AV nodal reentrant tachycardia
| AV nodal reentrant tachycardia | |
 | |
|---|---|
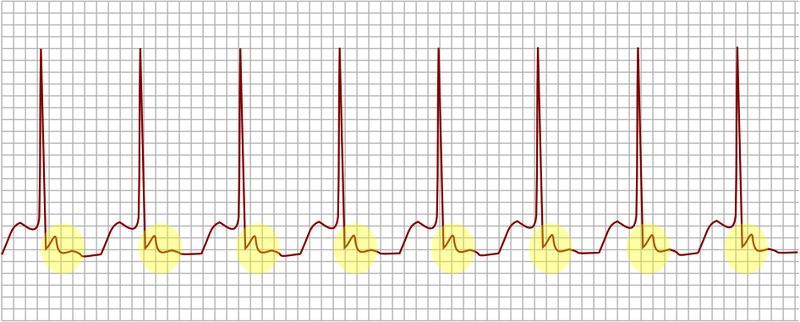
| AV nodal reentrant tachycardia. In yellow, is evidenced the P wave that falls after the QRS complex. | |
| ICD-10 | I47.1 |
| ICD-9 | 426.89, 427.0 |
| MeSH | D013611 |
|
AVNRT Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
AV nodal reentrant tachycardia On the Web |
|
American Roentgen Ray Society Images of AV nodal reentrant tachycardia |
|
Risk calculators and risk factors for AV nodal reentrant tachycardia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: AVNRT; AV node reentrant tachycardia; AV nodal reentry tachycardia; AV node reentry tachycardia; atrioventricular node reentrant tachycardia; atrioventricular nodal reentry tachycardia; atrioventricular node reentry tachycardia;
Overview
Historical Perspective
Pathophysiology
Classification
Risk Factors
Underlying structural heart disease is generally absent. Often, there is no precipitant of an episode. Risk factors for precipitation of AVNRT include:
- Alcohol
- Caffeine
- Chocolate
- Hyperthyroidism
- Hypokalemia
- Hypomagnesemia
- Myocardial ischemia
- Psychological stress
- Tea
- Theobromine in foods like tea, coffee and chocolate
- Theophylline
Differentiating Supraventricular Tachycardias
Supraventricular tachycardias must be differentiated from each other because the managment strategies may vary:
Atrial Fibrillation
- Rate: 110 to 180 bpm
- Rhythm: Irregularly irregular
- P waves: Absent, fibrillatory waves
- PR interval: Absent
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology in the absence of abberant conduction
- Response to Maneuvers: Does not break with adenosine or vagal maneuvers
- Epidemiology and Demographics: More common in the elderly, following bypass surgery, in mitral valve disease, hyperthyroidism
Atrial Flutter
- Rate: 75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) bpm, but 150 is most common
- Rhythm: Regular
- P waves: Sawtooth pattern of P waves at 250 to 350 beats per minute
- PR interval: Varies depending upon the magnitude of the block, but is short
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology
- Response to Maneuvers: Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm
- Epidemiology and Demographics: More common in the elderly, after alcohol
AV Nodal Reentry Tachycardia
- Rate: In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm.
- Rhythm: Regular
- P waves: The p wave is usually superimposed on or buried within the QRS complex
- PR interval: The PR interval cannot be calculated as the p wave is generally obscured by the QRS complex. In uncommon AVNRT, the p wave can appear after the QRS complex and before the T wave, and in atypical AVNRT, the p wave can appear just before the QRS complex.
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology in the absence of abberant conduction, QRS alternans may be present
- Response to Maneuvers: May break with adenosine or vagal maneuvers
- Epidemiology and Demographics: Accounts for 60%-70% of all SVTs. 80% to 90% of cases are due to antegrade conduction down a slow pathway and retrograde up a fast pathway.
AV Reciprocating Tachycardia
- Rate: More rapid than AVNRT
- Rhythm:
- P waves:
- PR interval:
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology
- Response to Maneuvers: May break with adenosine or vagal maneuvers
- Epidemiology and Demographics: More common in males, whereas AVNRT is more common in females, Occurs at a younger age
Junctional Tachycardia
- Rate: > 60 beats per minute
- Rhythm: Regular
- P waves: Usually inverted, may be burried in the QRS complex
- PR interval: The p wave is usually buried in the QRS complex
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology
- Response to Maneuvers: Does not break with adenosine or vagal maneuvers
- Epidemiology and Demographics: Common after heart surgery, digoxin toxicity, as an escape rhythm in AV block
Multifocal Atrial Tachycardia
- Rate: Atrial rate is > 100 beats per minute (bpm)
- Rhythm:
- P waves: P waves of varying morphology from at least three different foci, absence of one dominant atrial pacemaker, can be mistaken for atrial fibrillation if the P waves are of low amplitude
- PR interval: Variable PR intervals, RR intervals, and PP intervals
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology
- Response to Maneuvers: Does not terminate with adenosine or vagal maneuvers
- Epidemiology and Demographics: * High incidence in the elderly and in those with COPD
Sinus Node Reentry Tachycardia
- Rate:
- Rhythm:
- P waves: Upright P waves precede each regular, narrow QRS complex
- PR interval:
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology
- Response to Maneuvers: Although it cannot be distinguished on the surface 12 lead EKG from sinus tachycardia, SA node reentry tachycardia does often terminate with vagal maneuvers unlike sinus tachycardia.
- Epidemiology and Demographics:
Sinus tachycardia
- Rate: Greater than 100.
- Rhythm: Regular.
- P waves: Upright, consistent, and normal in morphology (if no atrial disease)
- PR interval: Between 0.12–0.20 seconds and shortens with increasing heart rate
- QRS complex: Less than 0.12 seconds, consistent, and normal in morphology
- Response to Maneuvers:
- Epidemiology and Demographics:
Ventricular Tachycardia
- Rate:
- Rhythm: Generally regular
- P waves: Normal morphology, upright, but dissociated from the QRS complex (i.e. "march through" the QRS complex)
- PR interval:
- QRS complex: Wide and greater than 0.12 seconds
- Response to Maneuvers: Does not terminate in response to adenosine or vagal maneuvers
- Epidemiology and Demographics:
- Risk Factors:: Occurs in the context of myocardial ischemia, myocardial infarction, congestive heart failure, drug toxicity, and inhereted channelopathies
Wolff-Parkinson-White syndrome
- Pathophysiology: Anatomically and functionally, the fast and slow pathways of AVNRT should not be confused with the accessory pathways that give rise to Wolff-Parkinson-White syndrome (WPW) syndrome or atrioventricular re-entrant tachycardia (AVRT). In AVNRT, the fast and slow pathways are located within the right atrium in close proximity to or within the AV node and exhibit electrophysiologic properties similar to AV nodal tissue. Accessory pathways that give rise to WPW syndrome and AVRT are located in the atrioventricular valvular rings, they provide a direct connection between the atria and ventricles, and have electrophysiologic properties similar to ventricular myocardium.
- Rate:
- Rhythm:
- P waves: In WPW with orthodromic conduction due to a bypass tract, the p wave generally follows the QRS complex, whereas in AVNRT, the p wave is generally buried in the QRS complex.
- PR interval:
- QRS complex: In WPW there is a delta wave and evidence of ventricular preexcitation if there is conduction to the ventrilce via antegrade conduction down an accessory pathway. It should be noted, however, that in some patients with WPW, a delta wave and pre-excitation may not be present because bypass tracts do not conduct antegrade.
- Response to Maneuvers: May break in response to procainamide, adenosine, vagal maneuvers
- Epidemiology and Demographics:
- Risk Factors: None, an inhereted disorder
Epidemiology and Demographics
AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia and accounts for 60% to 70% of these cases.
Sex
The ratio of female to male involvement is 3:1
Age
There is no age predilection.
Natural History, Complications, Prognosis
Natural History
The rhythm often ceases abruptly and spontaneously. An episode generally last seconds to hours.
Complications
- Some patients will develop syncope during episodes of AVRNT. The mechanism of syncope may be due to a reduction of cardiac output and hemodynamic compromise as a result of the short ventricular filling time or alternatively it may be due to transient asystole due to tachycardia-mediated suppression of the sinus node when the rhythm terminates. Those patients who do become symptomatic during episodes of AVNRT (i.e. have syncope) should avoid activities where the occurrence of hemodynamic compromise would endanger their safety or that of others (like driving).
- In patients with underlying ischemic heart disease, demand-related myocardial ischemia, angina and even myocardial infarction and/or congestive heart failure can occur.
- Tachycardia mediated cardiomyopathy
Prognosis
AVNRT is rarely life threatening and in the absence of underlying structural heart disease, the prognosis is good. Radiofrequency ablation is curative in 95% of cases.
Diagnosis
Symptoms
The following symptoms may be present:
- Sudden onset and sudden offset of rapid palpitations is common
- Dizziness and rarely syncope, especially at the onset of the episode of tachycardia
- Neck "pounding" may occur as a result of the right atrium contracting against a closed atrioventricular valve and Cannon a waves[1][2] and the simultaneous occurrence of the atrial and ventricular contractions.
- Chest pain and angina if the patient has ischemic heart disease
- Dyspnea
- Polyuria can occur after the episode breaks. It has been hypothesized that this is due to the release of atrial natriuretic peptide
Physical Examination
Pulse
The heart rate is typically regular and between 140-280 bpm. In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm.
Systolic Blood Pressure
- Hypotension may be present in some cases.
Neck
- Cannon a waves may be present in some cases
Lungs
- Rales may be present in some patients with congestive heart failure
Laboratory Studies
Depending upon the patient's history and demographics, the following laboratory studies should be considered:
- Thyroid function tests (TFTs) - an overactive thyroid may increase the risk of AVNRT
- Electrolytes - hypokalemia, hypomagnesemia may predispose to AVNRT
- Cardiac markers - if there is a concern that myocardial infarction (a heart attack) has occurred either as a cause or as a result of the AVNRT; this is usually only the case if the patient has experienced ischemic chest pain
Electrocardiogram
An electrocardiogram performed during the occurrence of symptoms may confirm the diagnosis of AVNRT.
Slow-Fast AVNRT (Common AVNRT)
- This form of AVNRT accounts for 80% to 90% of cases of AVNRT.
- The retrograde P wave that is conducted retrograde up the fast pathway is usually burried within the QRS but less frequently may be observed at the end of the QRS complex as a pseudo r’ wave in lead V1 or an S wave in leads II, III or aVF.
Fast-Slow AVNRT (Uncommon AVNRT)
- This form of AVNRT Accounts for 10% of cases of AVNRT
- In this form of AVNRT, the impulse is first conducted antegrade down the Fast AV nodal pathway and is then conducted retrograde up the Slow AV nodal pathway.
- In contrast to Common AVNRT, a retrograde P wave may be observed after the QRS complex before the T wave
Slow-Slow AVNRT (Atypical AVNRT)
- This form of AVNRT accounts for 1-5% of cases of AVNRT
- In this form of AVNRT, the impulse is first conducted antegrade down the Slow AV nodal pathway and retrograde up the Slow left atrial fibres approaching the AV node.
- The p wave may appear just before the QRS complex, and this makes it hard to distinguish the rhythm from sinus tachycardia.
Aberrant Conduction
It is not uncommon for there to be a wide QRS complex due to aberrant conduction due to underlying conduction system disease. This can make it difficult to distinguish AVNRT from VT. The distinguishing features include:
- AVNRT is associated with a QRS complex morphology resembles a typical bundle branch block
- AVNRT is not associated with AV dissociation where there is variable coupling of the p wave and the QRS complex
- AVNRT is associated with Cannon a waves
- AVNRT is not associated with capture beats or fusion beats
- AVNRT may convert with adenosine or vagal maneuvers
An electrophysiologic study may be needed to confirm AVNRT prior to ablation.
Holter Monitor / Event Recorder
If the patient complains of recurrent palpitations and no arrhythmia is present on the resting EKG, then a Holter Monitor or Cardiac Event Monitor should be considered.
Treatment
An episode of supraventricular tachycardia (SVT) due to AVNRT can be terminated by any action that transiently blocks the AV node. Various methods are possible.
Patient Position
Place the patient in a supine position to improve cerebral perfusion and reduce the odds of syncope. Placing the patient in Trendelenburg position may actually terminate the rhythm.
Vagal maneuvers
Some people with known AVNRT may be able to stop their attack by using various tricks to activate the vagus nerve. This includes carotid sinus massage (pressure on the carotid sinus in the neck), submersion of the face in ice water to trigger the diving reflex, putting the patient in Trendelenburg position or the Valsalva maneuver (increasing the pressure in the chest by attempting to exhale against a closed airway). Vagel maneuvers are contraindicated in the presence of hypotension.
Medication
Medical therapy can be initiated with AV nodal slowing drugs:
First Line Therapy
Adenosine
Beta blockers
Second Line Therapy
Numerous other antiarrhythmic drugs may be effective if the more commonly used medications have not worked; these include flecainide or amiodarone. Both adenosine and beta blockers may cause tightening of the airways, and are therefore used with caution in people who are known to have asthma. Calcium channel blockers should be avoided if there is a wide complex tacycardia and the diagnosis of AVNRT is not clearly established in so far as calcium channel blockers should be avoided in ventricular tachycardia. If the diagnosis of AVNRT is established, then non-dihydropyridine calcium channel blockers (such as verapamil) may be administered to terminate the rhythm is other agents are not effective.
Cardioversion
In very rare instances, cardioversion (the electrical restoration of a normal heart rhythm) is needed in the treatment of AVNRT. This would normally only happen if all other treatments have been ineffective, or if the fast heart rate is poorly tolerated (e.g. the development of heart failure symptoms, hypotension (low blood pressure) or unconsciousness).
Electrophysiology and Radiofrequency Ablation
After being diagnosed with AVNRT, patients can also undergo an electrophysiology (EP) study to confirm the diagnosis. Catheter ablation of the slow pathway, if successfully carried out, and cures 95% of patients with AVNRT. The risk of complications is quite low.
Prevention
Triggers such as alcohol and caffeine should be avoided.
References
- ↑ Laurent G, Leong-Poi H, Mangat I, Korley V, Pinter A, Hu X, So PP, Ramadeen A, Dorian P (2009). "Influence of ventriculoatrial timing on hemodynamics and symptoms during supraventricular tachycardia". Journal of Cardiovascular Electrophysiology. 20 (2): 176–81. doi:10.1111/j.1540-8167.2008.01276.x. PMID 18775049. Retrieved 2012-09-05. Unknown parameter
|month=ignored (help) - ↑ Gursoy S, Steurer G, Brugada J, et al. Brief report: the hemodynamic mechanism of pounding in the neck in atrioventricular nodal reentrant tachycardia. N Engl J Med. Sep 10 1992;327(11):772-4.
