Crohn's disease pathophysiology: Difference between revisions
Aditya Ganti (talk | contribs) |
Aditya Ganti (talk | contribs) |
||
| Line 42: | Line 42: | ||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
On microscopic | On microscopic analysis of the affected colon may show [[mucosa]]l inflammation. Histo-pathological finding include | ||
*Transmural [[inflammation]] | *Transmural [[inflammation]] | ||
* | *Lymphoid aggregates throughout the wall of the colon. | ||
*Focal infiltration of [[neutrophils]] along with [[lymphocyte|mononuclear cells]], may infiltrate into the [[Crypts of Lieberkühn|crypts]] leading to inflammation (crypititis) or abscess (crypt abscess). | |||
*Non- caseating [[Granuloma]]s (aggregates of [[macrophage]] derivatives) known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. | |||
*[[Granuloma]]s | *Blunting of the intestinal [[villus|villi]] | ||
* | *Atypical branching of the crypts | ||
*''Paneth cell metaplasia'' <ref name="Robbins">Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. ''Robbins Pathologic Basis of Disease: 5th Edition''. W.B. Saunders and Company, Philadelphia, 1994.</ref> | |||
* | |||
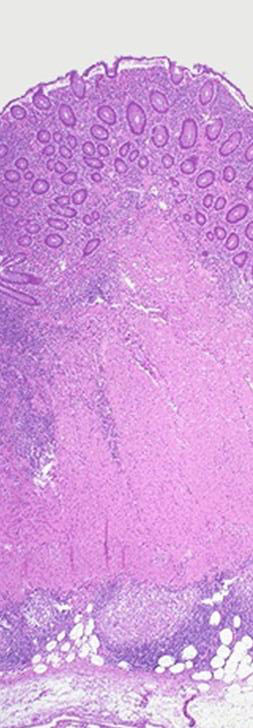
[[Image:Crohn's transmural path.jpg|thumb|center|120px|H and E section of [[colectomy]] showing transmural inflammation.]] | [[Image:Crohn's transmural path.jpg|thumb|center|120px|H and E section of [[colectomy]] showing transmural inflammation.]] | ||
Revision as of 19:39, 20 December 2017
| https://https://www.youtube.com/watch?v=thzOJV-CHRo%7C350}} |
|
Crohn's disease |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Crohn's disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Crohn's disease pathophysiology |
|
Risk calculators and risk factors for Crohn's disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Genetic and environmental factors play a key role in the pathogenesis of Crohn's disease. Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity. Environmental factors include autoimmune Disease and dysregulated Immune Response to Commensal Bacteria. Characteristic features of the pathology that point toward Crohn's disease are transmural pattern of inflammation and skip lesions. Under microscopy Granulomas are seen, which are aggregates of macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease.
Pathophysiology
Genetic and environmental factors play a key role in the pathogenesis of Crohn's disease.
Genetics
- Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity.[1][2]
- In earlier studies, only two genes were linked to Crohn's, but scientists now believe there are over eight genes that show genetics play a crucial role in the disease.
- Abnormalities in the immune system have often been invoked as being causes of Crohn's disease.
- It has been hypothesized that Crohn's disease involves augmentation of the Th1 of cytokine response in inflammation.[3]
- The most recent gene to be implicated in Crohn's disease is ATG16L1, which may reduce the effectiveness of autophagy, and hinder the body's ability to attack invasive bacteria.[4]
Environmental factors
Environmental factors include:
- Autoimmune disease
- Dysregulated immune response to commensal bacteria
Autoimmune disease
- Inflammatory response directed toward a self-antigen is believed to be responsible for development of Crohn's disease.
- Neutrophils are the main group of the cells that are targeted.
- Antineutrophil antibodies activate complement factors and localize on the luminal surface of the epithelium resulting in the destruction of intestinal tissue.
Immune reponse
- T-cell activation from chronic inflammation resulting in tissue injury is believed to the main reason in the pathogenesis of Crohn disease.
- After T cell activation by antigen presentation, unrestrained responses of type 1 T helper (Th1) cells predominate in Crohn disease as a consequence of defective regulation.
- Th1 cytokines such as interleukin (IL)-12 and TNF-α stimulate the inflammatory response.
- Inflammatory cells recruited by these cytokines release nonspecific inflammatory substances, including arachidonic acid metabolites, proteases, platelet activating factor, and free radicals, which result in direct injury to the intestine.
Gross Pathology
Characteristic features of the pathology that are suggestive of Crohn's disease include:
- Transmural pattern of inflammation, meaning that the inflammation may span the entire depth of the intestinal wall.
- Grossly, ulceration is an outcome seen in highly active disease.
- There is usually an abrupt transition between unaffected tissue and the ulcer.
Microscopic Pathology
On microscopic analysis of the affected colon may show mucosal inflammation. Histo-pathological finding include
- Transmural inflammation
- Lymphoid aggregates throughout the wall of the colon.
- Focal infiltration of neutrophils along with mononuclear cells, may infiltrate into the crypts leading to inflammation (crypititis) or abscess (crypt abscess).
- Non- caseating Granulomas (aggregates of macrophage derivatives) known as giant cells, are found in 50% of cases and are most specific for Crohn's disease.
- Blunting of the intestinal villi
- Atypical branching of the crypts
- Paneth cell metaplasia [5]
References
- ↑ Cuthbert A, Fisher S, Mirza M; et al. (2002). "The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease". Gastroenterology. 122 (4): 867–74. PMID 11910337.
- ↑ Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001 May 31;411(6837):603-6.
- ↑ Cobrin GM, Abreu MT. Defects in mucosal immunity leading to Crohn's disease. Immunol Rev. 2005 Aug;206:277-95. PMID 16048555
- ↑ Prescott NJ, Fisher SA, Franke A, Hampe J, Onnie CM, Soars D, Bagnall R, Mirza MM, Sanderson J, Forbes A, Mansfield JC, Lewis CM, Schreiber S, Mathew CG. A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn's disease and is independent of CARD15 and IBD5. Gastroenterology. 2007 May;132(5):1665-71. PMID: 17484864.
- ↑ Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. Robbins Pathologic Basis of Disease: 5th Edition. W.B. Saunders and Company, Philadelphia, 1994.