Cervical cancer screening
|
Cervical cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cervical cancer screening On the Web |
|
American Roentgen Ray Society Images of Cervical cancer screening |
|
Risk calculators and risk factors for Cervical cancer screening |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Assistant Editor-in-Chief: Monalisa Dmello, M.B,B.S., M.D. [2]
Overview
According to the American Cancer Society (ACS), American Society for Colposcopy and Cervical Pathology (ASCCP), and American Society for Clinical Pathology, screening for cervical cancer by pap smear is recommended for women 21-29 years of age every 3 years. For women ages 30-65 years screening can be done with cytology and HPV testing every 5 years or cytology alone every 3 years.
Screening
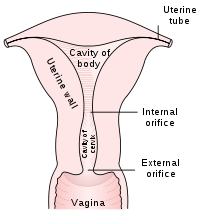
The Pap test aims to detect and prevent the progression of HPV-induced cervical cancer and other abnormalities in the female genital tract by sampling cells from the outer opening of the cervix of the uterus and the endocervix. It is generally recommended that sexually active females seek pap smear testing annually, although guidelines may vary from country to country. If results are abnormal, and depending on the nature of the abnormality, the test may need to be repeated in three to twelve months. If the abnormality requires closer scrutiny, the patient may be referred for detailed inspection of the cervix by colposcopy. The patient may also be referred for HPV DNA testing, which can serve as an adjunct (or even as an alternative) to Pap testing.[1]
About 5% to 7% of pap smears produce abnormal results, such as dysplasia, possibly indicating a pre-cancerous condition. Although many low grade cervical dysplasias spontaneously regress without ever leading to cervical cancer, dysplasia can serve as an indication that increased vigilance is needed. Endocervical and endometrial abnormalities can also be detected, as can a number of infectious processes, including yeast and trichomonas vaginalis. A small proportion of abnormalities are reported as of "uncertain significance
Liquid Based Monolayer Cytology
The techniques based around placing the sample into a vial containing a liquid medium which preserves the cells have been increasingly used. The media are primarily ethanol based. Two of the types are Sure-Path (TriPath Imaging) and Thin-Prep (Cytyc Corp). Once placed into the vial, the sample is processed at the laboratory into a cell thin-layer, stained, and examined by light microscopy. The liquid sample has the advantage of being suitable for low and high risk HPV testing and reduced unsatisfactory specimens from 4.1% to 2.6%.[2] Proper sample acquisition is crucial to the accuracy of the test; clearly, a cell that is not in the sample cannot be evaluated.
Studies of the accuracy of liquid based monolayer cytology report:
- Sensitivity 61%[3] to 66%[4]
- Specificity 82%[3] to 91%[4]
Some[2], but not all studies[4][3], report increased sensitivity from the liquid based smears.
Results
Screening Guidelines
| American Cancer Society (ACS), American Society for Colposcopy and Cervical Pathology (ASCCP), and American Society for Clinical Pathology | U.S. Preventive Services Task Force (USPSTF) | American College of Obstetricians and Gynecologists (ACOG) | ||
|---|---|---|---|---|
| When to start screening | Age 21. Women aged <21 years should not be screened regardless of the age of sexual initiation or other risk factors | Age 21. (A recommendation) Recommend against screening women aged <21 years (D recommendation) | Age 21 regardless of the age of onset of sexual activity. Women aged <21 years should not be screened regardless of age at sexual initiation and other behavior-related risk factors (Level A evidence) | |
| Statement about annual screening | Women of any age should not be screened annually by any screening method | Individuals and clinicians can use the annual Pap test screening visit as an opportunity to discuss other health problems and preventive measures. Individuals, clinicians, and health systems should seek effective ways to facilitate the receipt of recommended preventive services at intervals that are beneficial to the patient. Efforts also should be made to ensure that individuals are able to seek care for additional health concerns as they present | In women aged 30–65 years, annual cervical cancer screening should not be performed. (Level A evidence) Patients should be counseled that annual well-woman visits are recommended even if cervical cancer screening is not performed at each visit | |
| Screening method and intervals | ||||
| Cytology (conventional or liquid based) | 21–29 years | Every 3 years | Every 3 years (A recommendation) | Every 3 years (Level A evidence) |
| 30–65 years | Every 3 years | Every 3 years (A recommendation) | Every 3 years (Level A evidence) | |
| HPV co-test (cytology + HPV test administered together) | 21–29 years | HPV co-testing should not be used for women aged <30 years | Recommend against HPV co-testing in women aged <30 years (D recommendation) | HPV co-testing should not be performed in women aged <30 years. (Level A evidence ) |
| 30–65 years | Every 5 years; this is the preferred method. | For women who want to extend their screening interval, HPV co-testing every 5 years is an option (A recommendation) | Every 5 years; this is the preferred method (Level A evidence) | |
| Primary hrHPV f testing (as an alternative to cotesting or g cytology alone) | For women aged 30–65 years, screening by HPV testing alone is not recommended in most clinical settings | Recommend against screening for cervical cancer with HPV testing (alone or in combination with cytology) in women aged <30 years (D recommendation) | Not addressed | |
| When to stop screening | Aged >65 years with adequate negative prior screening* and no history of CIN2 or higher within the last 20 years | Aged >65 years with adequate screening history* and are not otherwise at high risk for cervical cancer (D recommendation) | Aged >65 years with adequate negative prior screening* results and no history of CIN 2 or higher (Level A evidence) | |
| When to screen after age 65 years | When to screen after age 65 years Aged >65 years with a history of CIN2 CIN2, CIN3, or adenocarcinoma in situ, routine screeningk should continue for at least 20 years | Women aged >65 years who have never been screened, do not meet the criteria for adequate prior screening, or for whom the adequacy of prior screening cannot be accurately accessed or documented.l Routine screeningk should continue for at least 20 years after spontaneous regression or appropriate management of a high-grade precancerous lesion, even if this extends screening past age 65 years. Certain considerations may support screening in women aged > 65 years who are otherwise considered high risk (such as women with a highgrade precancerous lesion or cervical cancer, women with in utero exposure to diethylstilbestrol, or women who are immunocompromised) | Women aged >65 years with a history of CIN2, CIN3, or AIS should continue routine agebased screeningk for at least 20 years (Level B evidence) | |
| Screening post-hysterectomy | Women who have had a total hysterectomy (removal of the uterus and cervix) should stop screening.Women who have had a supra-cervical hysterectomy (cervix intact) should continue screening according to guidelines | Recommend against screening in women who have had a hysterectomy (removal of the cervix) (D recommendation) | Women who have had a hysterectomy (removal of the cervix) should stop screening and not restart for any reason, (Level A evidence) | |
| The need for a bimanual pelvic exam | Not addressed in 2012 guidelines but was addressed in 2002 ACS guidelines | Addressed in USPSTF ovarian cancer screening recommendations (draft) | Addressed in 2012 well-woman visit recommendations.Aged <21 years, no evidence supports the routine internal examination of the healthy, asymptomatic patient. An “external-only” genital examination is acceptable. Aged ≥21 years, no evidence supports or refutes the annual pelvic examination or speculum and bimanual examination. The decision whether or not to perform a complete pelvic examination should be a shared decision after a discussion between the patient and her health care provider. Annual examination of the external genitalia should continue | |
| Screening among those immunized against HPV 16/18 | Women at any age with a history of HPV vaccination should be screened according to the age specific recommendations for the general population | The possibility that vaccination might reduce the need for screening with cytology alone or in combination with HPV testing is not established. Given these uncertainties, women who have been vaccinated should continue to be screened | Women who have received the HPV vaccine should be screened according to the same guidelines as women who have not been vaccinated (Level C evidence) | |
HPV = human papillomavirus; CIN = cervical intraepithelial neoplasia; AIS=adenocarcinoma in situ; hrHPV = high-risk HPV.
See also
References
- ↑ Safaeian, Mahboobeh; Solomon, Diane; Castle, Philip E. (2007). "Cervical Cancer Prevention—Cervical Screening: Science in Evolution". Obstetrics and Gynecology Clinics of North America. 34 (4): 739–760. doi:10.1016/j.ogc.2007.09.004. ISSN 0889-8545.
- ↑ 2.0 2.1 Ronco G, Cuzick J, Pierotti P; et al. (2007). "Accuracy of liquid based versus conventional cytology: overall results of new technologies for cervical cancer screening randomised controlled trial". doi:10.1136/bmj.39196.740995.BE. PMID 17517761.
- ↑ 3.0 3.1 3.2 Kulasingam SL, Hughes JP, Kiviat NB; et al. (2002). "Evaluation of human papillomavirus testing in primary screening for cervical abnormalities: comparison of sensitivity, specificity, and frequency of referral". JAMA. 288 (14): 1749–57. PMID 12365959.
- ↑ 4.0 4.1 4.2 Coste J, Cochand-Priollet B, de Cremoux P; et al. (2003). "Cross sectional study of conventional cervical smear, monolayer cytology, and human papillomavirus DNA testing for cervical cancer screening". BMJ. 326 (7392): 733. doi:10.1136/bmj.326.7392.733. PMID 12676841. ACP Journal Club