Peripheral arterial disease history and symptoms
|
Peripheral arterial disease Microchapters |
|
Differentiating Peripheral arterial disease from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
AHA/ACC Guidelines on Management of Lower Extremity PAD |
|
Guidelines for Structured Exercise Therapy for Lower Extremity PAD |
|
Guidelines for Minimizing Tissue Loss in Lower Extremity PAD |
|
Guidelines for Revascularization of Claudication in Lower Extremity PAD |
|
Guidelines for Management of Acute Limb Ischemial in Lower Extremity PAD |
|
Guidelines for Longitudinal Follow-up for Lower Extremity PAD |
|
Peripheral arterial disease history and symptoms On the Web |
|
American Roentgen Ray Society Images of Peripheral arterial disease history and symptoms |
|
Peripheral arterial disease history and symptoms in the news |
|
Directions to Hospitals Treating Peripheral arterial disease |
|
Risk calculators and risk factors for Peripheral arterial disease history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Vishnu Vardhan Serla M.B.B.S. [3]; Rim Halaby
Overview
Patients with peripheral arterial disease can be asymptomatic in 70% of cases, can have symptoms of intermittent claudication or can sometimes have critical symptoms that include ulceration and gangrene. The hallmark of peripheral arterial disease is the symptom of claudication which is an intermittent cramping pain in the leg that is induced by exercise and relieved by rest. The clinical presentation of peripheral arterial disease depends on the location and severity of stenosis of the vessel; in fact, calf cramping in the upper 2/3 of the calf is usually due to superficial femoral disease, while cramping in the lower 1/3 of the calf is due to popliteal disease. Buttock, thigh, calf or foot claudication, can occur either singly or in combination. The most frequently affected artery in intermittent claudication is the popliteal artery. Leg pain occurs in one leg in 40% of patients and in both legs in 60% of patients. Patients may also experience fatigue or pain in the thighs and buttocks.
History
An accurate history is the key to the diagnosis of PAD. The history must include information about:
- Any exertional limitation of the lower extremity muscles or any history of walking impairment (fatigue, numbness, aching, or pain).
- Detailed description of the pain: location, onset, progression, relieving and aggravating factors.
- Any pain at rest localized at the lower leg or foot and its association with the upright or recumbent positions.
- Atherosclerotic risk factors: The atherosclerotic risk factors may help to identify patients, who although asymptomatic, have evidence of PAD on physical examination or noninvasive testing.
- Any poorly healing or non healing ulcers of the legs or feet.
- Postprandial abdominal pain that reproducibly is provoked by eating and is associated with weight loss.
- Family history of a first-degree relative with abdominal aortic aneurysm.
Symptoms
- No symptoms or atypical symptoms (70% of cases)
Intermittent Claudication
- Onset: Always after walking or exercise
- Character: Cramping
- Site: Unilateral or bilateral
- Walking distance for the symptoms to start: Almost constant
- Relief: Rest and standing without movement
Chronic Limb Ischemia
- Rest pain
- Ulceration
- Gangrene
Acute Limb Ischemia
- Pain
- Pallor
- Paraesthesias
- Paralysis
- Pulselessness
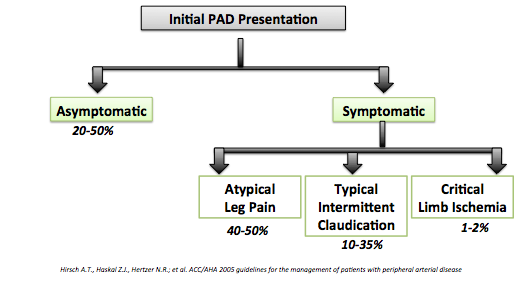
Shown below is an image that summarizes the initial presentation of peripheral arterial disease:
Shown below is an image depicting the location of symptoms depending on the nature of involved arteries:

Other Symptoms of Advanced PAD
- Calf muscles that shrink (wither)
- Hair loss over the toes and feet
- Thick toenails
- Shiny, tight skin
- Painful non-bleeding ulcers on the feet or toes (usually black) that are slow to heal
Leriche's Syndrome
Leriche's syndrome, an aortoiliac occlusive disease, is an atherosclerotic occlusive disease involving the abdominal aorta and/or both of the iliac arteries.
The classical triad of symptoms of Leriche's syndrome:
- Claudication of the buttocks and thighs
- Absent or decreased femoral pulses
- Impotence
In addition, any number of symptoms may present, depending on the distribution and severity of the disease, such as muscle atrophy and slow wound healing in the legs.
Management of Patients With Peripheral Artery Disease (Compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations) : A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines[1]
Vascular History and Physical Examination (DO NOT EDIT)[1]
| Class I |
| "1. Individuals at risk for lower extremity PAD should undergo a vascular review of symptoms to assess walking impairment, claudication, ischemic rest pain, and/or the presence of nonhealing wounds. (Level of Evidence: C)" |
| "2. Individuals at risk for lower extremity PAD should undergo comprehensive pulse examination and inspection of the feet. (Level of Evidence: C)" |
| "3. Individuals over 50 years of age should be asked if they have a family history of a first-order relative with an abdominal aortic aneurysm. (Level of Evidence: C)" |
Clinical Presentation (Asymptomatic)(DO NOT EDIT)[1]
| Class I |
| "1.A history of walking impairment, claudication, ischemic rest pain, and/or nonhealing wounds is recommended as a required component of a standard review of symptoms for adults 50 years and older who have atherosclerosis risk factors and for adults 70 years and older. (Level of Evidence: C)" |
| "2.Individuals with asymptomatic lower extremity PAD should be identified by examination and/or measurement of the ankle-brachial index (ABI) so that therapeutic interventions known to diminish their increased risk of myocardial infarction (MI), stroke, and death may be offered. (Level of Evidence: B)" |
| "3.Smoking cessation, lipid lowering, and diabetes and hypertension treatment according to current national treatment guidelines are recommended for individuals with asymptomatic lower extremity PAD. (Level of Evidence: B)" |
| "4.Antiplatelet therapy is indicated for individuals with asymptomatic lower extremity PAD to reduce the risk of adverse cardiovascular ischemic events. (Level of Evidence: C)" |
| Class IIa |
| "1.An exercise ABI measurement can be useful to diagnose lower extremity PAD in individuals who are at risk for lower extremity PAD who have a normal ABI (0.91 to 1.30), are without classic claudication symptoms, and have no other clinical evidence of atherosclerosis. (Level of Evidence: C)" |
| "2.A toe-brachial index or pulse volume recording measurement can be useful to diagnose lower extremity PAD in individuals who are at risk for lower extremity PAD who have an ABI greater than 1.30 and no other clinical evidence of atherosclerosis(Level of Evidence: C)" |
| Class IIb |
| "1.Angiotensin-converting enzyme (ACE) inhibition may be considered for individuals with asymptomatic lower extremity PAD for cardiovascular risk reduction.(Level of Evidence: C)" |
Claudication in PAD Patients (DO NOT EDIT)[2]
| Class I |
| "1. Patients with symptoms of intermittent claudication should undergo a vascular physical examination, including measurement of the ABI. (Level of Evidence: B)" |
| "2. In patients with symptoms of intermittent claudication, the ABI should be measured after exercise if the resting index is normal. (Level of Evidence: B)" |
| "3. Patients with intermittent claudication should have significant functional impairment with a reasonable likelihood of symptomatic improvement and absence of other disease that would comparably limit exercise even if the claudication was improved (e.g., angina, heart failure, chronic respiratory disease, or orthopedic limitations) before undergoing an evaluation for revascularization. (Level of Evidence: C)" |
| "4. Individuals with intermittent claudication who are offered the option of endovascular or surgical therapies should:(a) be provided information regarding supervised claudication exercise therapy and pharmacotherapy;(b) receive comprehensive risk factor modification and antiplatelet therapy;(c) have a significant disability, either being unable to perform normal work or having serious impairment of other activities important to the patient; and (d) have lower extremity PAD lesion anatomy such that the revascularization procedure would have low risk and a high probability of initial and long-term success. (Level of Evidence: C)" |
| Class III |
| "1. Arterial imaging is not indicated for patients with a normal postexercise ABI. This does not apply if other atherosclerotic causes (e.g., entrapment syndromes or isolated internal iliac artery occlusive disease) are suspected. (Level of Evidence: C)" |
References
- ↑ 1.0 1.1 1.2 Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss L; et al. (2013). "Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". J Am Coll Cardiol. 61 (14): 1555–70. doi:10.1016/j.jacc.2013.01.004. PMC 4492473. PMID 23473760.
- ↑ Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, Hiratzka LF, Murphy WR, Olin JW, Puschett JB, Rosenfield KA, Sacks D, Stanley JC, Taylor LM, White CJ, White J, White RA, Antman EM, Smith SC, Adams CD, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B (2006). "ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation". Circulation. 113 (11): e463–654. doi:10.1161/CIRCULATIONAHA.106.174526. PMID 16549646. Retrieved 2012-10-09. Unknown parameter
|month=ignored (help)