|
|
| (6 intermediate revisions by 3 users not shown) |
| Line 11: |
Line 11: |
| MeshID = D017700 | | | MeshID = D017700 | |
| }} | | }} |
| {{SI}} | | {{Cholesterol emboli syndrome}} |
| {{WikiDoc Cardiology Network Infobox}}
| | |
| {{CMG}} | | {{CMG}} |
|
| |
|
| {{Editor Help}}
| | ==[[Cholesterol emboli syndrome overview|Overview]]== |
|
| |
|
| == Overview == | | ==[[Cholesterol emboli syndrome historical perspective|Historical Perspective]]== |
| '''Cholesterol embolism''' (often '''cholesterol crystal embolism''' or '''atheroembolism''', sometimes '''blue toe''' or '''purple toe syndrome''' or '''trash foot''') occurs when [[cholesterol]] is released, usually from an [[atheroma|atherosclerotic plaque]], and travels along with the bloodsteam ([[embolism]]) to other places in the body, where it obstructs [[blood vessel]]s. Most commonly this causes skin symptoms (usually [[livedo reticularis]]), [[gangrene]] of the extremities and sometimes [[renal failure]]; problems with other organs may arise, depending on the site at which the cholesterol crystals enter the bloodstream.<ref name=Scolari>{{cite journal |author=Scolari F, Ravani P, Gaggi R, ''et al'' |title=The challenge of diagnosing atheroembolic renal disease: clinical features and prognostic factors |journal=Circulation |volume=116 |issue=3 |pages=298–304 |year=2007 |month=July |pmid=17606842 |doi=10.1161/CIRCULATIONAHA.106.680991 |url=http://circ.ahajournals.org/cgi/content/full/116/3/298}}</ref> When the [[kidney]]s are involved, the disease is referred to as '''atheroembolic renal disease''' (AERD).<ref name=Modi>{{cite journal |author=Modi KS, Rao VK |title=Atheroembolic renal disease |journal=J. Am. Soc. Nephrol. |volume=12 |issue=8 |pages=1781–7 |year=2001 |month=August |pmid=11461954 |doi= |url=http://jasn.asnjournals.org/cgi/content/full/12/8/1781}}</ref> The diagnosis usually involves [[biopsy]] (removing a tissue sample) from an affected organ. Cholesterol embolism is treated by removing the cause and with supportive therapy; [[statin]] drugs have been found to improve the prognosis.<ref name=Scolari/> CES is underdiagnosed and may mimic other diseases.
| |
|
| |
|
| ==History== | | ==[[Cholesterol emboli syndrome pathophysiology|Pathophysiology]]== |
| The phenomenon of embolisation of cholesterol was first recognized by the Danish [[physiology|physiologist]] Dr [[Peter Ludvig Panum]].<ref>{{cite journal | author=Panum PL | title=Experimentelle Beitrage zur Lehre von der Embolie | language=German | journal=Virchows Arch Pathol Anat Physiol | year=1862 | volume=25 | pages=308–310 | doi=10.1007/BF01879803}}</ref> Further pathological evidence that eroded atheroma was the source of emboli came from American [[pathology|pathologist]] Dr Curtis M. Flory, who reported the phenomenon in 3.4% of a large series of patients with severe atherosclerosis of the [[aorta]].<ref>{{cite journal | author=Flory CM | title=Arterial occlusions produced by emboli from eroded aortic atheromatous plaques | journal=Am J Pathol | year= 1945 | volume=21 | pages=549–565}} {{PMC|1934118}}</ref><ref name=Modi/>
| |
|
| |
|
| ==Pathophysiology== | | ==[[Cholesterol emboli syndrome causes|Causes]]== |
| Cholesterol emboli occur when atheromatous plaques rupture and release cholesterol crystals, either spontaneously or as a result of iatrogenesis.
| |
| Cholesterol emboli syndrome (CES) is defined as the occlusion of 55-900 um arterioles by cholesterol crystals after their dislodgment from eroded upstream atheromatous plaques. The occlusion site is subsequently surrounded by intimal tissue, fibrin and platelet thrombi, and foreign-body giant cells. | |
|
| |
| == Epidemiology and Demographics ==
| |
|
| |
|
| * Cholesterol emboli syndrome is more common in male patients (~75%) with severe [[atherosclerotic disease]], and often occurs days to weeks after an invasive procedure.
| | ==[[Cholesterol emboli syndrome differential diagnosis|Differentiating Cholesterol emboli syndrome from other Diseases]]== |
|
| |
|
| == Risk Factors == | | ==[[Cholesterol emboli syndrome epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| * Atherosclerotic cardiovascular disease, history of MI (myocardial infarction)
| | ==[[Cholesterol emboli syndrome risk factors|Risk Factors]]== |
| * Anticoagulation and perhaps thrombolytic therapy – perhaps because overlying thrombi do not form over eroded plaques
| |
| * Cardiopulmonary resuscitation
| |
| * [[Hypertension]]
| |
| * [[Aortic aneurysm]]
| |
| * [[Hypercholesterolemia]]
| |
| * Smoking history
| |
| * Male sex
| |
| * Age over 55 years
| |
| * Vascular procedures
| |
| * Invasive angiography, including interventional cardiac catheterizations
| |
| * Aortic aneurysm rupture or surgery
| |
| * Vascular surgery
| |
|
| |
|
| == Diagnosis == | | ==[[Cholesterol emboli syndrome screening|Screening]]== |
|
| |
|
| ===Common Cuases=== | | ==[[Cholesterol emboli syndrome natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| It is relatively unusual (25%) for cholesterol emboli to occur spontaneously; this usually happens in people with severe [[atherosclerosis]] of the large arteries such as the [[aorta]]. In the other 75% it is a complication of medical procedures involving the blood vessels, such as [[vascular surgery]] or [[angiography]]. In [[coronary catheterization]], for instance, the incidence is 1.4%.<ref name=Fukumoto>{{cite journal |author=Fukumoto Y, Tsutsui H, Tsuchihashi M, Masumoto A, Takeshita A |title=The incidence and risk factors of cholesterol embolization syndrome, a complication of cardiac catheterization: a prospective study |journal=J. Am. Coll. Cardiol. |volume=42 |issue=2 |pages=211–6 |year=2003 |month=July |pmid=12875753 |doi=10.1016/S0735-1097(03)00579-5 | url=http://linkinghub.elsevier.com/retrieve/pii/S0735109703005795}}</ref> Furthermore, cholesterol embolism may develop after the commencement of [[anticoagulant]]s or [[thrombolysis|thrombolytic]] medication that decrease blood clotting or dissolve blood clots, respectively. They probably lead to cholesterol emboli by removing blood clots that cover up a damaged atherosclerotic plaque; cholesterol-rich debris can then enter the bloodsteam.<ref name=Modi/>
| | ==Diagnosis== |
| | | [[Cholesterol emboli syndrome history and symptoms|History and Symptoms]] | [[Cholesterol emboli syndrome physical examination|Physical Examination]] | [[Cholesterol emboli syndrome laboratory findings|Laboratory Findings]] | [[Cholesterol emboli syndrome electrocardiogram|Electrocardiogram]] | [[Cholesterol emboli syndrome x ray|X Ray]] | [[Cholesterol emboli syndrome CT|CT]] | [[Cholesterol emboli syndrome MRI|MRI]] | [[Cholesterol emboli syndrome echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Cholesterol emboli syndrome other imaging findings|Other Imaging Findings]] | [[Cholesterol emboli syndrome other diagnostic studies|Other Diagnostic Studies]] |
| ===Complete Differential diagnosis===
| | ==Treatment== |
| Findings on general investigations (such as [[blood test]]s) are not specific for cholesterol embolism, which makes diagnosis difficult. The main problem is the distinction between cholesterol embolism and [[vasculitis]] (inflammation of the small blood vessels), which may cause very similar symptoms - especially the skin findings and the kidney dysfunction.<ref name=Modi/> Worsening kidney function after an angiogram may also be attributed to kidney damage by substances used during the procedure ([[Radiocontrast#Contrast-induced nephropathy|contrast nephropathy]]). Other causes that may lead to similar symptoms include [[acute tubular necrosis|ischemic renal failure]] (kidney dysfunction due to an interrupted blood supply), a group of diseases known as [[microangiopathic hemolytic anemia|thrombotic microangiopathies]] and [[endocarditis]] (infection of the [[heart valve]]s with small clumps of infected tissue embolizing through the body).<ref name=Modi/>
| | [[Cholesterol emboli syndrome medical therapy|Medical Therapy]] | [[Cholesterol emboli syndrome surgery|Surgery]] | [[Cholesterol emboli syndrome primary prevention|Primary Prevention]] | [[Cholesterol emboli syndrome secondary prevention|Secondary Prevention]] | [[Cholesterol emboli syndrome cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Cholesterol emboli syndrome future or investigational therapies|Future or Investigational Therapies]] |
| | | ==Case Studies== |
| | | [[Cholesterol emboli syndrome case study one|Case #1]] |
| === History and Symptoms ===
| |
| ==Signs and symptoms==
| |
| The symptoms experienced in cholesterol embolism depend largely on the organ involved. Non-specific symptoms often described are [[fever]], [[myalgia|muscle ache]] and [[weight loss#Unintentional weight loss|weight loss]]. Embolism to the legs causes a mottled appearance and purple discoloration of the [[toe]]s, smalls [[infarct]]s and areas of [[gangrene]] due to [[necrosis|tissue death]] that usually appear black, and areas of the skin that assume a marbled pattern known as ''[[Livedoid vasculitis|livedo reticularis]]''.<ref name=Modi/>
| |
| | |
| Kidney involvement leads to the symptoms of renal failure, which are non-specific but usually cause [[nausea]], reduced [[appetite]] ([[anorexia]]), raised [[blood pressure]] (hypertension), and occasionally the various symptoms of [[electrolyte disturbance]] such as an [[cardiac arrhythmia|irregular heartbeat]]. Some patients report [[hematuria]] (bloody urine) but this may only be detectable on microscopic examination of the urine. Increased amounts of [[protein]] in the urine may cause [[edema]] (swelling) of the skin (a combination of symptoms known as [[nephrotic syndrome]]).<ref name=Modi/>
| |
| | |
| If emboli have spread to the [[digestive tract]], reduced appetite, nausea and vomiting may occur, as well as nonspecific [[abdominal pain]], [[gastrointestinal hemorrhage]] (vomiting blood, or [[hematochezia|admixture of blood in the stool]]), and occasionally [[acute pancreatitis]] (inflammation of the [[pancreas]]).<ref name=Modi/>
| |
| | |
| Both the [[central nervous system]] (brain and [[spinal cord]]) and the [[peripheral nervous system]] may be involved. Emboli to the brain may cause [[stroke]]-like episodes, [[headache]] and episodes of loss of vision in one eye (known as [[amaurosis fugax]]).<ref name=Modi/> Emboli to the eye can be seen by [[ophthalmoscopy]] and are known as [[Hollenhorst plaque|plaques of Hollenhorst]].<ref name=Schwarcz>{{cite journal| author=Schwarcz TH, Eton D, Ellenby MI, Stelmack T, McMahon TT, Mulder S, Meyer JP, Eldrup-Jorgensen J, Durham JR, Flanigan DP, ''et al''|title=Hollenhorst plaques: retinal manifestations and the role of carotid endarterectomy| journal=J Vasc Surg. |volume=11|issue=5|pages=635-641|pmid=2335833|month=May}}</ref> Emboli to the spinal cord may cause [[paraparesis]] (decreased power in the legs) or [[cauda equina syndrome]], a group of symptoms due to loss of function of the distal part of the spinal cord - loss of control over the [[bladder]], [[rectum]] and skin sensation around the anus.<ref name=Modi/> If the blood supply to a single nerve is interrupted by an embolus, the result is loss of function in the muscles supplied by that nerve; this phenomenon is called a ''[[mononeuropathy]]''.<ref name=Modi/>
| |
| | |
| | |
| * CES may resemble a systemic [[vasculitis]] like PAN, with multiple scattered areas of ischemic damage, with skin, renal, extremity, intestinal, and neurologic manifestations.
| |
| * Signs of peripheral ischemia without large vessel disease
| |
| | |
| === Physical Examination === | |
| | |
| * Chest pain due to myocardial ischemia
| |
| * Paradoxical embolus: presence of [[patent foramen ovale]] or [[atrial septal defect]]
| |
| * Other rare manifestations include retinal lesions, splenic infarcts, prostatitis, orchitis, hemorrhagic cystitis
| |
| * Fever
| |
| | |
| === Abdomen ===
| |
| | |
| * Abdominal pain
| |
| *:* Occult blood positive stool due to ischemia of the stomach, small intestine and colon
| |
| *:* Less common manifestations include ischemic pancreatitis, focal liver cell necrosis and acalculous necrotizing cholecystitis.
| |
| * Renal failure
| |
| *:* Acute or step-wise worsening function
| |
| *:* Patients may demonstrate focal segmental glomerulosclerosis may be seen, presenting with progressive renal insufficiency, sometimes with significant proteinuria.
| |
| | |
| === Neurologic ===
| |
| * Neurologic abnormalities
| |
| *:* Mononeuritis multiplex
| |
| *:* CNS involvement
| |
| | |
| ==== Skin ====
| |
| * Cutaneous involvement – cutaneous involvement increases the likelihood of accurate diagnosis.
| |
| *:* Blue toes / nail bed infarctions
| |
| *:* Livedo reticularis – present in up to 50%
| |
| *:* Cyanosis, purpura, tender nodules, ulcerations, gangrene
| |
| | |
| == Laboratory Findings ==
| |
| ===Blood and urine===
| |
| Tests for [[inflammation]] ([[C-reactive protein]] and the [[erythrocyte sedimentation rate]]) are typically elevated, and abnormal [[liver enzyme]]s may be seen.<ref name=Modi/> If the kidneys are involved, tests of [[renal function]] (such as [[urea]] and [[creatinine]]) are elevated.<ref name=Modi/> The [[complete blood count]] may show particularly high numbers of a type of [[white blood cell]] known as ''[[eosinophil]]s'' (more than 0.5 billion per liter); this occurs in only 60-80% of cases, so normal eosinophil counts do not rule out the diagnosis.<ref name=Modi/><ref name=Fukumoto/> Examination of the urine may show [[red blood cell]]s (occasionally in [[urinary casts|casts]] as seen under the microscope) and increased levels of protein; in a third of the cases with kidney involvement, eosinophils can also be detected in the urine.<ref name=Modi/> If vasculitis is suspected, [[complement]] levels may be determined as reduced levels are often encountered in vasculitis; complement is a group of proteins that forms part of the innate [[immune system]]. Complement levels are frequently reduced in cholesterol embolism, limiting the use of this test in the distinction between vasculitis and cholesterol embolism.<ref>{{cite journal |author=Cosio FG, Zager RA, Sharma HM |title=Atheroembolic renal disease causes hypocomplementaemia |journal=Lancet |volume=2 |issue=8447 |pages=118–21 |year=1985 |month=July |pmid=2862317 |doi=10.1016/S0140-6736(85)90225-9}}</ref>
| |
| | |
| * Organ specific damage
| |
| *:* Renal failure - rapidly progressive in many cases <cite>greenberg</cite>
| |
| *:* Myocardial infarction - serum creatine kinase (CPK) and troponin elevation
| |
| *:* Mesenteric ischemia - Bloody (OB+) stool common
| |
| *:* Stroke
| |
| * Full septic picture may ensue
| |
| *:* Adult Respiratory Distress Syndrome (ARDS) <cite>greenberg</cite>
| |
| *:* Microangiopathic hemolysis (disseminated intravascular coagulopathy)
| |
| *:* Hypotension is usually a late finding
| |
| | |
| === Electrolyte and Biomarker Studies ===
| |
| | |
| * Peripheral eosinophilia <cite>moolenaarneth</cite>
| |
| * Urinary eosinophilia - usually in patients with cholesterol-renal disease
| |
| * May have leukocytosis (even >20K/µL) with left shift
| |
| * Hypocomplementemia is common
| |
| * Sed rates are nonspecifically elevated
| |
| * Thrombocytopenia due to aggregation and complement activation
| |
| | |
| === Other Diagnostic Studies === | |
| * Biopsy of lesions may be beneficial
| |
| *:* Biopsy of affected organs shows characteristic changes in about half<ref name=Fukumoto/> to 75%<ref name=Modi/> the clinically diagnosed cases.
| |
| *:* Biopsy of skin lesions is often revealing in patients with cutaneous involvement.
| |
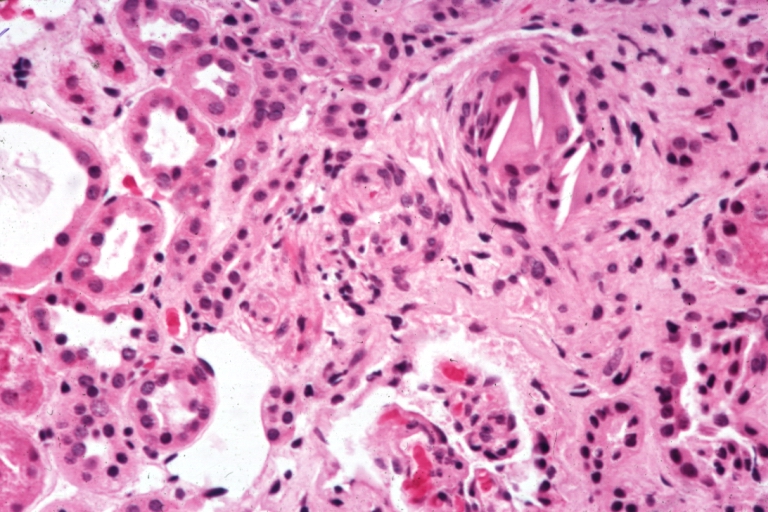
| *:* Transverse sections of affected arterioles, show occlusion of the lumen by biconvex needle-shaped cholesterol crystals, which dissolve during histologic processing to leave clefts, surrounded by fibrin and platelet thrombi, sometimes in association with foreign-body giant cells and intimal thickening.
| |
| | |
| == Risk Stratification and Prognosis==
| |
| | |
| * Many patients go on to amputation, renal failure, other organ system failure, and/or death.
| |
| * Mortality has not been well studied. The diagnosis may be difficult to make, and requires suspicion based upon clinical findings that often mimic other diseases. Therefore, the correct diagnosis is often never made, so the natural history and prognosis of all patients with CES is difficult to ascertain.
| |
| * Nevertheless, mortality been reported to be as high as 37-90%, biased by selection and report bias.
| |
| * Given the pathogenesis, one would expect a spectrum of disease, with probably significant numbers of subclinical, good prognosis patients.
| |
| | |
| == Treatment ==
| |
| Treatment of an episode of cholesterol emboli is generally symptomatic, i.e. it deals with the symptoms and complications but cannot reverse the phenomenon itself.<ref name=Fukumoto/> In kidney failure resulting from cholesterol crystal emboli, [[statin]]s have been shown to halve the risk of requiring [[hemodialysis]].<ref name=Scolari/>
| |
| * No definitive therapy at this time; supportive care, fluids
| |
| * The role of anticoagulation is not clear – some of advocated anticoagulation and others have warned against it.
| |
| * Some have advocated lipid-lowering agents.
| |
| * Unclear role for glucocorticoids, even when significant eosinophilia is present
| |
| *:* Anecdotal case reports have reported improvement
| |
| | |
| ==References==
| |
| {{reflist}}
| |
| | |
| ===Additional Reading===
| |
| #Rhodes, JM. Cholesterol emboli syndrome. Lancet 1996;347:1641.
| |
| #Mayo, RR, et al. Redefining the incidence of clinically detectable atheroembolism. Amer J Med 1996;100:524. PMID 8644764 | |
| #Kauffman, MG. Cholesterol emboli syndrome. Outlines in Clinical Medicine, 1997.
| |
| #Moolenaar, W, et al. Cholesterol crystal embolization in the Netherlands. Arch Int Med 1996;156:653. PMID 8629877
| |
| #Greenberg, A, et al. FSGS associated with cholesterol atheroembolism. Am J Kid Dis 1997;29:334. PMID 9041208
| |
| #Sijpkens, Y, et al. Vasculitis due to cholesterol embolism. Am J Med 1997;102:302. PMID 9217601
| |
| #Vidt, DG. Cholesterol emboli: a common cause of renal failure. Annu Rev Med 1997;48:375. PMID 9046969
| |
| #Moolenaar, W, et al. Cholesterol crystal embolism to the liver, gallbladder, and pancreas. Dig Dis Sci 1996;41:1819. PMID 8794801
| |
| | |
| == Acknowledgements ==
| |
| The content on this page was first contributed by: C. Michael Gibson, M.S>, M.D. and Ellison L. Smith, M.D.
| |
|
| |
|
| ==External links== | | ==External links== |
| Line 164: |
Line 46: |
| {{Vascular diseases}} | | {{Vascular diseases}} |
| {{Circulatory system pathology}} | | {{Circulatory system pathology}} |
| {{SIB}}
| |
| [[Category:Cardiology]]
| |
| [[Category:Nephrology]]
| |
| [[Category:Vascular surgery]]
| |
| [[Category:DiseaseState]]
| |
|
| |
|
| [[de:Cholesterinembolie-Syndrom]] | | [[de:Cholesterinembolie-Syndrom]] |
| Line 175: |
Line 52: |
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |
| | |
| | [[Category:Cardiology]] |
| | [[Category:Nephrology]] |
| | [[Category:Vascular surgery]] |
| | [[Category:Disease]] |