Primary amoebic meningoencephalitis laboratory findings: Difference between revisions
Hardik Patel (talk | contribs) No edit summary |
Hardik Patel (talk | contribs) (/* Direct Visualization{{cite journal| author=Visvesvara GS| title=Amebic meningoencephalitides and keratitis: challenges in diagnosis and treatment. | journal=Curr Opin Infect Dis | year= 2010 | volume= 23 | issue= 6 | pages= 590-4 | pmid=2080233...) |
||
| Line 19: | Line 19: | ||
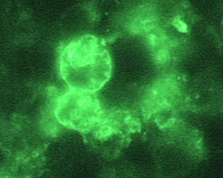
[[Image:NfowleriHEbraintissue.jpg|thumb|150|Indirect Immunofluorescence (IIF) assay for ''[[Naegleria fowleri]]'', 1000x oil magnification]] | [[Image:NfowleriHEbraintissue.jpg|thumb|150|Indirect Immunofluorescence (IIF) assay for ''[[Naegleria fowleri]]'', 1000x oil magnification]] | ||
|} | |} | ||
Copyleft images obtained courtesy of http://www.cdc.gov/parasites/naegleria/diagnosis-hcp.html | |||
===Immunohistochemistry (IHC)<ref name="pmid20802332">{{cite journal| author=Visvesvara GS| title=Amebic meningoencephalitides and keratitis: challenges in diagnosis and treatment. | journal=Curr Opin Infect Dis | year= 2010 | volume= 23 | issue= 6 | pages= 590-4 | pmid=20802332 | doi=10.1097/QCO.0b013e32833ed78b | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20802332 }} </ref><ref name="pmid19657454">{{cite journal| author=da Rocha-Azevedo B, Tanowitz HB, Marciano-Cabral F| title=Diagnosis of infections caused by pathogenic free-living amoebae. | journal=Interdiscip Perspect Infect Dis | year= 2009 | volume= 2009 | issue= | pages= 251406 | pmid=19657454 | doi=10.1155/2009/251406 | pmc=PMC2719787 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19657454 }} </ref>=== | ===Immunohistochemistry (IHC)<ref name="pmid20802332">{{cite journal| author=Visvesvara GS| title=Amebic meningoencephalitides and keratitis: challenges in diagnosis and treatment. | journal=Curr Opin Infect Dis | year= 2010 | volume= 23 | issue= 6 | pages= 590-4 | pmid=20802332 | doi=10.1097/QCO.0b013e32833ed78b | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20802332 }} </ref><ref name="pmid19657454">{{cite journal| author=da Rocha-Azevedo B, Tanowitz HB, Marciano-Cabral F| title=Diagnosis of infections caused by pathogenic free-living amoebae. | journal=Interdiscip Perspect Infect Dis | year= 2009 | volume= 2009 | issue= | pages= 251406 | pmid=19657454 | doi=10.1155/2009/251406 | pmc=PMC2719787 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19657454 }} </ref>=== | ||
Revision as of 20:00, 27 December 2012
|
Primary amoebic meningoencephalitis Microchapters |
|
Differentiating Primary Amoebic Meningoencephalitis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Primary amoebic meningoencephalitis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Primary amoebic meningoencephalitis laboratory findings |
|
FDA on Primary amoebic meningoencephalitis laboratory findings |
|
CDC on Primary amoebic meningoencephalitis laboratory findings |
|
Primary amoebic meningoencephalitis laboratory findings in the news |
|
Blogs on Primary amoebic meningoencephalitis laboratory findings |
|
Directions to Hospitals Treating Primary amoebic meningoencephalitis |
|
Risk calculators and risk factors for Primary amoebic meningoencephalitis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hardik Patel, M.D.
Please help WikiDoc by adding more content here. It's easy! Click here to learn about editing.
Overview
Primary amoebic meningoencephalitis is diagnosed using specific laboratory tests available in only a few laboratories in the United States. Because of the rarity of the infection and difficulty in initial detection, about 75% of diagnoses are made after the death of the patient. It can be diagnosed in the laboratory by detecting Naegleria fowleri organisms, nucleic acid, or antigen in cerebrospinal fluid (CSF), biopsy, or tissue specimens.
Laboratory Findings
CSF Analysis
Cerebrospinal fluid (CSF) studies of patients infected with Naegleria fowleri typically demonstrate a pattern similar to bacterial meningitis with an elevated opening pressure, a polymorphonuclear pleocytosis, normal or low glucose, and elevated protein. However the observations of blood in the CSF and/or motile amoeba are clues to a potential diagnosis of PAM.
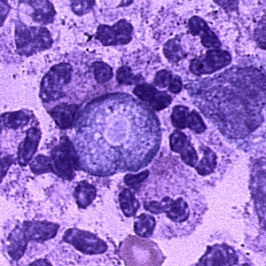
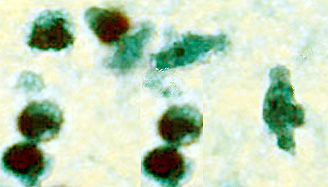
Direct Visualization[1][2]
The motile Naegleria fowleri can often be seen moving rapidly under a microscope when looking at a fresh sample of CSF. The amebae can also be stained with a variety of stains, such as Giemsa-Wright or a modified trichrome stain, for identification.
 |
 |
 |
Copyleft images obtained courtesy of http://www.cdc.gov/parasites/naegleria/diagnosis-hcp.html
Immunohistochemistry (IHC)[1][2]
A specific antibody to Naegleria fowleri can be used in conjunction with another antibody that deposits a chemical or glows under specific types of light (indirect fluorescent antibody [IFA]) to directly stain the amebae in tissue.
Polymerase Chain Reaction (PCR)[3][4][5]
Specific molecular tools can amplify DNA from the amebae in CSF or tissue to specifically identify if the amebae are present. Looking at strains or subtypes of Naegleria fowleri can be done, but little is known about the natural populations in the environment, which makes it difficult to interpret what the findings mean.
Amoeba Culture
The sample is added to a growth plate covered in bacteria that can serve as a food source for Naegleria fowleri. Incubating at higher temperatures selects for Naegleria fowleri growth, which can be seen as tracks made by the ameba as it moves across the plate eating the bacteria. Growing Naegleria fowleri in mammalian cell culture and looking for toxic cell effects is also possible.
Environmental Detection
Water samples can be collected, concentrated, and put into culture to grow and select for Naegleria fowleri. Samples can be tested using the serologic or molecular methods described above.
References
- ↑ 1.0 1.1 Visvesvara GS (2010). "Amebic meningoencephalitides and keratitis: challenges in diagnosis and treatment". Curr Opin Infect Dis. 23 (6): 590–4. doi:10.1097/QCO.0b013e32833ed78b. PMID 20802332.
- ↑ 2.0 2.1 da Rocha-Azevedo B, Tanowitz HB, Marciano-Cabral F (2009). "Diagnosis of infections caused by pathogenic free-living amoebae". Interdiscip Perspect Infect Dis. 2009: 251406. doi:10.1155/2009/251406. PMC 2719787. PMID 19657454.
- ↑ Qvarnstrom Y, Visvesvara GS, Sriram R, da Silva AJ (2006). "Multiplex real-time PCR assay for simultaneous detection of Acanthamoeba spp., Balamuthia mandrillaris, and Naegleria fowleri". J Clin Microbiol. 44 (10): 3589–95. doi:10.1128/JCM.00875-06. PMC 1594764. PMID 17021087.
- ↑ Robinson BS, Monis PT, Dobson PJ (2006). "Rapid, sensitive, and discriminating identification of Naegleria spp. by real-time PCR and melting-curve analysis". Appl Environ Microbiol. 72 (9): 5857–63. doi:10.1128/AEM.00113-06. PMC 1563602. PMID 16957204.
- ↑ Luan F, Xu X, Cordeiro MN, Liu H, Zhang X (2012). "QSAR modeling for the antimalarial activity of 1, 4-naphthoquinonyl derivatives as potential antimalarial agents". Curr Comput Aided Drug Des. PMID 23157413.