Primary mediastinal large B-cell lymphoma
For patient information, click Insert page name here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Badria Munir M.B.B.S.[2] Sowminya Arikapudi, M.B,B.S. [3]
Synonyms and keywords:: Mediastinal B-cell lymphoma; Mediastinal large B-cell lymphoma, PMBCL, Primary mediastinal B-cell lymphoma.
Overview
Primary mediastinal large B-cell lymphoma (PMBCL) is a subtype of diffuse large B-cell lymphoma (DLBCL). It is also considered a distinct type of non-Hodgkin lymphoma (NHL) in the World Health Organization (WHO) classification system. It occurs in the thymus gland. The small gland in the center of the chest behind the sternum where lymphocytes mature, multiply and become T cells. or lymph nodes in the center of the chest. On microscopic histopathological analysis, large-sized cells and alveolar fibrosis are characteristic findings of primary mediastinal large B-cell lymphoma. The incidence of primary mediastinal large B-cell lymphoma increases with age; the median age at diagnosis is 35 years. The symptoms of the primary mediastinal large B-cell lymphoma include fever, weight loss, night sweats, skin rash, facial swelling, cough, shortness of breath, and painless swelling in the neck, axilla, groin, thorax, or abdomen. Lymph node or mediastinal mass biopsy is diagnostic of primary mediastinal large B-cell lymphoma. The predominant therapy for primary mediastinal large B-cell lymphoma is chemotherapy. Adjunctive radiotherapy, stem cell transplant, and biological therapy may be required. The optimal therapy for primary mediastinal large B-cell lymphoma depends on the clinical presentation.
Classification
- Primary mediastinal B-cell lymphoma was recognized as a sub type of diffuse large B-cell lymphoma since the 1994 in Revised European American Lymphoma Classification.[1]
- It has been regarded as a unique clinical and biological entity since the 2001 according to World Health Organization classification.[2]
Pathophysiology
- Primary mediastinal large B-cell lymphoma most likely arises within the thymus.[3][4]
- Patients present with a localized anterosuperior mediastinal mass.
- The mass is often bulky and frequently invades adjacent structures such as lungs, pleura, or pericardium.
- Spreads to supraclavicular and cervical lymph nodes.
- Pathophysiologically, tumor grows through constitutive STAT 6 phosphorylation and DNA-binding activity.[5]
- STAT6 phosphorylation activates Interleukin 4/ interleukin-13 signalling pathway.
- Constitutive STAT6 phosphorylation and DNA-binding activity is detected is proved through immunohistochemical analysis.
- Another proposed mechanism of autocrine pathway is amplification of JAK 2 pathway which causes phosphorylation of IL-4 and IL-13 subsequently.
- The Janus kinase 2 (JAK2) is also constitutively phosphorylated in the primary mediastinal large B-cell lymphoma.
- Primary mediastinal large B-cell lymphoma is treated with JAK2 inhibitor AG490, resulted in partially decreased STAT6 phosphorylation, which suggests that JAK2 is partially involved in STAT6 activation in these cells.
Genetics:
- Genes involved in the pathogenesis of primary mediastinal large B-cell lymphoma include:
- Comparative genomic hybridzation demonstrated gains in chromosome 9p24 and 2p15
- Genomic hybridization in chromosome X-p11.4-21
- Translocations involving the CIITA gene[6]
- Amplification of the REL oncogene[7]
- Hyperdiploid karyotypes, often with gains in the region on chromosome 9p containing the JAK2 gene and the genes encoding PD-L1 and PD-L2, ligands for the receptor PD-1[8]
- The B cell leukemia/lymphoma 2 (BCL-2) gene and B cell leukemia 6 (BCL-6) gene rearrangements can occur.[9]
- Gains of the proto-oncogene BCL11A and nuclear accumulation of BCL11A(XL) protein.[10]
- Immunoglobulin genes clonally rearranged.
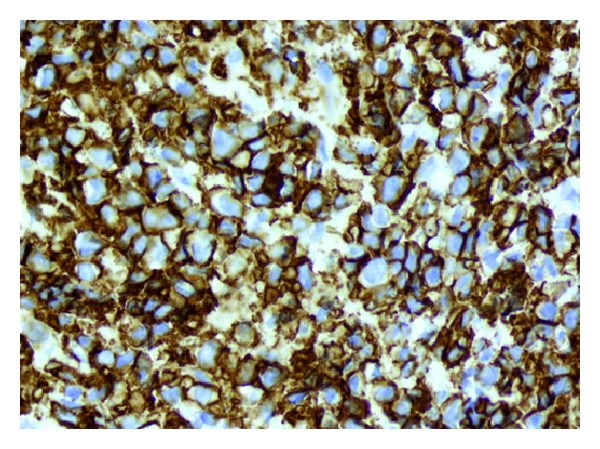
Immunophenotype:
- The immunophenotype of primary mediastinal large B-cell lymphoma is determined by histochemistry or flow cytometry.
- The tumor cells express B cell-associated antigens (CD19, CD20, CD22, CD79a) and CD45.[9]
- Weak expression of CD30 is often present.
- The tumor cells also stain for TRAF-1 and nuclear c-Rel. These two markers are also expressed by the Reed-Sternberg cells, but are not present in other forms of diffuse large B cell lymphoma. [11]
- Other markers that are relatively specific for primary mediastinal large B-cell lymphoma are CD200 and MAL.[12][13]
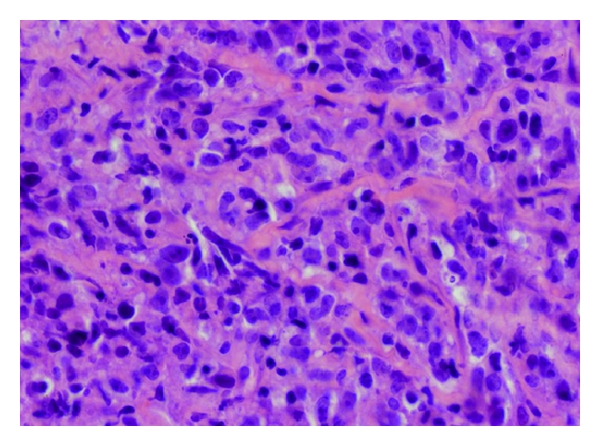
Microscopic Pathology:
- On microscopic histopathological analysis, large-sized cells and alveolar fibrosis are characteristic findings of primary mediastinal large B-cell lymphoma.
- The tumor is composed of large cells with variable nuclear features, cells may resemble:[14][15]
- Centroblasts
- Large centrocytes
- Multilobated cells, often with pale or "clear" cytoplasm
- Less frequently, the tumor cells resemble immunoblasts
- Reed-Sternberg-like cells
- Some cases have also presented with fine, compartmentalizing sclerosis.
-
Primary mediastinal large B-cell lymphoma pathology 2.jpg Primary mediastinal large B-cell lymphoma immunoreactivity for CD30[16]
Causes
- There are no established causes of primary mediastinal B-cell lymphoma.
Differentiating ((Page name)) from Other Diseases
- Primary mediastinal large B-cell lymphoma must be differentiated from other diseases such as:
Epidemiology and Demographics
- Primary mediastinal large B-cell lymphoma comprises of 7% of overall diffuse large B cell lymphoma's and 2.4 % of all Non hodgkin lymphomas. [17]
Age:
- The incidence of primary mediastinal large B-cell lymphoma increases with age; the median age at diagnosis is 35 years.[18]
Gender:
- Females are more commonly affected with primary mediastinal large B-cell lymphoma than males.[18]
Risk Factors
- There are no established risk factors for primary mediastinal large B-cell lymphoma.
Screening
- According to the the U.S. Preventive Service Task Force (USPSTF), there is insufficient evidence to recommend routine screening for primary mediastinal large B-cell lymphoma.[19]
Natural History, Complications, and Prognosis
- Primary mediastinal large B-cell lymphoma is usually a fast-growing lymphoma.
- Patients often have localized disease in the chest at first.
- If left untreated, primary mediastinal large B-cell lymphoma can cause:
- Primary mediastinal large B-cell lymphoma can also partially block the main vein (superior vena cava) that carries blood from the upper body to the heart and cause superior vena cava syndrome.
Common complications :
- Compression of vessels in the neck often causes following symptoms :
- Potential Oncologic emergencies are:
- Acute airway obstruction
- Pericardial tamponade
- Thrombosis of major neck or superior thoracic veins
- Patients with large mediastinal masses are at increased risk of respiratory or cardiac arrest during general anesthesia or heavy sedation.
- Patients who present with cardiorespiratory symptoms or radiographic evidence of tracheal obstruction are at greatest risk of perioperative respiratory morbidity.
Less common complication :
- Less common complication includes:
- Tumor lysis syndrome is caused by massive tumor cell lysis and the release of large amounts of potassium, phosphate, and uric acid into the systemic circulation.
- Deposition of uric acid and/or calcium phosphate crystals in the renal tubules results in acute renal failure.
- The bone marrow is rarely affected by this type of lymphoma.
- Recurrence or relapse often occurs in organs or tissues outside the lymph nodes (extranodal sites), such as the kidneys or central nervous system.
Prognosis:
- Prognosis is generally good after aggressive therapy, which usually combines chemotherapy with mediastinal irradiation. However if relapse occurs , it depends on paucity of molecular level of tumor cells, and their ability to evade immune system.
- Initial studies suggest that a more favorable course may be predicted by one of the following :
Diagnosis
Diagnostic Study of Choice
Biopsy:
- The diagnosis of primary mediastinal large B cell lymphoma relies on the exclusion of adequate tissue, which offers most difficulty due to the location of the tumor, therefore an excisional biopsy is usually not possible.
- Therefore, surgical biopsy is highly preferred.[21]
- Due to fibrosis, needle aspirates are often paucicellular and fail to provide information about the tissue.
- Small biopsies may be non-diagnostic because the lesion is not sampled adequately or because crush artifact or extensive necrosis, fibrosis, or cystic change obscures the diagnostic lesion.
- Similarly, core biopsies mostly contain fibrotic tissue or tumor cells that are disrupted and not useful.
- To obtain sufficient tissue for biopsy , patients usually undergo either one of the following techniques:[21]
Staging
- Staging for primary mediastinal large B-cell lymphoma is provided in the following table:[22]
| Stage | Involvement | Extranodal (E) status |
|---|---|---|
| Limited | ||
| Stage I | One node or a group of adjacent nodes | Single extranodal lesions without nodal involvement |
| Stage II | Two or more nodal groups on the same side of the diaphragm | Stage I or II by nodal extent with limited contiguous extranodal involvement |
| Stage II bulky | II as above with "bulky" disease | Not applicable |
| Advanced | ||
| Stage III | Nodes on both sides of the diaphragm; nodes above the diaphragm with spleen involvement | Not applicable |
| Stage IV | Additional noncontiguous extralymphatic involvement | Not applicable |
History and Symptoms
Symptoms of the primary mediastinal large B-cell lymphoma include:
- Fever
- Weight loss
- Night sweats
- Skin rash
- Shortness of breath
- Facial swelling
- Cough
- Painless swelling in the neck, axilla, groin, thorax, and abdomen
Physical Examination
Vitals
- Fever is often present
Skin
HEENT
- Cervical lymphadenopathy
- Facial edema
Thorax
- Thoracic masses suggestive of central lymphadenopathy
- Localized anterosuperior mediastinal mass
Abdomen
- Abdominal masses suggestive of central lymphadenopathy
Extremities
Laboratory Findings
Laboratory tests for primary mediastinal large B-cell lymphoma include:
- Complete blood count (CBC)
- Blood chemistry studies
- Liver function tests
- Serum LDH levels
- Beta 2 microglobulin levels
- Cytogenetic analysis
- Flow cytometry
- Immunohistochemistry
- Immunophenotyping
Electrocardiogram
- There are no ECG findings associated with primary mediastinal large B-cell lymphoma.
Chest X-Ray
- Chest X-ray may be helpful in the diagnosis of primary mediastinal large B-cell lymphoma. Finding on chest X-ray suggestive of primary mediastinal large B-cell lymphoma includes large anterior mediastinal mass.[16]
 |
Biopsy
- Lymph node or mediastinal mass biopsy is diagnostic of primary mediastinal large B-cell lymphoma.
Echocardiography
- Echocardiography may be helpful in the diagnosis of primary mediastinal large B-cell lymphoma.
CT
CT scan may be helpful in the diagnosis of primary mediastinal large B-cell lymphoma.
 |
MRI
MRI scan may be helpful in the diagnosis of primary mediastinal large B-cell lymphoma.
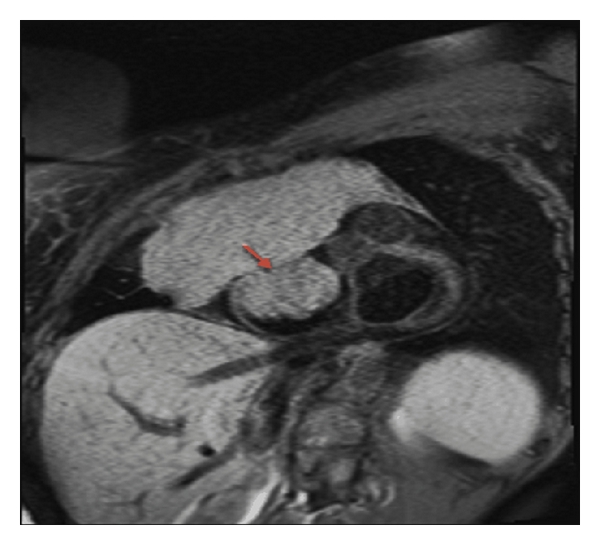 |
Other Imaging Findings
- PET scan may be helpful in the diagnosis of primary mediastinal large B-cell lymphoma.
- In contrast to CT imaging, FDG-PET is a functional imaging tool that can distinguish between viable tumor and necrosis or fibrosis in a residual mass.[23]
Other diagnostic studies
- Monoclonal anti-MAL antibody is now commercially used in order to identify primary mediastinal large B-cell lymphoma. It provides good sensitivity and high specificity for diagnosis of primary mediastinal large B-cell lymphoma. [24]
Treatment
Medical Therapy
| Therapy | Description |
|---|---|
| Chemotherapy |
|
| Biological therapy |
|
| Radiation therapy |
|
| Stem cell transplant |
|
- The choice of initial treatment depends on stage of disease at the time of presentation. Following are different treatment regimens that are recommended for various stages:
Induction Chemotherapy:
- R-CHOP chemotherapy which includes rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone is preferred regimen for limited disease but it is not suggested alone, follow up with radiotherapy is highly recommended to prevent relapse of disease.
- Dose adjusted da-EPOCH-Retoposide, doxorubicin, cyclophosphamide, vincristine, prednisone, and rituximab.
- This is best for the patients who wish to avoid radiotherapy, such as young patients (<30 yrs) or women who have concerns with irradiation of breast tissue.
- However investigators from Europe have suggested that MACOP-B(methotrexate with leucovorin rescue, doxorubicin, cyclophosphamide, vincristine, prednisone, and bleomycin) may be superior to CHOP in the management of primary mdiastinal large B-cell lymphoma.
Radiotherapy:
- Radiotherapy is usually indicated to prevent relapse and recurrence of disease after chemotherapy induction especially after following R-CHOP regimen.[20]
- In aggressive disease, radiation therapy has been proven to be beneficial in patients with good-prognosis stage I and nonbulky stage II disease.[25]
High-Dose Chemotherapy and Autologous Stem Cell Transplantation:
- The use of high-dose chemotherapy and autologous stem cell transplantation in patients with aggressive disease proves to be beneficial in some cases.[26]
Relapsed disease:
- Patients with relapsed disease often have systemic involvement and many also have extranodal diseas, in the parenchymal organs, including kidneys, liver, and CNS.[27]
- These patients are recommended to undergo salvage systemic chemotherapy followed by stem cell transplantation.[28]
Salvage therapy:
- rituximab, ifosfamide, carboplatin, and etoposide (RICE) serves as a salvage approach.
- Patients who demonstrate improvement on PET scan are recommended for transplantation.
- Patients who have refractory disease should be offered clinical trials, although some can be considered for allogeneic bone marrow transplantation.
Surgery
- Surgical intervention is not recommended for the management of primary mediastinal large B-cell lymphoma.
Primary Prevention
- There are no established measures for the primary prevention of primary mediastinal large B-cell lymphoma.
Secondary Prevention
- There are no established measures for the secondary prevention of primary mediastinal large B-cell lymphoma.
References
- ↑ Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, Delsol G, De Wolf-Peeters C, Falini B, Gatter KC (September 1994). "A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group". Blood. 84 (5): 1361–92. PMID 8068936.
- ↑ Liu PP, Wang KF, Xia Y, Bi XW, Sun P, Wang Y, Li ZM, Jiang WQ (July 2016). "Racial patterns of patients with primary mediastinal large B-cell lymphoma: SEER analysis". Medicine (Baltimore). 95 (27): e4054. doi:10.1097/MD.0000000000004054. PMC 5058818. PMID 27399089.
- ↑ Primary mediastinal large B-cell lymphoma. Surveillance, Epidemiology, and End Results Program. http://seer.cancer.gov/seertools/hemelymph/51f6cf56e3e27c3994bd5318/. Accessed on March 7, 2016
- ↑ Addis BJ, Isaacson PG (April 1986). "Large cell lymphoma of the mediastinum: a B-cell tumour of probable thymic origin". Histopathology. 10 (4): 379–90. PMID 2423430.
- ↑ Guiter C, Dusanter-Fourt I, Copie-Bergman C, Boulland ML, Le Gouvello S, Gaulard P, Leroy K, Castellano F (July 2004). "Constitutive STAT6 activation in primary mediastinal large B-cell lymphoma". Blood. 104 (2): 543–9. doi:10.1182/blood-2003-10-3545. PMID 15044251.
- ↑ Steidl C, Shah SP, Woolcock BW, Rui L, Kawahara M, Farinha P, Johnson NA, Zhao Y, Telenius A, Neriah SB, McPherson A, Meissner B, Okoye UC, Diepstra A, van den Berg A, Sun M, Leung G, Jones SJ, Connors JM, Huntsman DG, Savage KJ, Rimsza LM, Horsman DE, Staudt LM, Steidl U, Marra MA, Gascoyne RD (March 2011). "MHC class II transactivator CIITA is a recurrent gene fusion partner in lymphoid cancers". Nature. 471 (7338): 377–81. doi:10.1038/nature09754. PMC 3902849. PMID 21368758.
- ↑ Joos S, Otaño-Joos MI, Ziegler S, Brüderlein S, du Manoir S, Bentz M, Möller P, Lichter P (February 1996). "Primary mediastinal (thymic) B-cell lymphoma is characterized by gains of chromosomal material including 9p and amplification of the REL gene". Blood. 87 (4): 1571–8. PMID 8608249.
- ↑ Twa DD, Chan FC, Ben-Neriah S, Woolcock BW, Mottok A, Tan KL, Slack GW, Gunawardana J, Lim RS, McPherson AW, Kridel R, Telenius A, Scott DW, Savage KJ, Shah SP, Gascoyne RD, Steidl C (March 2014). "Genomic rearrangements involving programmed death ligands are recurrent in primary mediastinal large B-cell lymphoma". Blood. 123 (13): 2062–5. doi:10.1182/blood-2013-10-535443. PMID 24497532.
- ↑ 9.0 9.1 Lamarre L, Jacobson JO, Aisenberg AC, Harris NL (September 1989). "Primary large cell lymphoma of the mediastinum. A histologic and immunophenotypic study of 29 cases". Am. J. Surg. Pathol. 13 (9): 730–9. PMID 2788371.
- ↑ Weniger MA, Pulford K, Gesk S, Ehrlich S, Banham AH, Lyne L, Martin-Subero JI, Siebert R, Dyer MJ, Möller P, Barth TF (October 2006). "Gains of the proto-oncogene BCL11A and nuclear accumulation of BCL11A(XL) protein are frequent in primary mediastinal B-cell lymphoma". Leukemia. 20 (10): 1880–2. doi:10.1038/sj.leu.2404324. PMID 16871282.
- ↑ Rodig SJ, Savage KJ, Nguyen V, Pinkus GS, Shipp MA, Aster JC, Kutok JL (February 2005). "TRAF1 expression and c-Rel activation are useful adjuncts in distinguishing classical Hodgkin lymphoma from a subset of morphologically or immunophenotypically similar lymphomas". Am. J. Surg. Pathol. 29 (2): 196–203. PMID 15644776.
- ↑ Dorfman DM, Shahsafaei A, Alonso MA (December 2012). "Utility of CD200 immunostaining in the diagnosis of primary mediastinal large B cell lymphoma: comparison with MAL, CD23, and other markers". Mod. Pathol. 25 (12): 1637–43. doi:10.1038/modpathol.2012.129. PMID 22899296.
- ↑ Copie-Bergman C, Plonquet A, Alonso MA, Boulland ML, Marquet J, Divine M, Möller P, Leroy K, Gaulard P (November 2002). "MAL expression in lymphoid cells: further evidence for MAL as a distinct molecular marker of primary mediastinal large B-cell lymphomas". Mod. Pathol. 15 (11): 1172–80. doi:10.1097/01.MP.0000032534.81894.B3. PMID 12429796.
- ↑ De Paepe P, Achten R, Verhoef G, Wlodarska I, Stul M, Vanhentenrijk V, Praet M, De Wolf-Peeters C (October 2005). "Large cleaved and immunoblastic lymphoma may represent two distinct clinicopathologic entities within the group of diffuse large B-cell lymphomas". J. Clin. Oncol. 23 (28): 7060–8. doi:10.1200/JCO.2005.15.503. PMID 16129841.
- ↑ 15.0 15.1 Primary mediastinal large B-cell lymphoma. Canadian Cancer Society. http://www.cancer.ca/en/cancer-information/cancer-type/non-hodgkin-lymphoma/non-hodgkin-lymphoma/types-of-nhl/primary-mediastinal-large-b-cell-lymphoma/?region=nb. Accessed on March 7, 2016
- ↑ 16.0 16.1 Primary mediastinal large B-cell lymphoma.Hindawi Publishing Corporation. http://www.hindawi.com/journals/crihem/2012/197347/. Accessed on March 07, 2016
- ↑ "A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project". Blood. 89 (11): 3909–18. June 1997. PMID 9166827.
- ↑ 18.0 18.1 Nguyen LN, Ha CS, Hess M, Romaguera JE, Manning JT, Cabanillas F, Cox JD (July 2000). "The outcome of combined-modality treatments for stage I and II primary large B-cell lymphoma of the mediastinum". Int. J. Radiat. Oncol. Biol. Phys. 47 (5): 1281–5. PMID 10889382.
- ↑ Recommendations. U.S Preventive Services Task Force. http://www.uspreventiveservicestaskforce.org/BrowseRec/Search?s=Primary+mediastinal+large+B-cell+lymphoma+. Accessed on March 7, 2016
- ↑ 20.0 20.1 Martelli M, Ceriani L, Zucca E, Zinzani PL, Ferreri AJ, Vitolo U, Stelitano C, Brusamolino E, Cabras MG, Rigacci L, Balzarotti M, Salvi F, Montoto S, Lopez-Guillermo A, Finolezzi E, Pileri SA, Davies A, Cavalli F, Giovanella L, Johnson PW (June 2014). "[18F]fluorodeoxyglucose positron emission tomography predicts survival after chemoimmunotherapy for primary mediastinal large B-cell lymphoma: results of the International Extranodal Lymphoma Study Group IELSG-26 Study". J. Clin. Oncol. 32 (17): 1769–75. doi:10.1200/JCO.2013.51.7524. PMID 24799481.
- ↑ 21.0 21.1 Sun W, Song K, Zervos M, Pass H, Cangiarella J, Bizekis C, Crawford B, Wang BY (May 2010). "The diagnostic value of endobronchial ultrasound-guided needle biopsy in lung cancer and mediastinal adenopathy". Diagn. Cytopathol. 38 (5): 337–42. doi:10.1002/dc.21195. PMID 19890836.
- ↑ Cheson, Bruce D.; Fisher, Richard I.; Barrington, Sally F.; Cavalli, Franco; Schwartz, Lawrence H.; Zucca, Emanuele; Lister, T. Andrew; Alliance, Australasian Leukaemia and Lymphoma Group; Eastern Cooperative Oncology Group; European Mantle Cell Lymphoma Consortium; Italian Lymphoma Foundation; European Organisation for Research; Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study Group; German Hodgkin's Study Group; Japanese Lymphorra Study Group; Lymphoma Study Association; NCIC Clinical Trials Group; Nordic Lymphoma Study Group; Southwest Oncology Group; United Kingdom National Cancer Research Institute (2014-09-20). "Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification". Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 32 (27): 3059–3068. doi:10.1200/JCO.2013.54.8800. ISSN 1527-7755. PMID 25113753.
- ↑ Nagle SJ, Chong EA, Chekol S, Shah NN, Nasta SD, Glatstein E, Plastaras JP, Torigian DA, Schuster SJ, Svoboda J (January 2015). "The role of FDG-PET imaging as a prognostic marker of outcome in primary mediastinal B-cell lymphoma". Cancer Med. 4 (1): 7–15. doi:10.1002/cam4.322. PMC 4312112. PMID 25205600.
- ↑ Traverse-Glehen A, Pittaluga S, Gaulard P, Sorbara L, Alonso MA, Raffeld M, Jaffe ES (November 2005). "Mediastinal gray zone lymphoma: the missing link between classic Hodgkin's lymphoma and mediastinal large B-cell lymphoma". Am. J. Surg. Pathol. 29 (11): 1411–21. PMID 16224207.
- ↑ Miller TP, Dahlberg S, Cassady JR, Adelstein DJ, Spier CM, Grogan TM, LeBlanc M, Carlin S, Chase E, Fisher RI (July 1998). "Chemotherapy alone compared with chemotherapy plus radiotherapy for localized intermediate- and high-grade non-Hodgkin's lymphoma". N. Engl. J. Med. 339 (1): 21–6. doi:10.1056/NEJM199807023390104. PMID 9647875.
- ↑ Haioun C, Lepage E, Gisselbrecht C, Bastion Y, Coiffier B, Brice P, Bosly A, Dupriez B, Nouvel C, Tilly H, Lederlin P, Biron P, Brière J, Gaulard P, Reyes F (March 1997). "Benefit of autologous bone marrow transplantation over sequential chemotherapy in poor-risk aggressive non-Hodgkin's lymphoma: updated results of the prospective study LNH87-2. Groupe d'Etude des Lymphomes de l'Adulte". J. Clin. Oncol. 15 (3): 1131–7. doi:10.1200/JCO.1997.15.3.1131. PMID 9060555.
- ↑ Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-López A, Hagenbeek A, Cabanillas F, Klippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (April 1999). "Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group". J. Clin. Oncol. 17 (4): 1244. doi:10.1200/JCO.1999.17.4.1244. PMID 10561185.
- ↑ Popat U, Przepiork D, Champlin R, Pugh W, Amin K, Mehra R, Rodriguez J, Giralt S, Romaguera J, Rodriguez A, Preti A, Andersson B, Khouri I, Claxton D, de Lima M, Donato M, Anderlini P, Gajewski J, Cabanillas F, van Besien K (January 1998). "High-dose chemotherapy for relapsed and refractory diffuse large B-cell lymphoma: mediastinal localization predicts for a favorable outcome". J. Clin. Oncol. 16 (1): 63–9. doi:10.1200/JCO.1998.16.1.63. PMID 9440724.
![Primary mediastinal large B-cell lymphoma immunoreactivity for CD30[16]](/images/5/58/Primary_mediastinal_large_B-cell_lymphoma_pathology_2.jpg)