Acute coronary syndrome resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Charmaine Patel, M.D. [2]
Patient Presentation
- Substernal / precordial chest pressure / heaviness / pain
- Pain radiation to shoulder or arm / neck / jaw
- Nausea and/or vomiting
- Shortness of breath
- Diaphoresis
- Heartburn/ burning sensation in chest
- Dizziness
- Palpitations
- Near syncope / syncope
Initial Evaluation and Orders
- Ensure patency of airway, check for adequate breathing and circulation.
- Vital signs (pulse rate, blood pressure, respiratory rate, temperature, and oxygen saturation)
- 12-lead EKG (compare with old EKG if possible)
- Cardiac enzymes (three sets of troponin, CK, CK-MB at six hour intervals; first set may be normal, but order all three sets)
- Obtain complete blood count and basic metabolic panel.
- Chest x-ray
- Oxygen (titrate for oxygen saturation levels >92%)
- IV access
- Give IV morphine for persistent discomfort or anxiety
- 325mg non-enteric coated aspirin by mouth (or per rectum if patient cannot take orally)
- If patient is not hypotensive and inferior myocardial infarction has been ruled out by EKG, give 0.4mg nitroglycerin sublingually up to three times, at 5 minute intervals, until chest pain improves.
- If pulmonary embolism is suspected D-dimers should be obtained.
| Important |
| Follow up with all pending tests and lab results as soon as these become available. For information on evaluating the results go to the apppropriate section on this page. |
History and Symptoms
- History of Present Illness:
- Chest pain history; ask about onset, duration, nature, intensity, location, progression, radiation to arm, neck, jaw (acute coronary syndrome) or to back (aortic dissection), aggravating (pleuritic and pericarditis chest pain worsens with respiration) and relieving factors (such as nitrates or rest), constant or intermittent. Ask about any precipitating factors (trauma, physical strain, emotional distress).
- Ask about associated symptoms (head to toe): Headache, confusion, fever, photophobia, vision changes, bleeding, nausea, vomiting, apetite, weight loss, shortness of breath, palpitations, cough, sputum, abdominal pain, bowel symptoms, urinary symptoms.
- Past Medical History: History of stable/unstable angina, past myocardial infarction. Ask about history of hypertension, diabetes, hyperlipidemia, hypercoagulable state, stroke and TIA.
- Past Surgical History: Percutaneous coronary intervention, coronary artery bypass graft.
- Social History: History of smoking, alcohol use, illicit drug use.
- Family History: Family history of premature coronary artery disease in a first degree male relative <55 years of age, or a first degree female relative <65 years old. Family history of myocardial infarction, hypertension, diabetes, stroke, or hypercoagulable state.
- Medications: Obtain a list of home medications.
- Allergies: Obtain a history of allergic reactions.
Physical Examination
- General
- Check for alertness, and orientation with time, place, and person
- Patient leaning forward can point towards pericarditis
- HEENT:
- Auscultate carotid artery (check for bruit)
- Jugular venous distension, check for hepatojugular reflex
- Cardiovascular:
- Vital signs
- Pulse Rate (rate, rhythm. volume, quality, symmetry, all 4 limbs. Aortic dissection- Diminution or absence of pulses)
- Blood pressure (check for symmetry in all the limbs)
- Inspection: Check for displacement of the apex.
- Palpation: Confirm the findings of inspection (cardiac apex), musculo-skeletal tenderness, crepitus (esophageal rupture,subcutaneous emphysema), feel for any thrill (possible regurgitation), heave (right ventricular hypertrophy)
- Auscultation:
- Heart sounds (muffled in cardiac tamponade, Pericardial effusion), S3 and S4 (Heart failure)
- Murmur (commonly regurgitation murmur)
- Pericardial rub - (Pericarditis, commonly tricuspid area sounds like scratching), and gallop
- Vital signs
- Respiratory:
- Inspection: Observe for symmetry of chest movement, evidence of flail chest, tracheal deviation (pneumothorax).
- Palpation : Check for muscle tenderness, tracheal deviation, and chest wall movement.
- Percussion: Percuss all lung fields for dullness (effusion), or hyperresonance to percussion on the affected side (pneumothorax).
- Auscultation: Decreased breath sounds (effusion and tension pneumothorax), crackles (pleural effusion) rales (heart failure).
- Extremities: Check for pedal edema.
Differential Diagnosis
EKG Findings
Electrocardiogram in Unstable angina / NSTEMI
- No changes
- Non specific ST / T wave changes
- Flipped or inverted T waves
- ST Depression as shown below. Greater magnitudes of downsloping ST depression are associated with a poorer prognosis.
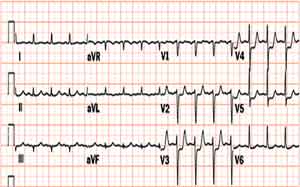
Electrocardiogram in STEMI
- ≥2 mm of ST segment elevation in 2 contiguous precordial leads
- ≥1mm in other leads (2 contiguous)
- An initial Q wave or abnormal R wave
- Additionally, new left bundle branch block and those with a true posterior MI are considered STEMI
- Specific types of STEMI:
- Anterior STEMI: ST elevation in the precordial leads + I and aVL (Left anterior descending artery)
- Posterior STEMI: ST elevations in II, III and aVF, reciprocal ST depressions in V1-V3, may have component of inferior ischemia (Left Circumflex artery)
- Inferior STEMI: ST elevation in II, III and aVF. When inferior MI is suspected a R - sided precordial leads is useful (ST elevation). Reciprocal changes in I and aVL (Right coronary artery or Left circumflex artery)
Chest X Ray Findings
- Aortic dissection: Suspect aortic dissection if findings include increased aortic diameter, widened mediastinum, and/or pleural effusion (hemothorax) in the absence of CHF
- Pulmonary embolism: May not appreciate any abnormalities on chest x ray.
- Tension pneumothorax: No pulmonary vessels are visible beyond the visceral pleural line. Tracheal deviation away from the collapsed area of lung will be seen.
- Esophageal rupture:The most common findings are pleural effusion, pneumothorax, pneumomediastinum, or subcutaneous emphysema.
- Heart failure: Cardiomegaly, and pulmonary congestion (Kerley B lines), may be seen. Obliteration of costophrenic angle may be seen in pleural effusion.
Laboratory Findings
- Check for elevation in CK, CK-MB, and troponin levels. If EKG changes are not present but enzymes are elevated, this can point to a diagnosis of Non-ST elevation myocardial infarction.
- Check basic metabolic panel for electrolyte abnormalities and correct accordingly. BUN and Creatinine levels should be checked in preparation the possible need for contrast during PCI.
- Elevated D-dimer levels >500ng/ml is considered abnormal, and may be indicative of a pulmonary embolism.
Management
If positive EKG findings are present consistent with acute coronary syndrome, OR if the patient history is highly suggestive of acute coronary syndrome despite a negative EKG, perform the following measures.
- Page the cardiology fellow and activate the cardiac catheterization lab.
- Give the patient loading doses of
- Aspirin 325mg non-enteric coated by mouth or per rectum, if not given previously.
- Clopidogrel 600mg by mouth loading dose OR ticagrelor 180mg loading dose.
- Heparin 60 to 100 units/kg, up to a maximum of 4000 units for an aPTT of 50 to 70 seconds.
- Atorvastatin 80mg or simvastatin 40mg.
- Metoprolol 25 mg by mouth if there are no signs of heart failure, hemodynamic compromise, bradycardia, or severe reactive airway disease.
Acute STEMI management:
• Select reperfusion strategy: PCI strongly preferred, especially for patients with cardiogenic shock, heart failure, late presentation, or contraindications to fibrinolysis.
• For patients with symptoms of >12 hours, fibrinolytic therapy is not indicated, but emergent PCI may be considered, particularly for patients with evidence of ongoing ischemia or those at high risk.
• Treat with fibrinolysis if PCI unavailable within 90-120 minutes, symptoms <12 hours, and no contraindications
• Give antiplatelet therapy (in addition to aspirin): clopidogrel 600 mg (300mg if fibrinolysis or no PCI). Consider adding glycoprotein IIb/IIIa inhibitor if PCI is planned.
• Give anticoagulant therapy: Unfractionated heparin (UFH) for patients undergoing PCI (IV bolus of 50 to 70 units/kg). Bivalirudin is an acceptable alternative to heparin in patients undergoing primary PCI. Enoxaparin only for patients not managed with PCI and GFR>30.
Other Diagnostic Work-up
- If esophageal rupture is suspected, a contrast-enhanced esophageal radiography is diagnostic.
- If pulmonary embolism is suspected, spiral CT scan should be obtained.
- If aortic dissection is suspected, obtain a CT scan with contrast.
- If cardiac tamponade is suspected, obtain an echocardiogram.