human chromosome-21 triplication, they only showed slight craniofacial abnormalities (688-690). The transgenic mice were compared to mice that had no gene duplication by measuring distances on various points on their skeletal structure and comparing them to the normal mice (Olson et al. 687). The exact characteristics of Down Syndrome were not observed, so more genes involved for Down Syndrome phenotypes have to be located elsewhere.
Reeves et al, using 250 clones of chromosme-21 and specific gene markers, were able to map the gene in mutated bacteria. The testing had 99.7% coverage of the gene with 99.9995% accuracy due to multiple redundancies in the mapping techniques. In the study 225 genes were identified (311-313).
The search for major genes that may be involved in Down syndrome symptoms is normally in the region 21q21–21q22.3. However, studies by Reeves et al. show that 41% of the genes on chromosome-21 of have no functional purpose, and only 54% of functional genes have a known protein sequence. Functionality of genes was determined by a computer using exon prediction analysis (312). Exon sequence was obtained by the same procedures of the chromosome-21 mapping.
Research has led to an understanding that two genes located on chromosome-21, that code for proteins that control gene regulators, DSCR1 and DYRK1A can be responsible for some of the phenotypes associated with Down Syndrome. DSCR1 and DYRK1A cannot be blamed outright for the symptoms; there are a lot of genes that have no known purpose. And further research is needed in order to treat Down Sydrome more effectively.
Recent use of transgenic mice to study specific genes in the Down syndrome critical region has yielded some results. APP[44] is an Amyloid beta A4 precursor protein. It is suspected to have a major role in cognitive difficulties.[45] Another gene, ETS2[46] is Avian Erythroblastosis Virus E26 Oncogene Homolog 2. Researchers have "demonstrated that overexpression of ETS2 results in apoptosis. Transgenic mice overexpressing ETS2 developed a smaller thymus and lymphocyte abnormalities, similar to features observed in Down syndrome."[47]
Sociological and cultural aspects
Advocates for people with Down syndrome point to various factors, such as special education and parental support groups to make life easier for parents. There are also strides being made in education, housing, and social settings to create environments which are accessible and supportive to people with Down syndrome. In most developed countries, since the early twentieth century many people with Down syndrome were housed in institutions or colonies and excluded from society. However, since the early 1960s parents and their organizations (such as MENCAP), educators and other professionals have generally advocated a policy of inclusion,[48] bringing people with any form of mental or physical disability into general society as much as possible. In many countries, people with Down syndrome are educated in the normal school system; there are increasingly higher-quality opportunities to mix special education with regular education settings.
Despite this change, reduced abilities of people with Down syndrome can pose a challenge to parents and families. Although living with family is preferable to institutionalization, people with Down syndrome often encounter patronizing attitudes and discrimination in the wider community.
The first World Down Syndrome Day was held on 21 March 2006. The day and month were chosen to correspond with 21 and trisomy respectively. It was proclaimed by Down Syndrome International.[49] In the United States, the National Down Syndrome Society observes Down Syndrome Month every October as "a forum for dispelling stereotypes, providing accurate information, and raising awareness of the potential of individuals with Down syndrome."[50] In South Africa, Down Syndrome Awareness Day is held every October 20.[51]
History
English physician John Langdon Down first characterized Down syndrome as a distinct form of mental disability in 1862, and in a more widely published report in 1866 entitled "Observations on an ethnic classification of idiots".[52] Due to his perception that children with Down syndrome shared physical facial similarities (epicanthal folds) with those of Blumenbach's Mongolian race, Down used terms such as mongolism and Mongolian idiocy.[53] Down wrote that mongolism represented "retrogression," the appearance of Mongoloid traits in the children of allegedly more advanced Caucasian parents.
By the 20th century, "Mongolian idiocy" had become the most recognizable form of mental disability. Most individuals with Down syndrome were institutionalized, few of the associated medical problems were treated, and most died in infancy or early adult life. With the rise of the eugenics movement, 33 of the (then) 48 U.S. states and several countries began programs of involuntary sterilization of individuals with Down syndrome and comparable degrees of disability. The ultimate expression of this type of public policy was the German euthanasia program "Action T-4", begun in 1940. Court challenges and public revulsion led to discontinuation or repeal of such programs during the decades after World War II.
Until the middle of the 20th century, the cause of Down syndrome remained unknown. However, the presence in all races, the association with older maternal age, and the rarity of recurrence had been noticed. Standard medical texts assumed it was caused by a combination of inheritable factors which had not been identified. Other theories focused on injuries sustained during birth.[54]
With the discovery of karyotype techniques in the 1950s, it became possible to identify abnormalities of chromosomal number or shape. In 1959, Professor Jérôme Lejeune discovered that Down syndrome resulted from an extra chromosome.[55] The extra chromosome was subsequently labeled as the 21st, and the condition as trisomy 21.
In his last years, Professor Lejeune did research into the question of metabolic abnormalities in persons with Down Syndrome. After his death in 1994, his research has been continued by Dr. Paddy Jim Baggot. Some success at identifying abnormalities and finding treatments has been experienced. In later research, it has been shown that measures to treat biochemical deficiencies should begin at about the 22nd week of pregnancy. Some parents are currently giving supplements to their children with Down Syndrome, which has resulted in some improvement of their capabilities. [56]
In 1961, nineteen geneticists wrote to the editor of The Lancet suggesting that Mongolian idiocy had "misleading connotations," had become "an embarrassing term," and should be changed.[57] The Lancet supported Down's Syndrome. The World Health Organization (WHO) officially dropped references to mongolism in 1965 after a request by the Mongolian delegate.[58] However, almost 40 years later, the term ‘mongolism’ still appears in leading medical texts such as Review of Medical Physiology, 22nd Edition, 2005, by Professor William Ganong and General and Systematic Pathology, 4th Edition, 2004, edited by Professor Sir James Underwood.
In 1975, the United States National Institutes of Health convened a conference to standardize the nomenclature of malformations. They recommended eliminating the possessive form: "The possessive use of an eponym should be discontinued, since the author neither had nor owned the disorder."[59] Although both the possessive and non-possessive forms are used in the general population, Down syndrome is the accepted term among professionals in the USA, Canada and other countries; Down's syndrome is still used in the United Kingdom and other areas.[60]
References
- ↑ "Trisomy 21: The Story of Down Syndrome paper".
- ↑ Roizen NJ, Patterson D.Down's syndrome. Lancet. 2003 12 April;361(9365):1281–9. Review. PMID 12699967
- ↑ "Definition of Brushfield's Spots".
- ↑ "Keep Kids Healthy article on Down syndrome". Unknown parameter
|accessedate=ignored (help) - ↑ Strom, C. "FAQ from Mosaic Down Syndrome Society". Retrieved 2006-06-03.
- ↑ McClure HM, Belden KH, Pieper WA, Jacobson CB. Autosomal trisomy in a chimpanzee: resemblance to Down's syndrome. Science. 1969 5 September;165(897):1010–2. PMID 4240970
- ↑ "Down's syndrome recreated in mice". BBC News. 2005-09-22. Retrieved 2006-06-14.
- ↑ For a description of human karyotype see Mittleman, A. (editor) (1995). "An International System for Human Cytogenetic Nomeclature". Retrieved 2006-06-04.
- ↑ 9.0 9.1 9.2 "Down syndrome occurrence rates (NIH)". Retrieved 2006-06-02.
- ↑ Mosaic Down syndrome on the Web
- ↑ Petersen MB, Tranebjaerg L, McCormick MK, Michelsen N, Mikkelsen M, Antonarakis SE. Clinical, cytogenetic, and molecular genetic characterization of two unrelated patients with different duplications of 21q. Am J Med Genet Suppl. 1990;7:104-9. PMID 2149934
- ↑ Based on estimates by National Institute of Child Health & Human Development "Down syndrome rates". Retrieved 2006-06-21.
- ↑ Center for Disease Control (6 January 2006). "Improved National Prevalence Estimates for 18 Selected Major Birth Defects, United States, 1999–2001". Morbidity and Mortality Weekly Report. 54 (51 & 52): 1301–1305. Check date values in:
|date=(help) - ↑ Hook, E.B. (1981). "Rates of chromosomal abnormalities at different maternal ages". Obstet Gynecol. 58: 282. PMID 6455611
- ↑ Estimate from "National Down Syndrome Center". Retrieved 2006-04-21.
- ↑ Warner, Jennifer. "Dad's Age Raises Down Syndrome Risk, Too", "WebMD Medical News". Retrieved 2007-09-29.
- ↑ 17.0 17.1 For a current estimate of rates, see Benn, PA, J Ying, T Beazoglou, JFX Egan. "Estimates for the sensitivity and false-positive rates for second trimester serum screening for Down syndrome and trisomy 18 with adjustments for cross-identification and double-positive results". Prenatal Diagnosis. 21 (1): 46–51. PMID 11180240
- ↑ 18.0 18.1 Some practices report adding Nasal Bone measurements and increasing the detection rate to 95% with a 2% False Positive Rate.
- ↑ NIH FASTER study (NEJM 2005 (353):2001). See also J.L. Simplson's editorial (NEJM 2005 (353):19).
- ↑ Fackler, A. "Down syndrome". Retrieved 2006-09-07.
- ↑ Assume the false positive rate is 2% (at the low end), the incidence of Down syndrome is 1/500 (on the high side) with 95% detection, and there is no ascertainment bias. Out of 100,000 screens, 200 will have Down syndrome, and the screen will detect 190 of them. From the 99,800 normal pregnancies, 1996 will be given a positive result. So, among the 2,186 positive test results, 91% will be false positives and 9% will be true positives.
- ↑ Eddleman, Keith A.; et al. (2006). "Pregnancy loss rates after midtrimester amniocentesis". Obstet Gynecol. 108 (5): 1067–1072. Retrieved 2006-12-09. PMID 17077226
- ↑ Caroline Mansfield, Suellen Hopfer, Theresa M. Marteau (1999). "Termination rates after prenatal diagnosis of Down syndrome, spina bifida, anencephaly, and Turner and Klinefelter syndromes: a systematic literature review". Prenatal Diagnosis. 19 (9): 808–812. PMID 10521836 This is similar to 90% results found by David W. Britt, Samantha T. Risinger, Virginia Miller, Mary K. Mans, Eric L. Krivchenia, Mark I. Evans (1999). "Determinants of parental decisions after the prenatal diagnosis of Down syndrome: Bringing in context". American Journal of Medical Genetics. 93 (5): 410–416. PMID 10951466
- ↑ Glover, NM and Glover, SJ (1996). "Ethical and legal issues regarding selective abortion of fetuses with Down syndrome". Ment. Retard. 34 (4): 207–214. PMID 8828339.
- ↑ Will, George (2005-04-14). "Eugenics By Abortion: Is perfection an entitlement?". Washington Post: A37. Retrieved 2006-07-03.
- ↑ Erik Parens and Adrienne Asch (2003). "Disability rights critique of prenatal genetic testing: Reflections and recommendations". Mental Retardation and Developmental Disabilities Research Reviews. 9 (1): 40–47. Retrieved 2006-07-03. PMID 12587137
- ↑ "Dear New or Expectant Parents". National Down Syndrome Society. Retrieved 2006-05-12. Also "Research projects - Early intervention and education". Retrieved 2006-06-02.
- ↑ Bird, G. and S. Thomas (2002). "Providing effective speech and language therapy for children with Down syndrome in mainstream settings: A case example". Down Syndrome News and Update. 2 (1): 30–31. Also, Kumin, Libby (1998). "Comprehensive speech and language treatment for infants, toddlers, and children with Down syndrome". In Hassold, T.J.and D. Patterson. Down Syndrome: A Promising Future, Together. New York: Wiley-Liss.
- ↑ "Development of Fine Motor Skills in Down Syndrome". Retrieved 2006-07-03.
- ↑ M. Bruni. "Occupational Therapy and the Child with Down Syndrome". Retrieved 2006-06-02.
- ↑ "Down Syndrome Information".
- ↑ "Berkeley Parents Network". Retrieved 2007-10-02.
- ↑ "Instituto Véras". Retrieved 2007-10-02.
- ↑ "The Institutes for the Achievement of Human Potential". Retrieved 2007-10-02.
- ↑ "Down Syndrome".
- ↑ S.E.Armstrong. "Inclusion: Educating Students with Down Syndrome with Their Non-Disabled Peers". Retrieved 2006-05-12. Also, see Debra L. Bosworth. "Benefits to Students with Down Syndrome in the Inclusion Classroom: K-3". Retrieved 2006-06-12. Finally, see a survey by NDSS on inclusion, Gloria Wolpert (1996). "The Educational Challenges Inclusion Study". National Down Syndrome Society. Retrieved 2006-06-28.
- ↑ There are many such programs. One is described by Action Alliance for Children, Template:Web cite Also, see Template:Web cite
- ↑ American Academy of Pediatrics Committee on Genetics (2001). "American Academy of Pediatrics: Health supervision for children with Down syndrome". Pediatrics. 107 (2): 442–449. PMID 11158488. Unknown parameter
|month=ignored (help) - ↑ Yang Q, Rasmussen SA, Friedman JM. Mortality associated with Down's syndrome in the USA from 1983 to 1997: a population-based study. Lancet 2002 23 March;359(9311):1019–25. PMID 11937181
- ↑ Young, Emma (2002-03-22). "Down syndrome lifespan doubles". New Scientist. Retrieved 2006-10-14.
- ↑ Ying-Hui H. Hsiang, Gary D. Berkovitz, Gail L. Bland, Claude J. Migeon, Andrew C. Warren, John M. Opitz, James F. Reynolds (1987). "Gonadal function in patients with Down syndrome". American Journal of Medical Genetics. Wiley-Liss, Inc. 27 (2): 449–458. 10.1002/ajmg.1320270223.
- ↑ Sheridan R, Llerena J, Matkins S, Debenham P, Cawood A, Bobrow M (1989). "Fertility in a male with trisomy 21". J Med Genet. 26 (5): 294–8. PMID 2567354.
- ↑ Pradhan M, Dalal A, Khan F, Agrawal S (2006). "Fertility in men with Down syndrome: a case report". Fertil Steril. 86 (6): 1765.e1–3. PMID 17094988.
- ↑ Online Mendelian Inheritance in Man (OMIM) 104760, gene located at 21q21. Retrieved on 2006-12-05.
- ↑ Shekhar, Chandra (2006-07-06). "Down syndrome traced to one gene". The Scientist. Retrieved 2006-07-11.
- ↑ Online Mendelian Inheritance in Man (OMIM) 164740, located at 21 q22.3. Retrieved on 2006-12-05.
- ↑ OMIM, NIH. "V-ETS Avian Erythroblastosis virus E26 Oncogene Homolog 2". Retrieved 2006-06-29.
- ↑ Inclusion. National Down Syndrome Society. Retrieved 2006-05-21.
- ↑ "World Down Syndrome Day". Retrieved 2006-06-02.
- ↑ National Down Syndrome Society
- ↑ Down Syndrome South Africa
- ↑ Down, J.L.H. (1866). "Observations on an ethnic classification of idiots". Clinical Lecture Reports, London Hospital. 3: 259–262. Retrieved 2006-07-14. For a history of the disorder, see OC Ward (1998). John Langdon Down, 1828–1896. Royal Society of Medicine Press. ISBN 1-85315-374-5. or Conor, Ward. "John Langdon Down and Down's syndrome (1828–1896)". Retrieved 2006-06-02.
- ↑ "John Langdon Down: The Man and the Message". Down Syndrome Research and Practice. 6 (1): 19–24. 1999. Unknown parameter
|Author=ignored (|author=suggested) (help);|access-date=requires|url=(help) - ↑ Warkany, J. (1971). Congenital Malformations. Chicago: Year Book Medical Publishers, Inc. pp. 313–314. ISBN 0-8151-9098-0.
- ↑ "Jérôme Lejeune Foundation". Retrieved 2006-06-02.
- ↑ "The Michael Fund".
- ↑ Gordon, Allen (1961). "Mongolism (Correspondence)". The Lancet. 1 (7180): 775. Unknown parameter
|coauthors=ignored (help) - ↑ Howard-Jones, Norman (1979). "On the diagnostic term "Down's disease"". Medical History. 23 (1): 102–104. PMID 153994.
- ↑ A planning meeting was held on 20 March 1974, resulting in a letter to The Lancet."Classification and nomenclature of malformation (Discussion)". The Lancet. 303 (7861): 798. 1974. The conference was held 10 February-11 February 1975, and reported to The Lancet shortly afterward."Classification and nomenclature of morphological defects (Discussion)". The Lancet. 305 (7905): 513. 1975.
- ↑ Leshin, Len (2003). "What's in a name". Retrieved 2006-05-12.
Sources
- Arron, Joseph R., et al. (2006). NFAT dysregulation by increased dosage of DSCR1 and DYRK1A on chromosome 21. Nature, 441: 595-599.
- Epstein, Charles J. (2006). Critical Genes in Critical Region. Nature, 441: 582-583.
- Ganong, W.J. (2005). Review of Medical Physiology. New York: Mc-Graw Hill.
- Nelson, David L., & Gibbs, Richard H. (2004). The Critical Region in Trisomy-21. Science, 306: 619-621.
- Olson, L.E., Richtsmeier J.T., & Reeves R.H. (2004). A Chromosome-21 Critical Region Does Not Cause Specific Down Syndrome Phenotypes. Science, 306: 687-690.
- Reeves, Roger H., et al. (2000). The DNA Sequence of Human Chromosome 21. Nature, 405: 311-319.
- Underwood, J.C.E. (2004). General and Systematic Pathology. Edinburgh: Churchill Livingstone.
Bibliography
- Beck, M.N. (1999). Expecting Adam. New York: Berkley Books.
- Buckley, S. (2000). Living with Down Syndrome. Portsmouth, UK: The Down Syndrome Educational Trust. ISBN 1903806011.
- Down Syndrome Research Foundation (2005). Bright Beginnings: A Guide for New Parents. Buckinghamshire, UK: Down Syndrome Research Foundation.
- Dykens EM (2007). "Psychiatric and behavioral disorders in persons with Down syndrome". Ment Retard Dev Disabil Res Rev. 13 (3): 272–8. doi:10.1002/mrdd.20159. PMID 17910080.
- Hassold, T.J., D. Patterson, eds. (1999). Down Syndrome: A Promising Future, Together. New York: Wiley Liss.
- Kingsley, J. (1994). Count Us In: Growing up with Down Syndrome. San Diego: Harcourt Brace. Unknown parameter
|coauthors=ignored (help) - Pueschel, S.M., M. Sustrova, eds. (1997). Adolescents with Down Syndrome: Toward a More Fulfilling Life. Baltimore, MD: Paul H. Brookes.
- Selikowitz, M. (1997). Down Syndrome: The Facts (2nd edition ed.). Oxford, UK: Oxford University Press.
- Van Dyke, D.C. (1995). Medical and Surgical Care for Children with Down Syndrome. Bethesda, MD: Woodbine House. Unknown parameter
|coauthors=ignored (help) - Zuckoff, M. (2002). Choosing Naia: A Family's Journey. New York: Beacon Press.
External links
For comprehensive lists of Down syndrome links see
- Directory of Down Syndrome Internet Sites (US based, but contains international links)
- UK resources for Down's syndrome
Societies and associations
By country
- Canadian Down Syndrome Society (Canada)
- Down Syndrome Research Foundation (Canada)
- Down's Syndrome Federation of India (INDIA)
- Down's Syndrome Scotland (Scotland)
- Down's Syndrome Association UK (Not including Scotland)
- National Down Syndrome Society (USA)
- National Down Syndrome Congress (USA)
- International Mosaic Down Syndrome Association (USA)
- Down's Heart Group (heart conditions related to Down's Syndrome)
- Down Syndrome Association (Singapore)
Health & Targeted Nutritional Intervention
- Dr. Len Leshin in Texas, USA
- Down's Heart Group (heart conditions related to Down's Syndrome)
- Riverbend Down Syndrome Parent Support Group - loads of information
Template:Chromosomal abnormalities Template:SIB
ar:متلازمة داون cs:Downův syndrom da:Downs syndrom de:Down-Syndrom et:Downi sündroom fa:سندرم داون gl:Síndrome de Down ko:다운증후군 id:Sindrom Down it:Sindrome di Down he:תסמונת דאון ka:დაუნის სინდრომი ku:Sendroma Down lt:Dauno sindromas hu:Down-szindróma ms:Sindrom Down nl:Syndroom van Down new:डाउन सिन्ड्रम no:Downs syndrom simple:Down syndrome sk:Downov syndróm sl:Downov sindrom sr:Даунов синдром fi:Downin oireyhtymä sv:Downs syndrom uk:Синдром Дауна zh-yue:唐氏綜合症