Central cord syndrome: Difference between revisions
No edit summary |
|||
| (5 intermediate revisions by the same user not shown) | |||
| Line 22: | Line 22: | ||
In the US the [[prevalence]] rate is 15.7-25% however this syndrome is generally associated with favorable prognosis for some degree of neurologic and functional recovery. CCS predominantly affects men more than women, similar to all other SCI. | In the US the [[prevalence]] rate is 15.7-25% however this syndrome is generally associated with favorable prognosis for some degree of neurologic and functional recovery. CCS predominantly affects men more than women, similar to all other SCI. | ||
==Historical Perspective== | ==Historical Perspective== | ||
*Central Cord Syndrome was first described by Schneider , et al in 1954.<ref name="GuestEleraky2002">{{cite journal|last1=Guest|first1=James|last2=Eleraky|first2=Mohammed A.|last3=Apostolides|first3=Paul J.|last4=Dickman|first4=Curtis A.|last5=Sonntag|first5=Volker K. H.|title=Traumatic central cord syndrome: results of surgical management|journal=Journal of Neurosurgery: Spine|volume=97|issue=1|year=2002|pages=25–32|issn=1547-5654|doi=10.3171/spi.2002.97.1.0025}}</ref> | |||
*Quencer, et al was the first to discover the association between neuroradiological and pathologic findings and the development of Central Cord Syndrome.<ref name="GuestEleraky2002">{{cite journal|last1=Guest|first1=James|last2=Eleraky|first2=Mohammed A.|last3=Apostolides|first3=Paul J.|last4=Dickman|first4=Curtis A.|last5=Sonntag|first5=Volker K. H.|title=Traumatic central cord syndrome: results of surgical management|journal=Journal of Neurosurgery: Spine|volume=97|issue=1|year=2002|pages=25–32|issn=1547-5654|doi=10.3171/spi.2002.97.1.0025}}</ref> | |||
*Raynor and Koplik described that the central part of the spinal cord was most affected when a moderate force was applied in an anterior posterior direction using the stress analysis theory.<ref name="GuestEleraky2002">{{cite journal|last1=Guest|first1=James|last2=Eleraky|first2=Mohammed A.|last3=Apostolides|first3=Paul J.|last4=Dickman|first4=Curtis A.|last5=Sonntag|first5=Volker K. H.|title=Traumatic central cord syndrome: results of surgical management|journal=Journal of Neurosurgery: Spine|volume=97|issue=1|year=2002|pages=25–32|issn=1547-5654|doi=10.3171/spi.2002.97.1.0025}}</ref> | |||
In | *In early 1970s surgical treatment was suggested by Quencer, et al to treat Central Cord syndrome.<ref name="GuestEleraky2002">{{cite journal|last1=Guest|first1=James|last2=Eleraky|first2=Mohammed A.|last3=Apostolides|first3=Paul J.|last4=Dickman|first4=Curtis A.|last5=Sonntag|first5=Volker K. H.|title=Traumatic central cord syndrome: results of surgical management|journal=Journal of Neurosurgery: Spine|volume=97|issue=1|year=2002|pages=25–32|issn=1547-5654|doi=10.3171/spi.2002.97.1.0025}}</ref> | ||
==Classification== | ==Classification== | ||
There is no established system for the classification of | There is no established system for the classification of Central Cord Syndrome. | ||
==Pathophysiology== | ==Pathophysiology== | ||
It is thought that Central Cord Syndrome is the result of Compression of the spinothalamic and corticospinal tracts of the spinal cord, is caused by either<ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref>. | |||
*Hyperextension injury.<ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
*Cervical spondylosis.<ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
*Arterial ischemia to the spinal cord<ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
*Central intraparenchymal spinal cord hematoma <ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
*Isolated injury to the decussating CorticoSpinal tracts in the brain stem. <ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
The | |||
==Causes== | ==Causes== | ||
Central Cord Syndrome can be caused by | |||
*Trauma( MVA, Falls, Diving)<ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
*Preexisting cervical spondylosis <ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
*Ischemia<ref name="HarropSharan2006">{{cite journal|last1=Harrop|first1=James S.|last2=Sharan|first2=Ashwini|last3=Ratliff|first3=Jonathon|title=Central cord injury: pathophysiology, management, and outcomes|journal=The Spine Journal|volume=6|issue=6|year=2006|pages=S198–S206|issn=15299430|doi=10.1016/j.spinee.2006.04.006}}</ref> | |||
== | |||
==Differentiating Central Cord Syndrome from other Diseases== | |||
Central Cord Syndrome must be differentiated from | |||
* Devic's Syndrome.<ref name="EpsteinHollingsworth2015">{{cite journal|last1=Epstein|first1=NancyE|last2=Hollingsworth|first2=Renee|title=Diagnosis and management of traumatic cervical central spinal cord injury: A review|journal=Surgical Neurology International|volume=6|issue=5|year=2015|pages=140|issn=2152-7806|doi=10.4103/2152-7806.156552}}</ref> | |||
* Primary Sjogren syndrome involving the Central Nervous System.<ref name="EpsteinHollingsworth2015">{{cite journal|last1=Epstein|first1=NancyE|last2=Hollingsworth|first2=Renee|title=Diagnosis and management of traumatic cervical central spinal cord injury: A review|journal=Surgical Neurology International|volume=6|issue=5|year=2015|pages=140|issn=2152-7806|doi=10.4103/2152-7806.156552}}</ref> | |||
* Multiple Sclerosis.<ref name="EpsteinHollingsworth2015">{{cite journal|last1=Epstein|first1=NancyE|last2=Hollingsworth|first2=Renee|title=Diagnosis and management of traumatic cervical central spinal cord injury: A review|journal=Surgical Neurology International|volume=6|issue=5|year=2015|pages=140|issn=2152-7806|doi=10.4103/2152-7806.156552}}</ref> | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
Latest revision as of 09:59, 1 September 2020
| Central Cord Syndrome | |
 | |
|---|---|
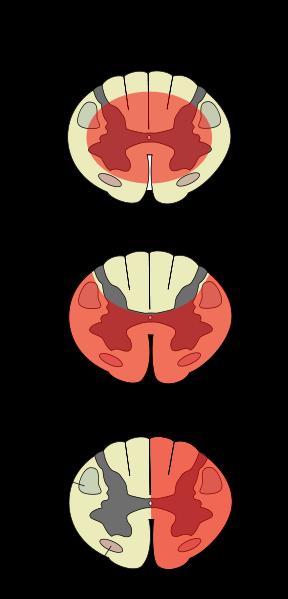
| Central cord syndrome is top diagram | |
| ICD-9 | 952.18 |
| DiseasesDB | 33409 |
| eMedicine | pmr/22 |
| MeSH | D020210 |
Central cord syndrome (CCS) is an acute cervical spinal cord injury (SCI), characterized by disproportionately greater motor impairment in upper compared to lower extremities, bladder dysfunction, and variable degree of sensory loss below the level of injury. This syndrome is unlike a complete lesion, that causes loss of all sensation and movement below the level of the injury. First described by Schneider in 1954,[1] CCS has been reported to occur more frequently among older persons with cervical spondylosis who sustain hyperextension injury. Though it also may occur in persons of any age. CCS is the most common incomplete SCI syndrome.
CCS most often occurs after hyperextension injury in an individual with long-standing cervical spondylosis. Historically, spinal cord damage was believed to originate from concussion or contusion of the cord with stasis of axoplasmic flow, causing edematous injury rather than destructive hematomyelia. More recently, autopsy studies have demonstrated that CCS may be caused by bleeding into the central part of the cord, portending less favorable prognosis. Studies also have shown that CCS probably is associated with axonal disruption in the lateral columns at the level of the injury to the spinal cord with relative preservation of the grey matter.
In the US the prevalence rate is 15.7-25% however this syndrome is generally associated with favorable prognosis for some degree of neurologic and functional recovery. CCS predominantly affects men more than women, similar to all other SCI.
Historical Perspective
- Central Cord Syndrome was first described by Schneider , et al in 1954.[2]
- Quencer, et al was the first to discover the association between neuroradiological and pathologic findings and the development of Central Cord Syndrome.[2]
- Raynor and Koplik described that the central part of the spinal cord was most affected when a moderate force was applied in an anterior posterior direction using the stress analysis theory.[2]
- In early 1970s surgical treatment was suggested by Quencer, et al to treat Central Cord syndrome.[2]
Classification
There is no established system for the classification of Central Cord Syndrome.
Pathophysiology
It is thought that Central Cord Syndrome is the result of Compression of the spinothalamic and corticospinal tracts of the spinal cord, is caused by either[3].
- Hyperextension injury.[3]
- Cervical spondylosis.[3]
- Arterial ischemia to the spinal cord[3]
- Central intraparenchymal spinal cord hematoma [3]
- Isolated injury to the decussating CorticoSpinal tracts in the brain stem. [3]
Causes
Central Cord Syndrome can be caused by
Differentiating Central Cord Syndrome from other Diseases
Central Cord Syndrome must be differentiated from
- Devic's Syndrome.[4]
- Primary Sjogren syndrome involving the Central Nervous System.[4]
- Multiple Sclerosis.[4]
Epidemiology and Demographics
The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide.
OR
In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide.
OR
In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%.
Patients of all age groups may develop [disease name].
OR
The incidence of [disease name] increases with age; the median age at diagnosis is [#] years.
OR
[Disease name] commonly affects individuals younger than/older than [number of years] years of age.
OR
[Chronic disease name] is usually first diagnosed among [age group].
OR
[Acute disease name] commonly affects [age group].
There is no racial predilection to [disease name].
OR
[Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name].
[Disease name] affects men and women equally.
OR
[Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1.
The majority of [disease name] cases are reported in [geographical region].
OR
[Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2].
Risk Factors
There are no established risk factors for [disease name].
OR
The most potent risk factor in the development of [disease name] is [risk factor 1]. Other risk factors include [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] include [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] may be occupational, environmental, genetic, and viral.
Screening
There is insufficient evidence to recommend routine screening for [disease/malignancy].
OR
According to the [guideline name], screening for [disease name] is not recommended.
OR
According to the [guideline name], screening for [disease name] by [test 1] is recommended every [duration] among patients with [condition 1], [condition 2], and [condition 3].
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4].
OR
The diagnosis of [disease name] is based on the [criteria name] criteria, which include [criterion 1], [criterion 2], and [criterion 3].
OR
The diagnosis of [disease name] is based on the [definition name] definition, which includes [criterion 1], [criterion 2], and [criterion 3].
OR
There are no established criteria for the diagnosis of [disease name].
History and Symptoms
The majority of patients with [disease name] are asymptomatic.
OR
The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
See also
References
- ↑ Schneider RC, Cherry G, Pantek H (1954). "The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine". J. Neurosurg. 11 (6): 546–77. PMID 13222164.
- ↑ 2.0 2.1 2.2 2.3 Guest, James; Eleraky, Mohammed A.; Apostolides, Paul J.; Dickman, Curtis A.; Sonntag, Volker K. H. (2002). "Traumatic central cord syndrome: results of surgical management". Journal of Neurosurgery: Spine. 97 (1): 25–32. doi:10.3171/spi.2002.97.1.0025. ISSN 1547-5654.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Harrop, James S.; Sharan, Ashwini; Ratliff, Jonathon (2006). "Central cord injury: pathophysiology, management, and outcomes". The Spine Journal. 6 (6): S198–S206. doi:10.1016/j.spinee.2006.04.006. ISSN 1529-9430.
- ↑ 4.0 4.1 4.2 Epstein, NancyE; Hollingsworth, Renee (2015). "Diagnosis and management of traumatic cervical central spinal cord injury: A review". Surgical Neurology International. 6 (5): 140. doi:10.4103/2152-7806.156552. ISSN 2152-7806.
- http://health.enotes.com/neurological-disorders-encyclopedia/central-cord-syndrome
- http://www.ninds.nih.gov/disorders/central_cord/central_cord.htm
Template:Disease-stub Template:Lesions of spinal cord and brainstem