Adenocarcinoma of the lung pathophysiology
|
Adenocarcinoma of the Lung Microchapters |
|
Differentiating Adenocarcinoma of the Lung from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Adenocarcinoma of the lung pathophysiology On the Web |
|
American Roentgen Ray Society Images of Adenocarcinoma of the lung pathophysiology |
|
Risk calculators and risk factors for Adenocarcinoma of the lung pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Shanshan Cen, M.D. [2] Sudarshana Datta, MD [3]
Overview
Adenocarcinoma is the most common type of lung cancer found in non-smokers and is usually seen as a peripheral lesion in the lungs. Individual susceptibility, active smoking, radon exposure, exposure to high pollution levels, asbestos exposure, occupational or environmental exposure to particular agents or carcinogens contribute to the development of adenocarcinoma of the lung. Hydrocarbons cause damage to the DNA and form DNA adducts. Benzo-A-pyrine has effects on inducing p53 mutations and affects molecular signaling pathways such as AKT. Genes involved in the pathogenesis of adenocarcinoma of the lung include EGFR, HER2, KRAS, ALK, and BRAF. On gross pathology, peripheral multifocal lesions are characteristic findings in patients with adenocarcinoma of the lung. On microscopic histopathological analysis, nuclear atypia, eccentrically placed nuclei, abundant cytoplasm, and conspicuous nucleoli are characteristic findings of adenocarcinoma of the lung.
Pathogenesis
- Adenocarcinoma is the most common type of lung cancer found in non-smokers and is usually seen as a peripheral lesion in the lungs, as compared to centrally located tumors such as small cell lung cancer and squamous cell lung cancer.[1][2]
- Individual susceptibility, active smoking, radon exposure, exposure to high pollution levels, asbestos exposure, occupational or environmental exposure to particular agents or carcinogens contribute to the development of adenocarcinoma of the lung. Hydrocarbons cause damage to the DNA and form DNA adducts. Benzo-A-pyrine has effects on inducing p53 mutations and affects molecular signaling pathways such as AKT.
- The “multiple hit theory” for adenocarcinoma of the lung states that genetic reproduction is hindered due to the cumulative effect of several toxic insults. Underlying lung disease such as COPD, idiopathic pulmonary fibrosis and tuberculosis may exacerbate also trigger the process.
- Mutations involving several oncogenes may lead to the development of adenocarcinoma of the lung. These are as follows:
- Mutations of ras (found in thirty percent of cases) affect signal transduction by affecting GTPase activity:
- c-myc
- c-raf
- Tumor suppressor genes retinoblastoma (Rb) and p53
- Mutations of APOBEC protein
Genetics
- Genes involved in the pathogenesis of adenocarcinoma of the lung include:[3][4][5][6]
- EGFR (7p11)
- KRAS (12p12)
- BRAF (7q34)
- PIK3CA (3q26)
- ERBB2 (17q12)
- Translocation EML4/ALK
- Tyrosine kinase fusions
- ALK (2p23), ROS1 (6q22), and RET (10q11)
Gross Pathology
- On gross pathology, peripheral multifocal lesions are characteristic findings in patients with adenocarcinoma of the lung.[7]
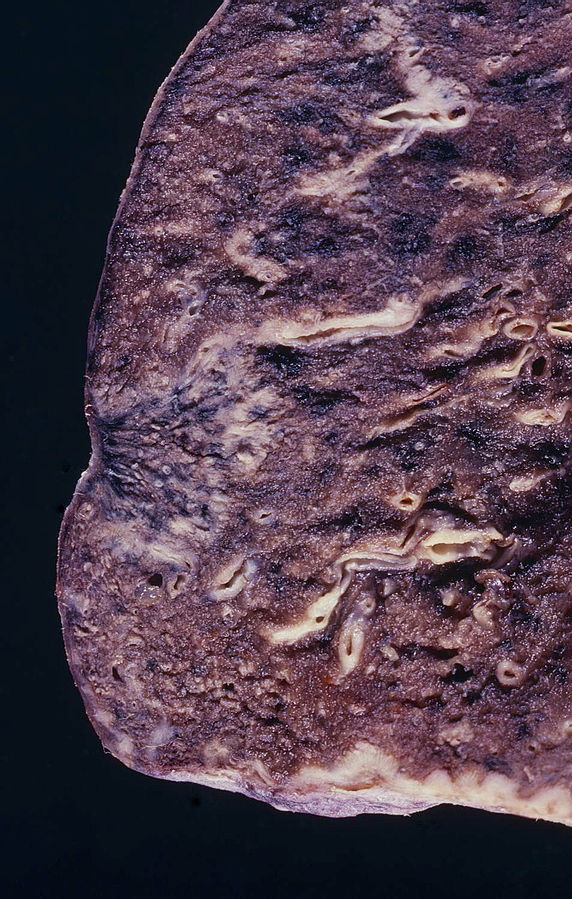
Source: Libre pathology
Microscopic Pathology
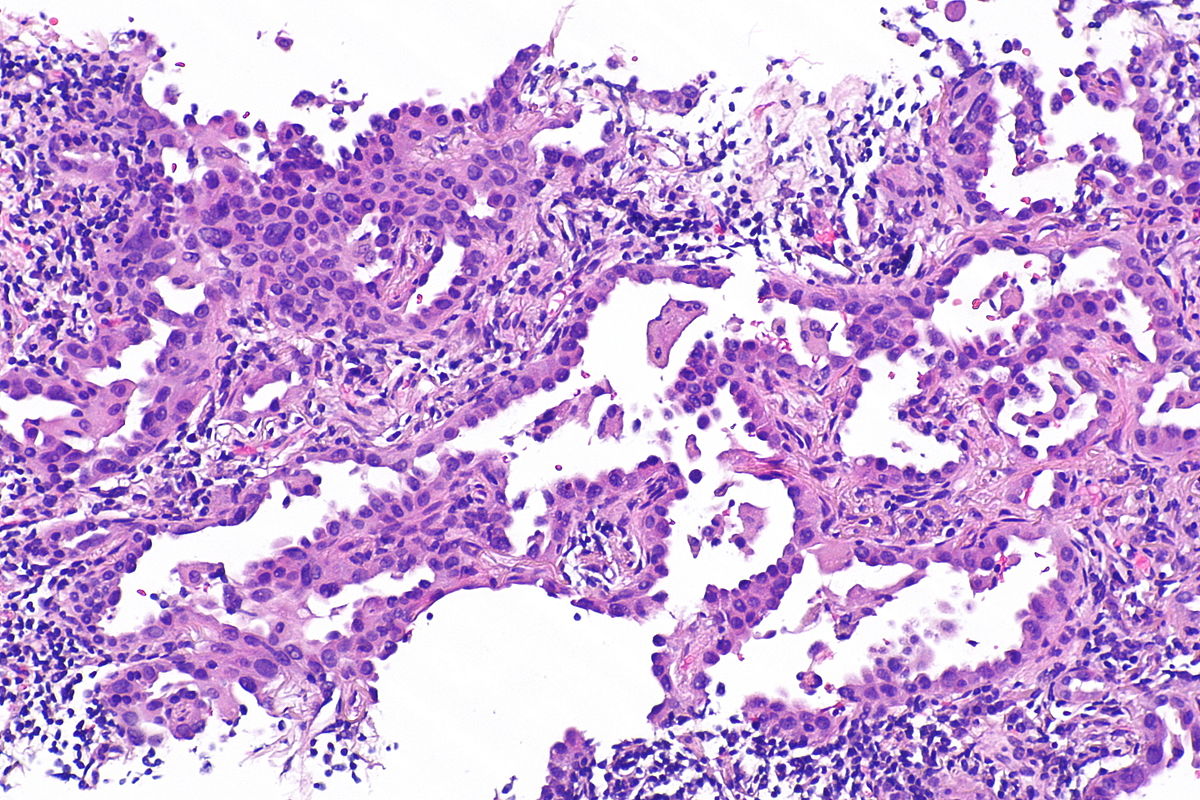
Source: Libre pathology
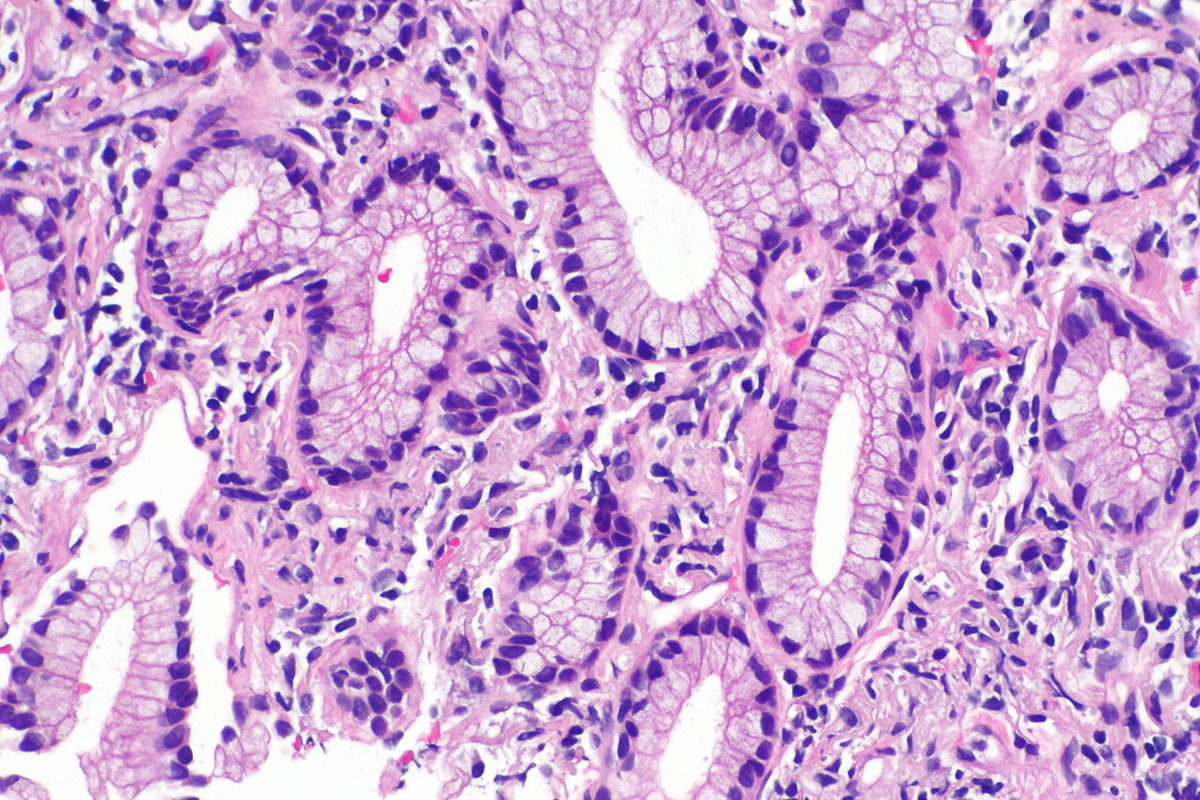
Source: Libre pathology
- On microscopic histopathological analysis, nuclear atypia, eccentrically placed nuclei, abundant cytoplasm, and conspicuous nucleoli are characteristic findings of adenocarcinoma of the lung.
- Atypical adenomatous hyperplasia (AAH): is the precursor of peripheral adenocarcinomas. It consists of well demarcated columnar or cuboidal cells with the following features:[8][9]
- Varying degrees of cytologic atypia
- Hyperchromasia
- Pleomorphism
- Prominent nucleoli
- As adenocarcinoma is a derivative of mucus producing glands in the lungs, it tends to stain mucin positive.
- Based on differentiation, the tumor may be:
- Well differentiated (low grade) : Normal appearance
- Poorly differentiated (high grade): Abnormal glandular appearance with a positive mucin stain
Histological Subtypes
- Histologically adenocarcinoma is divided in to following subtypes:[10][11]
- The IASLC/ATS/ERS lung adenocarcinoma histologic classification system was proposed in the Journal of Thoracic Oncology in 2011.[12]
- According to this new classification, tumor size ≤3 cm with pure lepidic pattern, but without lymphatic, vascular, pleural invasion or tumor necrosis was defined as adenocarcinoma in situ (AIS).
- If tumor size ≤3 cm with a lepidic predominant pattern and contained ≤5 mm stromal invasion it was defined as minimally invasive adenocarcinoma (MIA).
- If tumor had >5 mm stromal invasion it was defined as an invasive adenocarcinoma.
- Lepidic adenocarcinoma[13][14]
- Lepidic growth adenocarcinoma is defined as tumor cells proliferating along the surface of intact alveolar walls without stromal or vascular invasion pathologically.
- Solitary adenocarcinomas with pure lepidic growth, termed “AIS” has 100% disease-specific survival, if the lesion is completely resected.
- Acinar adenocarcinoma:[11][15]
- Acinar pattern comprises infiltrating round to oval glands lined by tumour cells.
- Irregular-shaped glands.
- Malignant cells: Hyperchromatic nuclei, fibroblastic stroma.
- Sometimes the glandular cells and lumina may contain mucin.
- Papillary adenocarcinoma[16]
- The papillary pattern is composed of glandular tumour cells growing along fibrovascular cores.
- Papillae, necrosis, surrounding invasion, cuboidal to columnar epithelial lining, mucinous or non-mucinous.
- Lung adenocarcinomas with papillary growth show 2 types of papillary architecture:
- True papillary type: Papillae containing a layered glandular epithelium surrounded by fibrovascular core.
- Micropapillary type: The papillary tufts lack a central fibrovascular core and extensively shed within alveolar spaces.
- Micropapillary growth has been associated with an aggressive clinical course compared with traditional papillary adenocarcinoma.
- Micropapillary adenocarcinoma (MPA) may be often diagnosed at a high stage in nonsmokers, with intralobar satellites.
- Micropapillary adenocarcinoma frequently metastasizes to the contralateral lung, mediastinal lymph nodes, bone, and adrenal glands, with high mortality.
- Micropapillary adenocarcinoma
- Solid adenocarcinoma
- Invasive mucinous adenocarcinoma
- Mixed invasive mucinous
- Nonmucinous adenocarcinoma
- Colloid adenocarcinoma
- Fetal adenocarcinoma
- Enteric adenocarcinoma
- Minimally invasive adenocarcinoma
- Nonmucinous
- Mucinous:
- Low grade differentiation
- Composed of: Tall columnar cells, basal nuclei and pale cytoplasm resembling goblet cells
- Varying amounts of cytoplasmic mucin and cytologic atypia
- Preinvasive lesions
- Atypical adenomatous hyperplasia
- Adenocarcinoma in situ
- Nonmucinous
- Mucinous
- Lepidic adenocarcinoma[13][14]
References
- ↑ Travis WD, Travis LB, Devesa SS (January 1995). "Lung cancer". Cancer. 75 (1 Suppl): 191–202. doi:10.1002/1097-0142(19950101)75:1+<191::AID-CNCR2820751307>3.0.CO;2-Y. PMID 8000996.
- ↑ Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson. "Chapter 13, box on morphology of adenocarcinoma". Robbins Basic Pathology (8th ed.). Philadelphia: Saunders. ISBN 1-4160-2973-7.
- ↑ Stewart, Bernard (2014). World cancer report 2014. Lyon, France Geneva, Switzerland: International Agency for Research on Cancer,Distributed by WHO Press, World Health Organization. ISBN 9283204298.
- ↑ Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S; et al. (2007). "Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer". Nature. 448 (7153): 561–6. doi:10.1038/nature05945. PMID 17625570.
- ↑ Davies KD, Le AT, Theodoro MF, Skokan MC, Aisner DL, Berge EM; et al. (2012). "Identifying and targeting ROS1 gene fusions in non-small cell lung cancer". Clin Cancer Res. 18 (17): 4570–9. doi:10.1158/1078-0432.CCR-12-0550. PMC 3703205. PMID 22919003.
- ↑ Stewart, Bernard (2014). World cancer report 2014. Lyon, France Geneva, Switzerland: International Agency for Research on Cancer,Distributed by WHO Press, World Health Organization. ISBN 9283204298.
- ↑ Adenocarcinoma of the lung. Librepathology 2015. http://librepathology.org/wiki/index.php/File:Adenocarcinoma_%283950819000%29.jpg
- ↑ Kumar, Vinay (2007). Robbins basic pathology. Philadelphia, PA: Saunders/Elsevier. ISBN 1416029737.
- ↑ Stewart, Bernard (2014). World cancer report 2014. Lyon, France Geneva, Switzerland: International Agency for Research on Cancer,Distributed by WHO Press, World Health Organization. ISBN 9283204298.
- ↑ Travis, William (2004). Pathology and genetics of tumours of the lung, pleura, thymus, and heart. Lyon: IARC Press. ISBN 9283224183.
- ↑ 11.0 11.1 "www.jto.org".
- ↑ . doi:10.3978/j.issn.2072-1439.2014.09.13. Missing or empty
|title=(help) - ↑ Iwata H (September 2016). "Adenocarcinoma containing lepidic growth". J Thorac Dis. 8 (9): E1050–E1052. doi:10.21037/jtd.2016.08.78. PMID 27747060.
- ↑ Jones KD (December 2013). "Whence lepidic?: the history of a Canadian neologism". Arch. Pathol. Lab. Med. 137 (12): 1822–4. doi:10.5858/arpa.2013-0144-HP. PMID 23937575.
- ↑ Lin, Gengpeng; Xie, Canmao (2017). "PUB070 Acinar-Predominant Pattern Correlates with Poorer Outcome in Invasive Mucinous Adenocarcinoma of the Lung". Journal of Thoracic Oncology. 12 (1): S1489. doi:10.1016/j.jtho.2016.11.2040. ISSN 1556-0864.
- ↑ De Oliveira Duarte Achcar, Rosane; Nikiforova, Marina N.; Yousem, Samuel A. (2009). "Micropapillary Lung Adenocarcinoma". American Journal of Clinical Pathology. 131 (5): 694–700. doi:10.1309/AJCPBS85VJEOBPDO. ISSN 0002-9173.