Peripheral arterial disease pathophysiology: Difference between revisions
No edit summary |
|||
| Line 37: | Line 37: | ||
===Associated Disorders=== | ===Associated Disorders=== | ||
Many PVD patients also have [[angina pectoris]] or have had [[myocardial infarction]]. There is also an increased risk for [[stroke]]. | Many PVD patients also have [[angina pectoris]] or have had [[myocardial infarction]]. There is also an increased risk for [[stroke]]. | ||
==References== | ==References== | ||
Revision as of 23:57, 30 October 2012
|
Peripheral arterial disease Microchapters |
|
Differentiating Peripheral arterial disease from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
AHA/ACC Guidelines on Management of Lower Extremity PAD |
|
Guidelines for Structured Exercise Therapy for Lower Extremity PAD |
|
Guidelines for Minimizing Tissue Loss in Lower Extremity PAD |
|
Guidelines for Revascularization of Claudication in Lower Extremity PAD |
|
Guidelines for Management of Acute Limb Ischemial in Lower Extremity PAD |
|
Guidelines for Longitudinal Follow-up for Lower Extremity PAD |
|
Peripheral arterial disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Peripheral arterial disease pathophysiology |
|
Directions to Hospitals Treating Peripheral arterial disease |
|
Risk calculators and risk factors for Peripheral arterial disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
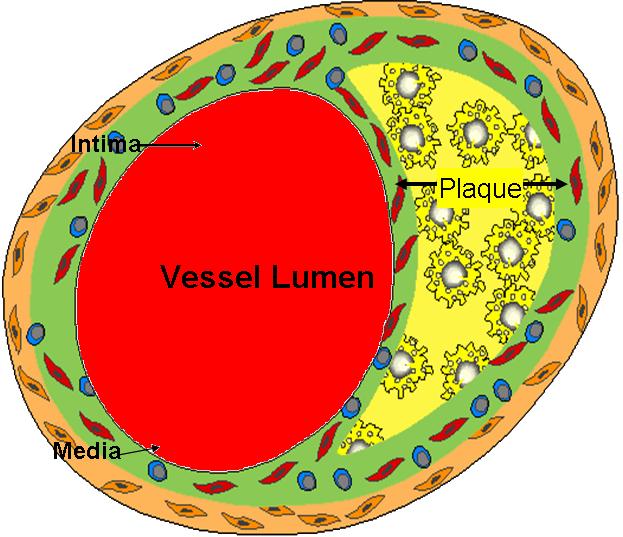
Pathophysiology
- PAD is a manifestation of systemic atherosclerosis that has developed over many years.
- Atherosclerosis is a complex process that involves endothelial dysfunction, lipid disturbances, platelet activation, thrombosis, oxidative stress, vascular smooth muscle activation, altered matrix metabolism, remodeling and genetic factors
- Atherosclerosis frequently develops at arterial bifurcations and branches where endogenous atheroprotective mechanisms are impaired as a result of the effects of disturbed flow on endothelial cells
- The stages of atherosclerosis are divided into the following:
- Lesion initiation
- Results from endothelial dysfunction
- Formation of the fatty streak
- Results from an inflammatory lesion that develops first
- Affects the intima of the artery and leads to formation of the foam cell
- Fatty streak consists primarily of smooth muscle cells, monocytes, macrophages, and T and B cells
- Fibroproliferative atheroma development
- Originates from the fatty streak
- Contains larger numbers of smooth muscle cells frlled with lipids
- Advanced lesion development
- Results from continued accumulation of cells that make up the fatty streak and fibroproliferative atheroma
- Highly cellular
- Contains intrinsic vascular cell walls (both endothelial and smooth muscle), and inflammatory cells (monocytes, macrophages, and T lymphocytes)
- Also contains a lipid core covered by a fibrous cap
- Lesion initiation
- Arteries initially compensate for atherosclerosis by remodeling, which causes the blood vessels to increase in size
- Advanced lesions eventually intrude into the lumen, resultsing in flow-limiting stenoses and chronic ischemic syndromes
- Acute arterial events occur if the fibrous cap is disrupted, the resulting exposure of the "prothrombotic" necrotic lipid core and subendothelial tissue leads to thrombus formation and flow occlusion
- In addition to coronary artery disease and cerebrovascular disease, PAD is one of the three major syndromes of atherothrombosis
- Atherothrombosis is the term currently used to describe the process of thrombus formation on top of a ruptured plaque located at a disease arterial segment
- Such atherosclerotic plaques tend to occur at vessel bifurcations, presumed to be due to both impaired atheroprotective mechanisms and disturbed blood flow leading to local intimal injury
- Panvascular disease refers to clinically significant atherosclerosis is present in multiple vascular beds
Associated Disorders
Many PVD patients also have angina pectoris or have had myocardial infarction. There is also an increased risk for stroke.