Peripheral arterial disease classification
|
Peripheral arterial disease Microchapters |
|
Differentiating Peripheral arterial disease from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
AHA/ACC Guidelines on Management of Lower Extremity PAD |
|
Guidelines for Structured Exercise Therapy for Lower Extremity PAD |
|
Guidelines for Minimizing Tissue Loss in Lower Extremity PAD |
|
Guidelines for Revascularization of Claudication in Lower Extremity PAD |
|
Guidelines for Management of Acute Limb Ischemial in Lower Extremity PAD |
|
Guidelines for Longitudinal Follow-up for Lower Extremity PAD |
|
Peripheral arterial disease classification On the Web |
|
American Roentgen Ray Society Images of Peripheral arterial disease classification |
|
Directions to Hospitals Treating Peripheral arterial disease |
|
Risk calculators and risk factors for Peripheral arterial disease classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2], Rim Halaby
Overview
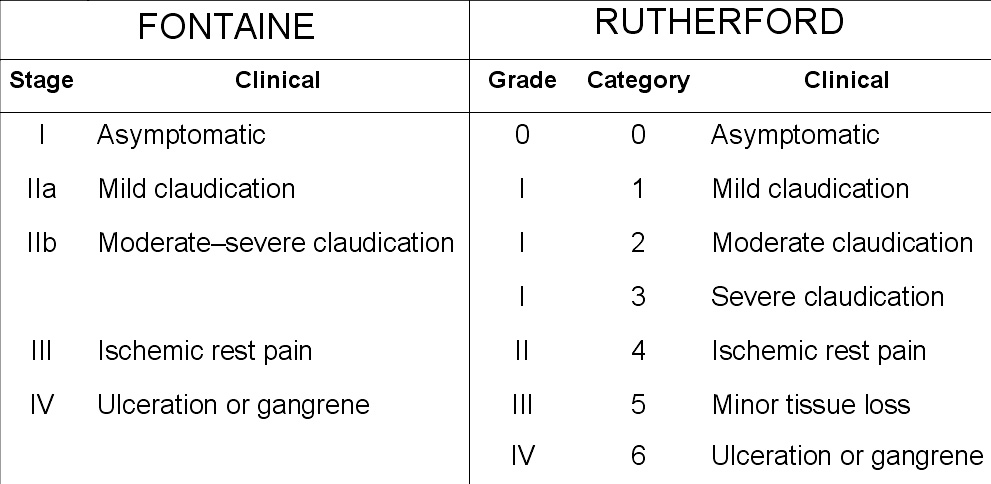
Peripheral arterial disease is commonly divided in the Fontaine stages, introduced by Dr. René Fontaine in 1954. There's another classification created by Rutherford consisting of three grades and six categories. In addition, the American College of Cardiology/American Heart Assocommon iliac arterytion (ACC/AHA) uses a symptoms-based classification (absence of symptoms, claudication, critical limb ischemia and acute limb ischemia) in their guidelines. TASC (Trans Atlantic Inter-Society Consensus) morphological consensus is used to guide the choice between endovascular and surgical revarscularization in the management of patients with peripheral artery disease.
Classification
Fontaine Stages
- Stage I: Asymptomatic
- Stage II a: Claudication after walking a distance that exceeds 200 meters
- Stage II b: Claudication after walking a distance inferior to 200 meters
- Stage III: Ischemia rest pain
- Stage IV: Ulceration or tissue loss (gangrene)[1]
Rutherford Categories
- Grade 0, Category 0: Asymptomatic
- Grade I, Category 1: Mild claudication
- Grade I, Category 2: Moderate claudication
- Grade I, Category 3: Severe claudication
- Grade II, Category 4: Ischaemia rest pain
- Grade III, Category 5: Minor tissue loss
- Grade IV, Category 6: Major tissue loss[2]
Shown below is an image showing the difference between Fontaine's and Rutherford's classification:
Classification Used in American College of Cardiology/American Heart Assocommon Iliac Arterytion (ACC/AHA) Practice Guidelines
- Absence of symptoms
- Claudication
- Critical/chronic limb ischaemia
- Acute limb ischaemia
TASC Morphological Stratification
- TASC (Trans Atlantic Inter-Society Consensus) morphological consensus is used to guide the choice between endovascular and surgical revarscularization in the management of the patients with peripheral artery disease.
Morphological Stratification of Iliac Lesions
- TASC type A iliac lesions:
- Single stenosis less than 3 cm of the common iliac artery or external iliac artery (unilateral/bilateral)
- TASC type B iliac lesions:
- Single stenosis 3 to 10 cm in length, not extending into the common femoral artery, or
- Total of 2 stenoses less than 5 cm long in the common iliac artery and/or external iliac artery and not extending into the common femoral artery, or
- Unilateral common iliac artery occlusion
- TASC type C iliac lesions:
- Bilateral 5- to 10-cm-long stenosis of the common iliac artery and/or external iliac artery, not extending into the common femoral artery, or
- Unilateral external iliac artery occlusion not extending into the common femoral artery, or
- Unilateral external iliac artery stenosis extending into the common femoral artery, or
- Bilateral common iliac artery occlusion
- TASC type D iliac lesions:
- Diffuse, multiple unilateral stenoses involving the common iliac artery, external iliac artery, and common femoral artery (usually more than 10 cm long), or
- Unilateral occlusion involving both the common iliac artery and external iliac artery, or
- Bilateral external iliac artery occlusions, or
- Diffuse disease involving the aorta and both iliac arteries, or
- Iliac stenoses in a patient with an abdominal aortic aneurysm orother lesion requiring aortic or iliac surgery[3]
Morphological Stratification of Femoropopliteal Lesions
- TASC type A femoropopliteal lesions:
- Single stenosis less than 3 cm of the superficial femoral artery or popliteal artery
- TASC type B femoropopliteal lesions:
- Single stenosis 3 to 10 cm in length, not involving the distal popliteal artery, or
- Heavily calcified stenoses up to 3 cm in length, or
- Multiple lesions, each less than 3 cm (stenoses or occlusions), or
- Single or multiple lesions in the absence of continuous tibial runoff to improve inflow for distal surgical bypass
- TASC type C femoropopliteal lesions:
- Single stenosis or occlusion longer than 5 cm, or
- Multiple stenoses or occlusions, each 3 to 5 cm in length, with or without heavy calcification
- TASC type D femoropopliteal lesions:
- Complete common femoral artery or superficial femoral artery occlusions or complete popliteal and proximal trifurcation occlusions[3]
References
- ↑ Fontaine R, Kim M, Kieny R (1954). "Die chirugische Behandlung der peripheren Durchblutungsstörungen. (Surgical treatment of peripheral circulation disorders)". Helvetica Chirurgica Acta (in German). 21 (5/6): 499&ndash, 533. PMID 14366554.
- ↑ Christopher W. Advances in interventional cardiology. Circulation November 6, 2007 vol. 116 no. 19 2203-2215
- ↑ 3.0 3.1 Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, White CJ, White J, White RA, Antman EM, Smith SC, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B (2006). "ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation". Circulation. 113 (11): e463–654. doi:10.1161/CIRCULATIONAHA.106.174526. PMID 16549646. Retrieved 2012-10-09. Unknown parameter
|month=ignored (help)