Melanoma surgery
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Melanoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Melanoma surgery On the Web |
|
American Roentgen Ray Society Images of Melanoma surgery |
Overview
Surgery
Surgical Margins for Wide Excision of Primary Melanoma
- The National Comprehensive Cancer Network (NCCN) recommends wide excision of margins of primary tumors based on tumor thickness.
- The margins may be individualized to accomodate anatomic and functional considerations.
| Tumor thickness | Recommended Clinical Margins |
| In situ | 0.5 cm |
| ≤ 1 mm | 1 cm |
| > 1 mm - 2 mm | 1-2 cm |
| > 2 mm - 4 mm | 2 cm |
| > 4 mm | 2 cm |

Diagnostic punch or excisional biopsies may appear to excise (and in some cases may indeed actually remove) the tumor, but further surgery is often necessary to reduce the risk of recurrence.
Complete surgical excision with adequate margins and assessment for the presence of detectable metastatic disease along with short and long term follow up is standard. Often this is done by a "wide local excision" (WLE) with 1 to 2 cm margins. The wide excision aims to reduce the rate of tumour recurrence at the site of the original lesion. This is a common pattern of treatment failure in melanoma. Considerable research has aimed to elucidate appropriate margins for excision with a general trend toward less aggressive treatment during the last decades. There seems to be no advantage to taking in excess of 2 cm margins for even the thickest tumors.[1]
Mohs micrographic surgery is not well accepted in the treatment of melanoma. In this surgery, performed by specially-trained dermatologists, a small layer of tissue is excised and prepared as a frozen tissue section. This section can be prepared and examined by the dermatologist/dermatopathologist within one hour, and the patient will return for further stages of excision as needed, with each excised tissue layer being examined until clear margins are obtained.[2] However, the usefulness of Moh's surgery in melanoma is limited because of the difficulty of identifying melanocytic atypia on a frozen section, which may lead to incomplete resection of the melanoma.[2][3]
Other issues to consider with Moh's technique are risks of tumor implantation and possible false negative margins due to suboptimal melanocytic staining.[4] Deviation from recommended 1-2 cm margins of excision should thus be approached carefully.
Melanomas which spread usually do so to the lymph nodes in the region of the tumour before spreading elsewhere. Attempts to improve survival by removing lymph nodes surgically (lymphadenectomy) were associated with many complications but unfortunately no overall survival benefit. Recently the technique of sentinel lymph node biopsy has been developed to reduce the complications of lymph node surgery while allowing assessment of the involvement of nodes with tumour.
Although controversial and without prolonging survival, "sentinel lymph node" biopsy is often performed, especially for T1b/T2+ tumors, mucosal tumors, ocular melanoma and tumors of the limbs. A process called lymphoscintigraphy is performed in which a radioactive tracer is injected at the tumor site in order to localize the "sentinel node(s)". Further precision is provided using a blue tracer dye and surgery is performed to biopsy the node(s). Routine H&E staining, and immunoperoxidase staining will be adequate to rule out node involvement. PCR (Polymerase Chain Reaction) tests on nodes, usually performed to test for entry into clinical trials, now demonstrate that many patients with a negative SLN actually had a small number of positive cells in their nodes. Alternatively, a fine-needle aspiration may be performed, and is often used to test masses.
If a lymph node is positive, depending on the extent of lymph node spread, a radical lymph node dissection will often be performed. If the disease is completely resected the patient will be considered for adjuvant therapy.
Minor surgery
Moles that are irregular in color or shape are suspicious of a malignant or a premalignant melanoma. Following a visual examination and a dermatoscopic exam (an instrument that illuminates a mole, revealing its underlying pigment and vascular network structure), the doctor may biopsy the suspicious mole. If it is malignant, the mole and an area around it needs excision. This will require a referral to a surgeon or dermatologist.
The diagnosis of melanoma requires experience, as early stages may look identical to harmless moles or not have any color at all. Where any doubt exists, the patient will be referred to a specialist dermatologist. Beyond this expert knowledge a biopsy performed under local anesthesia is often required to assist in making or confirming the diagnosis and in defining the severity of the melanoma.
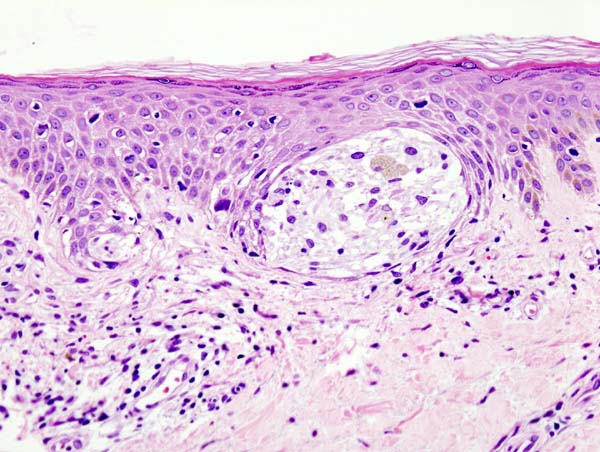
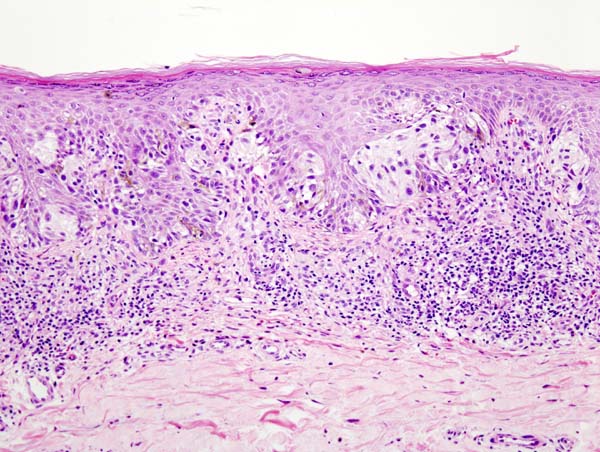
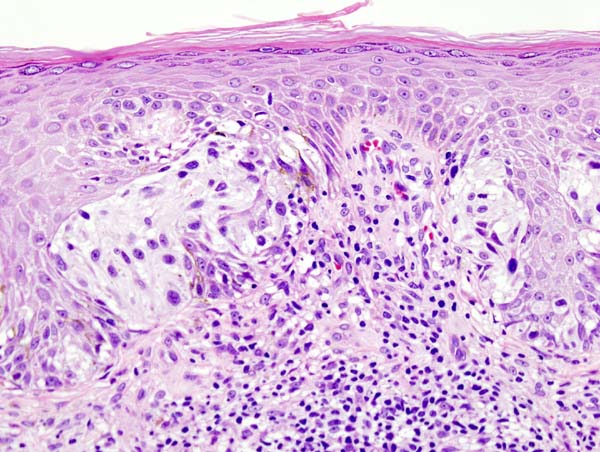
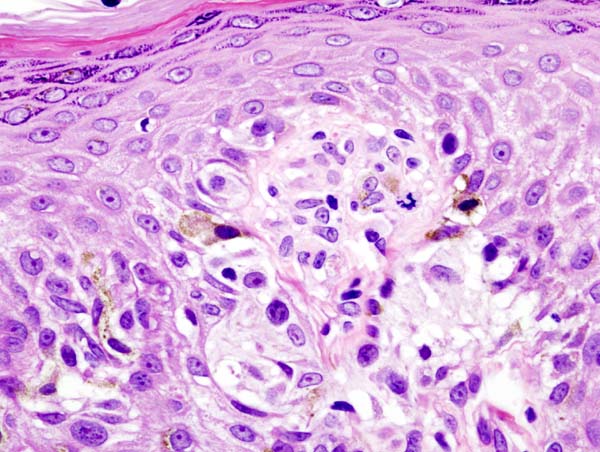
Excisional biopsy is the management of choice; this is where the suspect lesion is totally removed with an adequate ellipse of surrounding skin and tissue.[5] The biopsy will include the epidermal, dermal, and subcutaneous layers of the skin, enabling the histopathologist to determine the depth of penetration of the melanoma by microscopic examination. This is described by Clark's level (involvement of skin structures) and Breslow's depth (measured in millimeters).
If an excisional biopsy is not possible in certain larger pigmented lesions, a punch biopsy may be performed by a specialist hospital doctor, using a surgical punch (an instrument similar to a tiny cookie cutter with a handle, with an opening ranging in size from 1 to 6 mm). The punch is used to remove a plug of skin (down to the subcutaneous layer) from a portion of a large suspicious lesion, for histopathological examination.
References
- ↑ Balch C, Urist M, Karakousis C, Smith T, Temple W, Drzewiecki K, Jewell W, Bartolucci A, Mihm M, Barnhill R (1993). "Efficacy of 2-cm surgical margins for intermediate-thickness melanomas (1 to 4 mm). Results of a multi-institutional randomized surgical trial". Ann Surg. 218 (3): 262–7, discussion 267-9. PMID 8373269.
- ↑ 2.0 2.1 Bowen G, White G, Gerwels J (2005). "Mohs micrographic surgery". Am Fam Physician. 72 (5): 845–8. PMID 16156344.Full text
- ↑ Nahabedian M (2005). "Melanoma". Clin Plast Surg. 32 (2): 249–59. PMID 15814121.
- ↑ Nahabedian MY (2005). "Melanoma". Clin Plastic Surg. 32: 249–259.
- ↑ Swanson N, Lee K, Gorman A, Lee H (2002). "Biopsy techniques. Diagnosis of melanoma". Dermatol Clin. 20 (4): 677–80. PMID 12380054.