Tick-borne encephalitis primary prevention
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ilan Dock, B.S.
|
Tick-borne encephalitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tick-borne encephalitis primary prevention On the Web |
|
American Roentgen Ray Society Images of Tick-borne encephalitis primary prevention |
|
Risk calculators and risk factors for Tick-borne encephalitis primary prevention |
Overview
Tick- borne encephalitis prevention strategies are based on avoiding potential, infected tick bites. Avoiding tick bites may be accomplished through limiting exposure to endemic areas. However if it is impossible or impractical to avoid these areas, several preventative strategies may be implemented. These strategies are indicated under the Prevention title below. Other prevention strategies include a proper removal of the tick. This process is also outlined below under the title, the best way to remove a tick.
Prevention
Limiting tick exposure

It is unreasonable to assume that a person can completely eliminate activities that may result in tick exposure. Therefore, prevention measures should emphasize personal protection when exposed to natural areas where ticks are present:
- Wear light-colored clothing which allows you to see ticks that are crawling on your clothing.
- Tuck your pants legs into your socks so that ticks cannot crawl up the inside of your pants legs.
- Apply repellents to discourage tick attachment. Repellents containing permethrin can be sprayed on boots and clothing, and will last for several days. Repellents containing DEET (n, n-diethyl-m-toluamide) can be applied to the skin, but will last only a few hours before reapplication is necessary. Use DEET with caution on children. Application of large amounts of DEET on children has been associated with adverse reactions.
- Conduct a body check upon return from potentially tick-infested areas by searching your entire body for ticks. Use a hand-held or full-length mirror to view all parts of your body. Remove any tick you find on your body.
- Parents should check their children for ticks, especially in the hair, when returning from potentially tick-infested areas.
- Ticks may also be carried into the household on clothing and pets and only attach later, so both should be examined carefully to exclude ticks.[1]
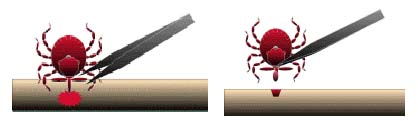
The best way to remove a tick
- Use fine-tipped tweezers or notched tick extractor, and protect your fingers with a tissue, paper towel, or latex gloves. Persons should avoid removing ticks with bare hands.
- Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure. Do not twist or jerk the tick; this may cause the mouth-parts to break off and remain in the skin. (If this happens, remove mouth-parts with tweezers. Consult your health care provider if illness occurs.)
- After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water.
- Do not squeeze, crush, or puncture the body of the tick because its fluids may contain infectious organisms. Skin accidentally exposed to tick fluids can be disinfected with iodine scrub, rubbing alcohol, or water containing detergents.

- Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. [2]
Vaccination
- TBE vaccinations are not available in the United States.
- There are two inactivated, cell-culture derived vaccinations, FSME-IMMUN and Encepur, available in both Europe and in Canada.
- Two vaccines, TBE-Moscow and EnceVir exist in Russia.
- Vaccines from Russia and Europe provide cross-protection against the all three viral subtypes; Siberian, Far east, European.
- Vaccines provide above 95% efficacy; failure is noted in individuals above the age of 50.
- Vaccination process requires approximately six months for completion.
- It is recommended that travelers to endemic areas prioritize avoiding tick bites, more so than relying on the protection of a vaccination.[3]

References
- ↑ General Tick Disease Information. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/symptoms.html Accessed on December 30, 2015
- ↑ Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015
- ↑ 3.0 3.1 TBEV Vaccination. Centers for Disease Control and Prevention. http://wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/tickborne-encephalitis Accessed February 11,2016.