Constipation other diagnostic studies: Difference between revisions
Kiran Singh (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (8 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Constipation}} | {{Constipation}} | ||
{{CMG}} | {{CMG}}; {{AE}}{{EG}} | ||
==Overview== | |||
[[Endoscopic]] evaluation of patients with constipation include [[flexible sigmoidoscopy]] and [[colonoscopy]]. [[Flexible sigmoidoscopy]] is the direct visualization of the [[rectum]] and [[sigmoid colon]]. However, [[colonoscopy]] is study of the whole [[colon]] [[lumen]]. Every patient with alarm signs have to be evaluated using [[colonoscopy]]. In younger patients, [[flexible sigmoidoscopy]] would be sufficient for further investigation of alarm signs. Colonic [[manometry]] is 24-hour measurement of pressure within the [[large bowel]], using specific [[Probe|probes]] and portable recorders. [[Anorectal]] [[manometry]] is studying the pressure activity of anorectum during rest and [[defecation]], along with [[rectal]] [[sensation]], rectoanal reflexes, and [[anal sphincter]] function. Balloon expulsion test is a simple bedside test to evaluate the ability of patient to evacuate the artificial [[stool]]. Rectal biostat test consists of a very compliant plastic balloon, which is inserted into the [[rectum]], concurrently connected to computer device to measure the [[pressure]]. | |||
==Other Diagnostic Studies== | ==Other Diagnostic Studies== | ||
=== | === Endoscopy === | ||
{| align="right" | |||
|{{#ev:youtube|xWxdfhmXcNI|500}} | |||
|} | |||
* [[Endoscopic]] evaluation of patients with constipation include [[flexible sigmoidoscopy]] and [[colonoscopy]]. [[Flexible sigmoidoscopy]] is the direct visualization of the [[rectum]] and [[sigmoid colon]]. However, [[colonoscopy]] is study of the whole [[colon]] [[lumen]]. | |||
* Based on American Society of Gastrointestinal [[Endoscopy]] guideline, alarm signs in constipated patients are as following:<ref name="pmid16046978">{{cite journal |vauthors=Qureshi W, Adler DG, Davila RE, Egan J, Hirota WK, Jacobson BC, Leighton JA, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Baron TH, Faigel DO |title=ASGE guideline: guideline on the use of endoscopy in the management of constipation |journal=Gastrointest. Endosc. |volume=62 |issue=2 |pages=199–201 |year=2005 |pmid=16046978 |doi=10.1016/j.gie.2005.04.016 |url=}}</ref> | |||
** [[Rectal bleeding]] | |||
** [[Heme]] positive [[stool]] | |||
** [[Iron deficiency anemia]] | |||
** [[Weight loss]] | |||
** Obstructive symptoms | |||
** Recent onset of symptoms | |||
** [[Rectal prolapse]] | |||
** Change in [[stool]] caliber | |||
** Every subjects older than 50 years without previous screening for [[colon cancer]] | |||
* Every patient with alarm signs have to be evaluated using [[colonoscopy]]. In younger patients, [[flexible sigmoidoscopy]] would be sufficient for further investigation of alarm signs. | |||
* [[Colonoscopy]] has lower yield and correlation with [[symptoms]] in patients with constipation alone. Therefore, it is better not to use in patients with [[constipation]] and without any alarm sign. | |||
=== Colonic function tests === | |||
==== Colonic manometry ==== | |||
* Colonic [[manometry]] is 24-hour measurement of pressure within the [[large bowel]], using specific [[Probe|probes]] and portable recorders. | |||
* The colon pressure is studied during different conditions, such as:<ref name="pmid11254489">{{cite journal |vauthors=Rao SS, Sadeghi P, Beaty J, Kavlock R, Ackerson K |title=Ambulatory 24-h colonic manometry in healthy humans |journal=Am. J. Physiol. Gastrointest. Liver Physiol. |volume=280 |issue=4 |pages=G629–39 |year=2001 |pmid=11254489 |doi=10.1152/ajpgi.2001.280.4.G629 |url=}}</ref> | |||
{| align="right" | |||
|{{#ev:youtube|3Wgxhz9DwL8|500}} | |||
|} | |||
** Rest | |||
** During [[sleep]] | |||
** After waking | |||
** After meals | |||
** After provocative stimulation, such as: | |||
*** [[Drugs]] | |||
*** Meal | |||
*** Balloon distensions | |||
* Colonic [[manometry]] findings suggestive of constipation are:<ref name="pmid15571589">{{cite journal |vauthors=Rao SS, Sadeghi P, Beaty J, Kavlock R |title=Ambulatory 24-hour colonic manometry in slow-transit constipation |journal=Am. J. Gastroenterol. |volume=99 |issue=12 |pages=2405–16 |year=2004 |pmid=15571589 |doi=10.1111/j.1572-0241.2004.40453.x |url=}}</ref> | |||
** Fewer pressure waves and lower area under the curve | |||
** Decreased colonic motility induced by waking or meal | |||
** Lower incidence and propagation velocity of high-amplitude propagating contractions (HAPCs) | |||
=== | === Anorectal function tests === | ||
==== Anorectal manometry ==== | |||
* [[Anorectal]] [[manometry]] is studying the pressure activity of anorectum during rest and [[defecation]], along with the followings:<ref name="pmid15335368">{{cite journal |vauthors=Karlbom U, Lundin E, Graf W, Påhlman L |title=Anorectal physiology in relation to clinical subgroups of patients with severe constipation |journal=Colorectal Dis |volume=6 |issue=5 |pages=343–9 |year=2004 |pmid=15335368 |doi=10.1111/j.1463-1318.2004.00632.x |url=}}</ref> | |||
* | ** [[Rectal]] [[sensation]] | ||
* | {| align="right" | ||
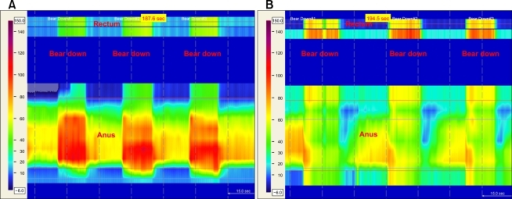
* | |[[image:PMC2879847 jnm-16-213-g001.png|thumb|700px|Anorectal manometry during simulated defecation in left lateral decubitus position with inappropriate increase of rectal pressure (green color) and no decrease in anal sphincter pressure (yellow to red color) which is consistent with pelvic floor dyssynergia(A); and sitting position with rectal pressure increased (yellow to red color) in coordination with relaxation of the anal sphincter pressure (green color), which is a normal pattern of anorectal manometry(B), via https://openi.nlm.nih.gov]] | ||
|} | |||
:* Rectoanal reflexes | |||
:* [[Anal sphincter]] function | |||
* Anorectal [[manometry]] is used for the diagnosis of defecatory disorder (dyssynergism) and [[Hirschsprung disease]]. | |||
* Lack of concordance between [[defecation]] propulsive pressure and reflex relaxation of the [[puborectalis]] and [[Sphincter ani externus muscle|external anal sphincter muscles]] is the primary concern in dyssynergism. Based on [[anorectal]] [[manometry]], there are four types of dyssynergic defecation.<ref name="pmid15500515">{{cite journal |vauthors=Rao SS, Mudipalli RS, Stessman M, Zimmerman B |title=Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus) |journal=Neurogastroenterol. Motil. |volume=16 |issue=5 |pages=589–96 |year=2004 |pmid=15500515 |doi=10.1111/j.1365-2982.2004.00526.x |url=}}</ref> | |||
{| | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Type | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Intrarectal pressure | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Intraanal pressure | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |1 | |||
| style="background:#F5F5F5;" align="center" + |↑ | |||
| style="background:#F5F5F5;" align="center" + |↑ | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |2 | |||
| style="background:#F5F5F5;" align="center" + | - | |||
| style="background:#F5F5F5;" align="center" + |↑ | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |3 | |||
| style="background:#F5F5F5;" align="center" + |↑ | |||
| style="background:#F5F5F5;" align="center" + | - | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |4 | |||
| style="background:#F5F5F5;" align="center" + | - | |||
| style="background:#F5F5F5;" align="center" + | - | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |Normal [[defecation]] | |||
| style="background:#F5F5F5;" align="center" + |↑ | |||
| style="background:#F5F5F5;" align="center" + |↓ | |||
|} | |||
=== | ==== Balloon expulsion test ==== | ||
* | * Balloon expulsion test is a simple bedside test to evaluate the ability of patient to evacuate the artificial [[stool]]. | ||
* The balloon filled with 50 cc of warm water or silicone-filled [[stool]]-like device is inserted into the [[rectum]] and the subject is asked to evacuate the balloon in sitting position. Expulsion within 1 minute is assumed as normal.<ref name="pmid10086665">{{cite journal |vauthors=Rao SS, Hatfield R, Soffer E, Rao S, Beaty J, Conklin JL |title=Manometric tests of anorectal function in healthy adults |journal=Am. J. Gastroenterol. |volume=94 |issue=3 |pages=773–83 |year=1999 |pmid=10086665 |doi=10.1111/j.1572-0241.1999.00950.x |url=}}</ref> | |||
* The expulsion test has a [[specificity]] and [[sensitivity]] of 89% and 88%, respectively. While, [[Negative predictive value|negative]] and [[Positive predictive value|positive predictive values]] are 97% and 67%, respectively.<ref name="pmid155005152">{{cite journal |vauthors=Rao SS, Mudipalli RS, Stessman M, Zimmerman B |title=Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus) |journal=Neurogastroenterol. Motil. |volume=16 |issue=5 |pages=589–96 |year=2004 |pmid=15500515 |doi=10.1111/j.1365-2982.2004.00526.x |url=}}</ref> | |||
{| align="right" | |||
|[[image:Barostat Balloon rectal.jpg|thumb|400px|Rectal barostat balloon-By No machine-readable author provided, via Wimimedia commons<ref name="//commons.wikimedia.org/wiki/User:Dbach"><"https://creativecommons.org/licenses/by-sa/2.5" title="Creative Commons Attribution-Share Alike 2.5">CC BY-SA 2.5, <"https://commons.wikimedia.org/w/index.php?curid=489883"></ref>]] | |||
|} | |||
==== Rectal barotest test ==== | |||
* Rectal biostat test consists of a very compliant plastic balloon, which is inserted into the [[rectum]], concurrently connected to computer device to measure the [[pressure]]. | |||
* First, the balloon is inflated in the [[rectum]] and then the effect of various [[defecation]] maneuvers on the pressure will be recorded. | |||
* Decreased intrarectal pressure during the [[defecation]] is suggestive of constipation secondary to dyssynergism.<ref name="pmid16696790">{{cite journal |vauthors=Gladman MA, Lunniss PJ, Scott SM, Swash M |title=Rectal hyposensitivity |journal=Am. J. Gastroenterol. |volume=101 |issue=5 |pages=1140–51 |year=2006 |pmid=16696790 |doi=10.1111/j.1572-0241.2006.00604.x |url=}}</ref> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category: | [[Category:Medicine]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Radiology]] | |||
Latest revision as of 21:07, 29 July 2020
|
Constipation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Constipation On the Web |
|
American Roentgen Ray Society Images of Constipation |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2]
Overview
Endoscopic evaluation of patients with constipation include flexible sigmoidoscopy and colonoscopy. Flexible sigmoidoscopy is the direct visualization of the rectum and sigmoid colon. However, colonoscopy is study of the whole colon lumen. Every patient with alarm signs have to be evaluated using colonoscopy. In younger patients, flexible sigmoidoscopy would be sufficient for further investigation of alarm signs. Colonic manometry is 24-hour measurement of pressure within the large bowel, using specific probes and portable recorders. Anorectal manometry is studying the pressure activity of anorectum during rest and defecation, along with rectal sensation, rectoanal reflexes, and anal sphincter function. Balloon expulsion test is a simple bedside test to evaluate the ability of patient to evacuate the artificial stool. Rectal biostat test consists of a very compliant plastic balloon, which is inserted into the rectum, concurrently connected to computer device to measure the pressure.
Other Diagnostic Studies
Endoscopy
| xWxdfhmXcNI|500}} |
- Endoscopic evaluation of patients with constipation include flexible sigmoidoscopy and colonoscopy. Flexible sigmoidoscopy is the direct visualization of the rectum and sigmoid colon. However, colonoscopy is study of the whole colon lumen.
- Based on American Society of Gastrointestinal Endoscopy guideline, alarm signs in constipated patients are as following:[1]
- Rectal bleeding
- Heme positive stool
- Iron deficiency anemia
- Weight loss
- Obstructive symptoms
- Recent onset of symptoms
- Rectal prolapse
- Change in stool caliber
- Every subjects older than 50 years without previous screening for colon cancer
- Every patient with alarm signs have to be evaluated using colonoscopy. In younger patients, flexible sigmoidoscopy would be sufficient for further investigation of alarm signs.
- Colonoscopy has lower yield and correlation with symptoms in patients with constipation alone. Therefore, it is better not to use in patients with constipation and without any alarm sign.
Colonic function tests
Colonic manometry
- Colonic manometry is 24-hour measurement of pressure within the large bowel, using specific probes and portable recorders.
- The colon pressure is studied during different conditions, such as:[2]
| 3Wgxhz9DwL8|500}} |
- Colonic manometry findings suggestive of constipation are:[3]
- Fewer pressure waves and lower area under the curve
- Decreased colonic motility induced by waking or meal
- Lower incidence and propagation velocity of high-amplitude propagating contractions (HAPCs)
Anorectal function tests
Anorectal manometry
- Anorectal manometry is studying the pressure activity of anorectum during rest and defecation, along with the followings:[4]
 |
- Rectoanal reflexes
- Anal sphincter function
- Anorectal manometry is used for the diagnosis of defecatory disorder (dyssynergism) and Hirschsprung disease.
- Lack of concordance between defecation propulsive pressure and reflex relaxation of the puborectalis and external anal sphincter muscles is the primary concern in dyssynergism. Based on anorectal manometry, there are four types of dyssynergic defecation.[5]
| Type | Intrarectal pressure | Intraanal pressure |
|---|---|---|
| 1 | ↑ | ↑ |
| 2 | - | ↑ |
| 3 | ↑ | - |
| 4 | - | - |
| Normal defecation | ↑ | ↓ |
Balloon expulsion test
- Balloon expulsion test is a simple bedside test to evaluate the ability of patient to evacuate the artificial stool.
- The balloon filled with 50 cc of warm water or silicone-filled stool-like device is inserted into the rectum and the subject is asked to evacuate the balloon in sitting position. Expulsion within 1 minute is assumed as normal.[6]
- The expulsion test has a specificity and sensitivity of 89% and 88%, respectively. While, negative and positive predictive values are 97% and 67%, respectively.[7]
 |
Rectal barotest test
- Rectal biostat test consists of a very compliant plastic balloon, which is inserted into the rectum, concurrently connected to computer device to measure the pressure.
- First, the balloon is inflated in the rectum and then the effect of various defecation maneuvers on the pressure will be recorded.
- Decreased intrarectal pressure during the defecation is suggestive of constipation secondary to dyssynergism.[9]
References
- ↑ Qureshi W, Adler DG, Davila RE, Egan J, Hirota WK, Jacobson BC, Leighton JA, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Baron TH, Faigel DO (2005). "ASGE guideline: guideline on the use of endoscopy in the management of constipation". Gastrointest. Endosc. 62 (2): 199–201. doi:10.1016/j.gie.2005.04.016. PMID 16046978.
- ↑ Rao SS, Sadeghi P, Beaty J, Kavlock R, Ackerson K (2001). "Ambulatory 24-h colonic manometry in healthy humans". Am. J. Physiol. Gastrointest. Liver Physiol. 280 (4): G629–39. doi:10.1152/ajpgi.2001.280.4.G629. PMID 11254489.
- ↑ Rao SS, Sadeghi P, Beaty J, Kavlock R (2004). "Ambulatory 24-hour colonic manometry in slow-transit constipation". Am. J. Gastroenterol. 99 (12): 2405–16. doi:10.1111/j.1572-0241.2004.40453.x. PMID 15571589.
- ↑ Karlbom U, Lundin E, Graf W, Påhlman L (2004). "Anorectal physiology in relation to clinical subgroups of patients with severe constipation". Colorectal Dis. 6 (5): 343–9. doi:10.1111/j.1463-1318.2004.00632.x. PMID 15335368.
- ↑ Rao SS, Mudipalli RS, Stessman M, Zimmerman B (2004). "Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus)". Neurogastroenterol. Motil. 16 (5): 589–96. doi:10.1111/j.1365-2982.2004.00526.x. PMID 15500515.
- ↑ Rao SS, Hatfield R, Soffer E, Rao S, Beaty J, Conklin JL (1999). "Manometric tests of anorectal function in healthy adults". Am. J. Gastroenterol. 94 (3): 773–83. doi:10.1111/j.1572-0241.1999.00950.x. PMID 10086665.
- ↑ Rao SS, Mudipalli RS, Stessman M, Zimmerman B (2004). "Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus)". Neurogastroenterol. Motil. 16 (5): 589–96. doi:10.1111/j.1365-2982.2004.00526.x. PMID 15500515.
- ↑ <"https://creativecommons.org/licenses/by-sa/2.5" title="Creative Commons Attribution-Share Alike 2.5">CC BY-SA 2.5, <"https://commons.wikimedia.org/w/index.php?curid=489883">
- ↑ Gladman MA, Lunniss PJ, Scott SM, Swash M (2006). "Rectal hyposensitivity". Am. J. Gastroenterol. 101 (5): 1140–51. doi:10.1111/j.1572-0241.2006.00604.x. PMID 16696790.