Breast cancer mammography: Difference between revisions
Jump to navigation
Jump to search
(Mahshid) |
No edit summary |
||
| Line 8: | Line 8: | ||
==Disadvantages== | ==Disadvantages== | ||
* Evidence in favor of mammographic diagnostic screening comes from eight randomized clinical trials from the 1960s through 1980s. Many of these trials have been criticised for methodological errors, and the results were summarized in a review article published in 1993.<ref name=Fletcher_1993>{{cite journal | author = Fletcher SW, Black W, Harris R, Rimer BK, Shapiro S | title = Report of the International Workshop on Screening for Breast Cancer | journal = J. Natl. Cancer Inst. | volume = 85 | issue = 20 | pages = 1644-56 | year = 1993 | pmid = 8105098 | doi = | accessdate = 2007-05-26}}</ref> | * Evidence in favor of mammographic diagnostic screening comes from eight randomized clinical trials from the 1960s through 1980s. Many of these trials have been criticised for methodological errors, and the results were summarized in a review article published in 1993.<ref name="Fletcher_1993">{{cite journal | author = Fletcher SW, Black W, Harris R, Rimer BK, Shapiro S | title = Report of the International Workshop on Screening for Breast Cancer | journal = J. Natl. Cancer Inst. | volume = 85 | issue = 20 | pages = 1644-56 | year = 1993 | pmid = 8105098 | doi = | accessdate = 2007-05-26}}</ref> | ||
* False positives are a major problem of mammographic breast cancer screening. Approximately 7% of all mammographic screenings are false positives. <ref name="pmid17404352">{{cite journal| author=Brewer NT, Salz T, Lillie SE| title=Systematic review: the long-term effects of false-positive mammograms. | journal=Ann Intern Med | year= 2007 | volume= 146 | issue= 7 | pages= 502-10 | pmid=17404352 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17404352 }} </ref> | * False positives are a major problem of mammographic breast cancer screening. Approximately 7% of all mammographic screenings are false positives. <ref name="pmid17404352">{{cite journal| author=Brewer NT, Salz T, Lillie SE| title=Systematic review: the long-term effects of false-positive mammograms. | journal=Ann Intern Med | year= 2007 | volume= 146 | issue= 7 | pages= 502-10 | pmid=17404352 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17404352 }} </ref> | ||
:*Data reported in the UK Million Woman Study indicates that if 134 mammograms are performed, 20 women will be called back for suspicious findings, and four biopsies will be necessary, to diagnose one cancer. Recall rates are higher in the U.S. than in the UK.<ref name="pmid15814020">{{cite journal |author=Smith-Bindman R, Ballard-Barbash R, Miglioretti DL, Patnick J, Kerlikowske K |title=Comparing the performance of mammography screening in the USA and the UK |journal=Journal of medical screening |volume=12 |issue=1 |pages=50-4 |year=2005 |pmid=15814020 |doi=10.1258/0969141053279130}}</ref> | :*Data reported in the UK Million Woman Study indicates that if 134 mammograms are performed, 20 women will be called back for suspicious findings, and four biopsies will be necessary, to diagnose one cancer. Recall rates are higher in the U.S. than in the UK.<ref name="pmid15814020">{{cite journal |author=Smith-Bindman R, Ballard-Barbash R, Miglioretti DL, Patnick J, Kerlikowske K |title=Comparing the performance of mammography screening in the USA and the UK |journal=Journal of medical screening |volume=12 |issue=1 |pages=50-4 |year=2005 |pmid=15814020 |doi=10.1258/0969141053279130}}</ref> | ||
| Line 26: | Line 26: | ||
:*[[Lotion]] | :*[[Lotion]] | ||
*The outcome of a mammogram may be [[benign]] or may require further investigation. If the cause cannot be determined to be benign with sufficient certainty, a [[biopsy]] will be recommended. | *The outcome of a mammogram may be [[benign]] or may require further investigation. If the cause cannot be determined to be benign with sufficient certainty, a [[biopsy]] will be recommended. | ||
* | |||
* | |||
* | |||
* Serial mammography might slightly increase the risk of developing breast cancer in high-risk patients such as patients with a family history of breast cancer and patients with known genetic carcinogenic mutations. | |||
:* According to a recently published study by Jansen-van der Weide et.al. average increased the risk of breast cancer because of low-dose radiation exposure was (OR between 1.3 and 2 with respect to the patients' risk and exposure) observed compared to that of high-risk women not exposed to low-dose radiation. | |||
:* Pooled OR revealed an increased risk of breast cancer among high-risk women due to low-dose radiation exposure (OR = 1.3, 95% CI: 0.9- 1.8). | |||
:* Exposure before age 20 (OR = 2.0, 95% CI: 1.3-3.1) | |||
:* A mean of ≥5 exposures (OR = 1.8, 95% CI: 1.1-3.0) | |||
:* When using low-dose radiation among high-risk women, a careful approach is needed, by means of | |||
:* They recommended careful approach in these subgroup of patients as follows: | |||
::* Reducing repeated exposure, | |||
::* Avoidance of exposure at a younger age | |||
::* Using non-ionising screening techniques. | |||
:* According to another study by Diana L. Miglioretti et.al. radiation-induced breast cancer incidence and mortality from digital mammography screening are impacted by: | |||
::* Dose variability from screening and resultant diagnostic work-up, | |||
::* Initiation age | |||
::* Screening frequency. | |||
::* Women with large breasts may be at higher risk of radiation-induced breast cancer; | |||
* '''''However, we should keep in mind that "the benefits of screening outweigh these risks".''''' | |||
==References== | ==References== | ||
Revision as of 14:02, 2 April 2019
|
Breast Cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Breast cancer mammography On the Web |
|
American Roentgen Ray Society Images of Breast cancer mammography |
|
Risk calculators and risk factors for Breast cancer mammography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Assistant Editor(s)-In-Chief: Jack Khouri; Ammu Susheela, M.D. [2]
Overview
Mammography may be performed to detect breast cancer.
Advantages
- Mammography has been estimated to reduce breast cancer-related mortality by 20-30%.[1]
Disadvantages
- Evidence in favor of mammographic diagnostic screening comes from eight randomized clinical trials from the 1960s through 1980s. Many of these trials have been criticised for methodological errors, and the results were summarized in a review article published in 1993.[2]
- False positives are a major problem of mammographic breast cancer screening. Approximately 7% of all mammographic screenings are false positives. [3]
- Data reported in the UK Million Woman Study indicates that if 134 mammograms are performed, 20 women will be called back for suspicious findings, and four biopsies will be necessary, to diagnose one cancer. Recall rates are higher in the U.S. than in the UK.[4]
- Mammography in women under 50 years of age can be imprecise due to mammographic breast density. Breast density is an independent adverse prognostic factor on breast cancer prognosis. [5]
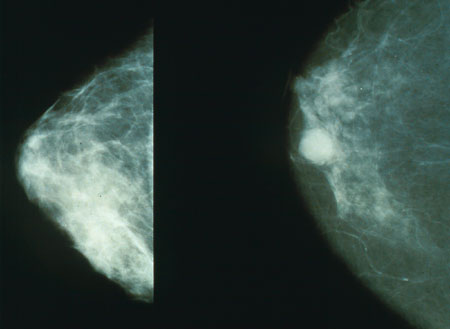
Procedure
- After a screening mammogram, some women may have areas of concern which can't be resolved with only the information available from the screening mammogram. They would then be called back for a "diagnostic mammogram". This phrase is essentially a problem-solving mammogram. During this session, the radiologist will be monitoring each of the additional films as they are taken to determine the cause of the abnormal appearance.
- During the procedure, the breast is compressed by a dedicated mammography machine to:
- Even out the tissue
- Increase image quality
- Hold the breast still (preventing motion blur).
- Due to imaging limitations, some elements may show up on x-ray as calcium spots. For this reason, women are discourage from applying the following on the day of the mammogram.
- The outcome of a mammogram may be benign or may require further investigation. If the cause cannot be determined to be benign with sufficient certainty, a biopsy will be recommended.
- Serial mammography might slightly increase the risk of developing breast cancer in high-risk patients such as patients with a family history of breast cancer and patients with known genetic carcinogenic mutations.
- According to a recently published study by Jansen-van der Weide et.al. average increased the risk of breast cancer because of low-dose radiation exposure was (OR between 1.3 and 2 with respect to the patients' risk and exposure) observed compared to that of high-risk women not exposed to low-dose radiation.
- Pooled OR revealed an increased risk of breast cancer among high-risk women due to low-dose radiation exposure (OR = 1.3, 95% CI: 0.9- 1.8).
- Exposure before age 20 (OR = 2.0, 95% CI: 1.3-3.1)
- A mean of ≥5 exposures (OR = 1.8, 95% CI: 1.1-3.0)
- When using low-dose radiation among high-risk women, a careful approach is needed, by means of
- They recommended careful approach in these subgroup of patients as follows:
- Reducing repeated exposure,
- Avoidance of exposure at a younger age
- Using non-ionising screening techniques.
- According to another study by Diana L. Miglioretti et.al. radiation-induced breast cancer incidence and mortality from digital mammography screening are impacted by:
- Dose variability from screening and resultant diagnostic work-up,
- Initiation age
- Screening frequency.
- Women with large breasts may be at higher risk of radiation-induced breast cancer;
- However, we should keep in mind that "the benefits of screening outweigh these risks".
References
- ↑ Elwood J, Cox B, Richardson A. "The effectiveness of breast cancer screening by mammography in younger women". Online J Curr Clin Trials. Doc No 32: [23, 227 words, 195 paragraphs]. PMID 8305999.
- ↑ Fletcher SW, Black W, Harris R, Rimer BK, Shapiro S (1993). "Report of the International Workshop on Screening for Breast Cancer". J. Natl. Cancer Inst. 85 (20): 1644–56. PMID 8105098.
|access-date=requires|url=(help) - ↑ Brewer NT, Salz T, Lillie SE (2007). "Systematic review: the long-term effects of false-positive mammograms". Ann Intern Med. 146 (7): 502–10. PMID 17404352.
- ↑ Smith-Bindman R, Ballard-Barbash R, Miglioretti DL, Patnick J, Kerlikowske K (2005). "Comparing the performance of mammography screening in the USA and the UK". Journal of medical screening. 12 (1): 50–4. doi:10.1258/0969141053279130. PMID 15814020.
- ↑ Armstrong K, Moye E, Williams S, Berlin JA, Reynolds EE (2007). "Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians". Ann. Intern. Med. 146 (7): 516–26. PMID 17404354.