Paroxysmal AV block other diagnostic studies: Difference between revisions
Homa Najafi (talk | contribs) No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}}{{Akash}} | {{CMG}}; {{AE}}{{Akash}} | ||
==Overview== | ==Overview== | ||
An [[Implantable Cardiac Monitor]] is almost exclusively used in the [[diagnosis]] of [[bradycardia]] related disorders such as high-grade [[atrioventricular block]], [[sinus node dysfunction]] and [[neurocardiogenic syncope]] (with predominant cardio-inhibitory component). This prolonged monitoring (up to 3 years) can help correlate [[bradycardia]] conduction disorders with symptoms. An [[EPS]] is an invasive [[catheter]] based procedure that is employed to detect and [[anatomically]] locate conduction disorders. An increased [[HH interval]] is seen in [[intrinsic paroxysmal AV Block]]. Certain maneuvers cause an increase in [[vagal]] surge and may precipitate symptoms in extrinsic vagal paroxysmal AV block. These include [[carotid sinus massage]] and [[tilt table testing]]. | |||
==Implantable Loop Recorder== | |||
*[[Implantable loop recorders]] are useful tools as they help correlate electrical tracings with the patients [[symptoms]] during an [[acute]] event. | |||
**By giving an inkling of the [[etiology]] of the [[syncope]], it helps guide [[therapy]] strategies, such as adopting permanent stimulation devices in patients with [[paroxysmal AV block]].<ref name="pmid28496928">{{cite journal| author=Guerrero-Márquez FJ, Arana-Rueda E, Pedrote A| title=Idiopathic Paroxysmal Atrio-Ventricular Block. What is The Mechanism? | journal=J Atr Fibrillation | year= 2016 | volume= 9 | issue= 3 | pages= 1449 | pmid=28496928 | doi=10.4022/jafib.1449 | pmc=5368548 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28496928 }} </ref> | |||
* According to the '''European Society of Cardiology''', the indication for [[implantable loop recorders]] are as follows : | |||
*#In the early phase of evaluation in patients with recurrent [[syncope]] of uncertain origin, absence of high risk criteria and a high likelihood of recurrence within the battery life of the device | |||
*#In patients with suspected or certain [[reflex syncope]] presenting with frequent or severe [[Syncope|syncopal]] episodes | |||
*#In patients whom [[epilepsy]] was suspected but the treatment has proven ineffective. | |||
*#In patients with unexplained falls. {{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}} | |||
[ | *'''The ISSUE (International Study on Syncope of Unknown Etiology)''' study conducted by '''Brignole et a'''l monitored 198 patients with an [[implantable loop recorder]] and classified the first syncope event following implantation. | ||
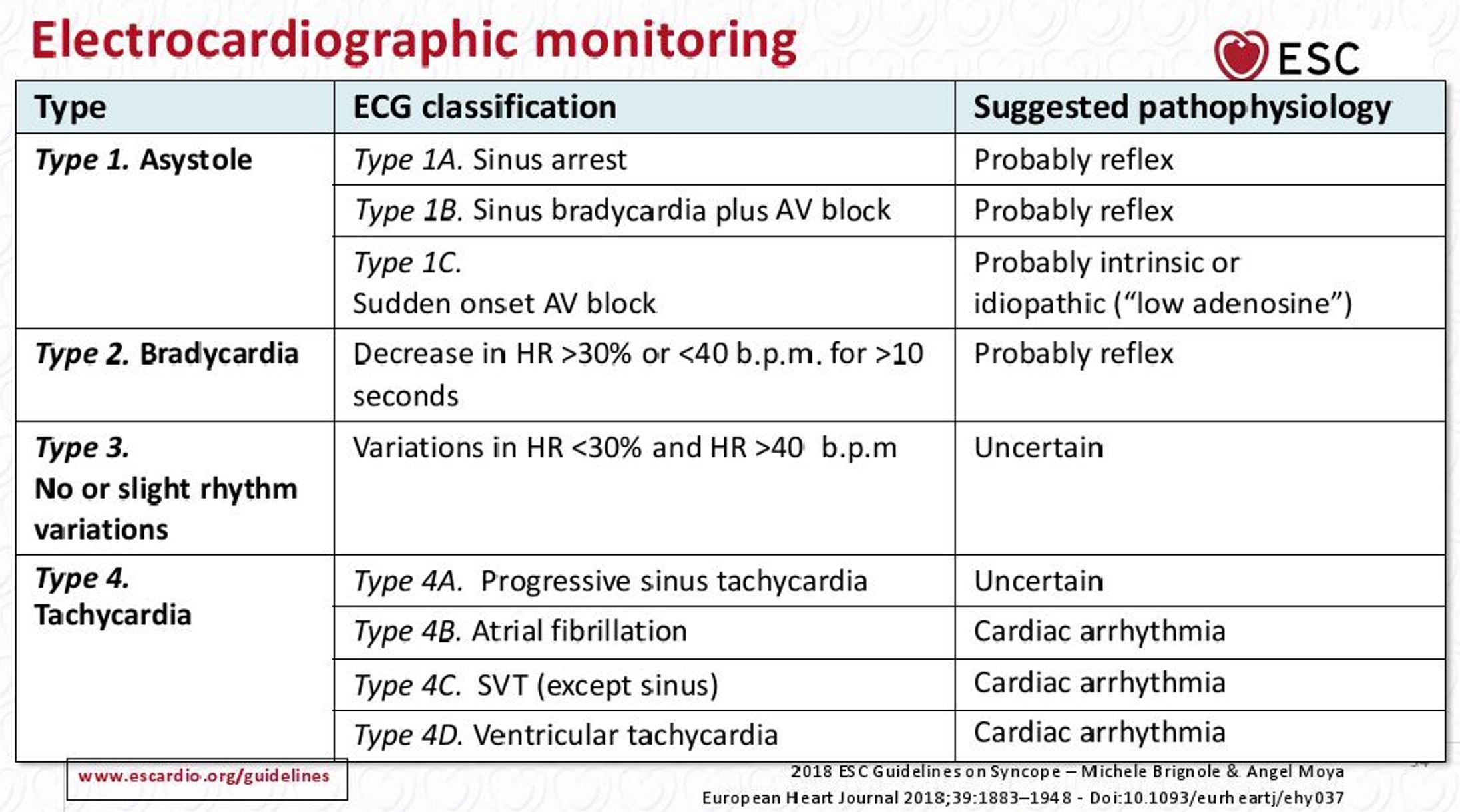
**The ISSUE classification has '''[[pathophysiological]] implications''' in terms of the event being [[neutrally mediated]] (type 1A or type 1B or type 2), due to an intrinsic [[Conduction System|conduction]] defect (type 1C), secondary to [[Orthostatic hypotension|orthostatic hypotension (]]<nowiki/>type 4A) or a primary [[cardiac]] [[Cardiac arrhythmia|arrhythmia]] (types 4B, 4C or 4D).<ref name="pmid15670961">{{cite journal| author=Brignole M, Moya A, Menozzi C, Garcia-Civera R, Sutton R| title=Proposed electrocardiographic classification of spontaneous syncope documented by an implantable loop recorder. | journal=Europace | year= 2005 | volume= 7 | issue= 1 | pages= 14-8 | pmid=15670961 | doi=10.1016/j.eupc.2004.11.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15670961 }} </ref> | |||
[[Image:ISSUE Classification.JPG|thumb|center|500px|ISSUE ECG Classification-{{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}}]] | |||
*'''The ISSUE 2 study''' (characterized by a frequently injured [[elderly]] population with a history of recurrent [[syncope]]) demonstrated the importance o[[Implantable loop recorders|f implantable loop recorders]] (ILR) as a [[Diagnosis|diagnostic]] modality by showing that '''the recurrence rate in [[syncope]] patients treated with ILR based therapy was much lower than those treated with no-specific therapy'''. | |||
**In addition, a recurrence rate of 5% was noted in those treated with [[cardiac pacing]].<ref name="pmid16569653">{{cite journal| author=Brignole M, Sutton R, Menozzi C, Garcia-Civera R, Moya A, Wieling W | display-authors=etal| title=Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope. | journal=Eur Heart J | year= 2006 | volume= 27 | issue= 9 | pages= 1085-92 | pmid=16569653 | doi=10.1093/eurheartj/ehi842 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16569653 }} </ref> | |||
= | =2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay:Recommendation for Implantable Cardiac Monitor= | ||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background: Pink"|[[2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay| Recommendation for Implantable Cardiac Monitor]] | |||
|- | |||
| bgcolor="Pink"|<nowiki>"</nowiki>'''1.''' In patients with infrequent symptoms (>30 days between symptoms) suspected to be caused by bradycardia, longterm ambulatory monitoring with an implantable cardiac monitor (ICM) is reasonable if initial noninvasive evaluation is nondiagnostic.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])'' <nowiki>"</nowiki> | |||
|} | |||
*An Implantable Cardiac Monitor is almost exclusively used in the diagnosis of [[bradycardia]] related disorders such as high-grade [[atrioventricular block]], [[sinus node dysfunction]] and [[neurocardiogenic syncope]] (with a predominant cardio-inhibitory component). | |||
*This prolonged monitoring (up to 3 years) can help correlate [[bradycardia]] [[Conduction System|conduction]] disorders with [[Symptom|symptoms]]<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>. | |||
==Electrophysiologic studies (EPS)== | |||
*[ | *The decision to perform an EPS requires a '''global risk assessment'''. | ||
*[ | **The application of this study is most important in diagnosing '''I-AVB'''. | ||
*According to the '''European Society of Cardiology''', indications for EPS are as follows : | |||
*# In patients with [[syncope]] and previous [[myocardial infarction]] or other scar related conditions, EPS is indicated when [[syncope]] remains unexplained after non- invasive evaluation. | |||
*#In patients with [[syncope]] and asymptomatic [[sinus bradycardia]], EPS may be considered in a few instances where no invasive tests (eg. ECG monitoring) have failed to show a correlation between [[syncope]] and [[bradycardia]]. | |||
*#In patients with [[syncope]] preceded by sudden and brief [[palpitations]], EPS may be considered when [[syncope]] remains unexplained after non invasive evaluation. {{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}} | |||
====EPS guided therapy==== | |||
*#In patients with unexplained [[syncope]] and bifasicular [[bundle branch block]], a [[pacemaker]] is indicated in the presence of either a baseline H-V interval of more than or equal to 70ms, or second or third degree [[His- Purkinje]] block during incremental atrial [[pacing]], or with pharmacological challenge. | |||
*[ | *# In patients with unexplained [[syncope]] and previous [[myocardial infarction]] or scar related condition, it is recommended to manage induction of sustained [[monomorphic ventricular tachycardia]] according to the current European Society of Cardiology Guidelines for [[Ventricular Arrhythmias]]. | ||
*#In patients without structural heart disease with [[syncope]] preceded by sudden and brief [[palpitations]], it is recommended to manage the induction of rapid [[SVT]] or [[Ventricular tachycardia|VT]], which reproduces [[Hypotension|hypotensive]] or spontaneous symptoms, with appropriate therapy according to the current European Society of Cardiology Guidelines. | |||
*#In patients with [[syncope]] and [[asymptomatic]] [[sinus bradycardia]], a [[pacemaker]] should be considered is a prolonged [[sinus node]] recovery time is present.{{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}} | |||
* | |||
*[ | *'''A 42 month follow up was performed by Gronda et al in 155 patients''', majority of whom had a history of previous syncope. | ||
**[ | **[[Electrophysiologic study]] findings of '''basal HV greater than or equal to 65 ms , HV value greater than or equal to 120 ms or 2nd-3rd degree atrioventricular block during ajmaline test and HV prolonged greater than 10 ms or 2nd-3rd degree [[atrioventricular block]] during atrial [[pacing]] correlated to an increased risk of developing advanced [[atrioventricular block]] below the [[AV node]]'''.<ref name="pmid6519386">{{cite journal| author=Gronda M, Magnani A, Occhetta E, Sauro G, D'Aulerio M, Carfora A | display-authors=etal| title=Electrophysiological study of atrio-ventricular block and ventricular conduction defects. Prognostic and therapeutical implications. | journal=G Ital Cardiol | year= 1984 | volume= 14 | issue= 10 | pages= 768-73 | pmid=6519386 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6519386 }} </ref> | ||
**[ | |||
**[ | [[Image:Diagnostic Summary 2.JPG|thumb|center|500px|EPS significance-{{cite web |url=https://onlinelibrary.wiley.com/doi/pdf/10.1016/j.joa.2017.03.008 |title=Syncope and paroxysmal atrioventricular block - Aste - 2017 - Journal of Arrhythmia - Wiley Online Library |format= |work= |accessdate=}}]] | ||
=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay= | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background: Lightgreen"|[[2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay| Recommendation for Electrophysiology Testing]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' In patients with symptoms suspected to be attributable to bradycardia, an electrophysiology study (EPS) may be considered in selected patients for diagnosis of, and elucidation of bradycardia mechanism, if initial noninvasive evaluation is nondiagnostic''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>''<nowiki>"</nowiki> | |||
|} | |||
*An EPS is an invasive [[catheter]] based procedure that is employed to detect and [[Anatomy|anatomically]] locate [[Conduction System|conduction]] disorders. | |||
*It is well tolerated, has a low [[Complications|complication]] risk and not usually employed as a first line study in the diagnosis of [[bradycardia]] related disorders. <ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref> | |||
==Vagal Maneuvers : Carotid Sinus massage and Tilt Table testing== | |||
*Though not specific,[[tilt table testing]] (TT) and other [[vagal]] maneuvers such as the [[vasalva]] maneuver, eye ball pressure and immersing one's face in cold water can be used in the diagnosis of '''EV-AVB'''. | |||
*'''The Syncope Unit Project-2 study''' found an increase recurrence rate in patients who did not undergo tilt table testing. This highlights '''the utility of TT as a screening test for reflex syncope'''.<ref name="pmid26612880">{{cite journal| author=Brignole M, Arabia F, Ammirati F, Tomaino M, Quartieri F, Rafanelli M | display-authors=etal| title=Standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncope: 3-year insights from the Syncope Unit Project 2 (SUP 2) study. | journal=Europace | year= 2016 | volume= 18 | issue= 9 | pages= 1427-33 | pmid=26612880 | doi=10.1093/europace/euv343 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26612880 }} </ref> | |||
*A positive response is indicated as a '''marker of [[hypotensive]] susceptibility which involves a decrease in both [[Preload (cardiology)|preload]] and [[afterload]]'''. | |||
*Having said that, a negative test '''does not rule out the possibility of an [[extrinsic vagal paroxysmal AV block]]'''. | |||
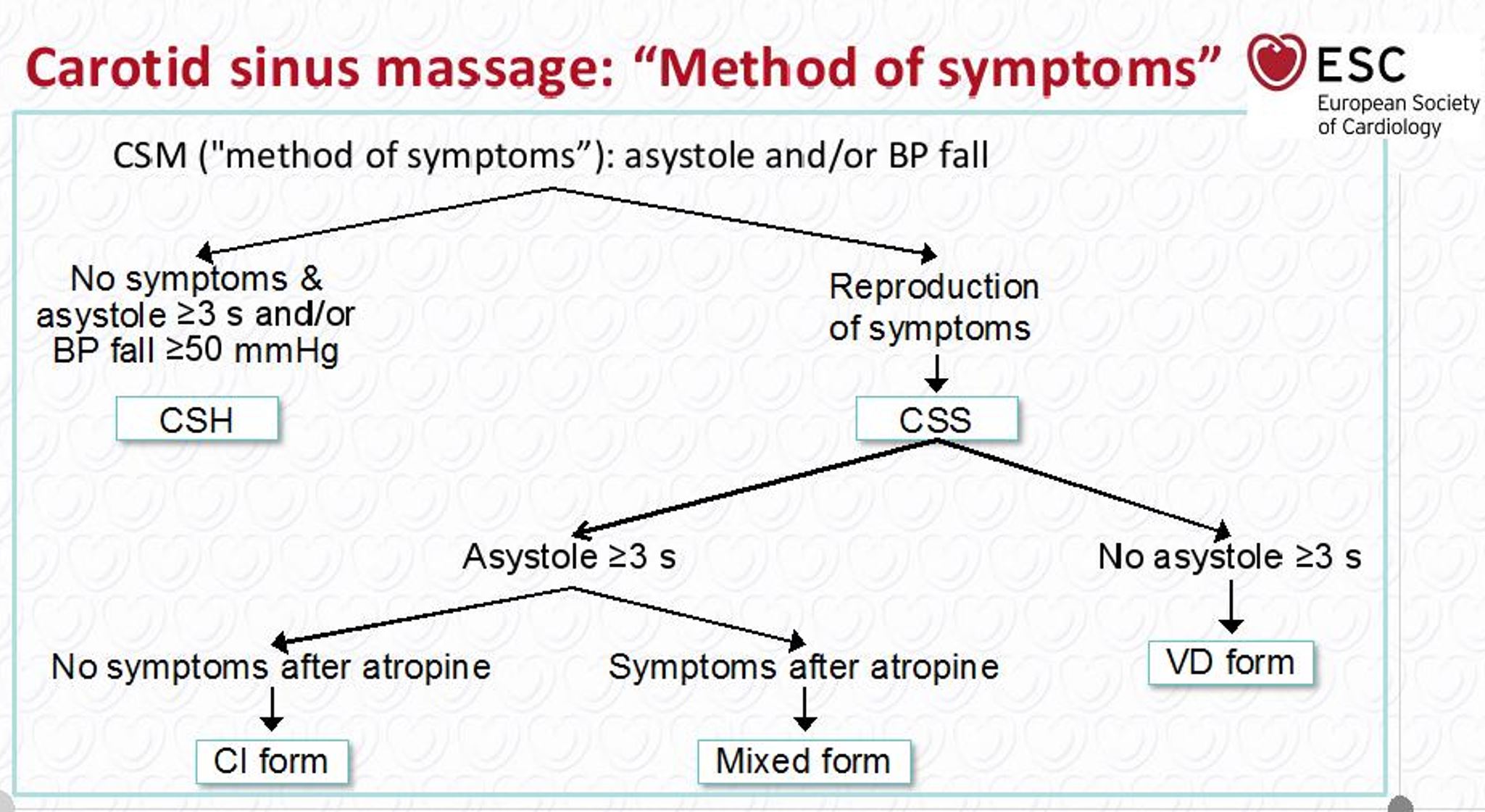
*A [[carotid sinus massage]] is indicated in '''patients more than 40 years of age with [[syncope]] of unknown origin compatible with [[reflex]] mechanism'''. | |||
**[[Carotid sinus]] sensitivity is confirmed if [[carotid sinus massage]] causes [[bradycardia]] ([[asystole]]) and/or [[hypotension]] that reproduce spontaneous symptoms and patients have clinical features compatible with [[reflex]] mechanism of [[syncope]]. {{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}} | |||
[[Image:Carotid Sinus Massage.JPG|thumb|center|500px|Carotid Sinus Massage- {{cite web |url=https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Syncope-Guidelines-on-Diagnosis-and-Management-of |title=ESC Guidelines on Syncope (Diagnosis and Management of) |format= |work= |accessdate=}}]] | |||
==References== | ==References== | ||
Latest revision as of 06:28, 11 July 2020
|
Paroxysmal AV block Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Paroxysmal AV block other diagnostic studies On the Web |
|
American Roentgen Ray Society Images of Paroxysmal AV block other diagnostic studies |
|
Risk calculators and risk factors for Paroxysmal AV block other diagnostic studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akash Daswaney, M.B.B.S[2]
Overview
An Implantable Cardiac Monitor is almost exclusively used in the diagnosis of bradycardia related disorders such as high-grade atrioventricular block, sinus node dysfunction and neurocardiogenic syncope (with predominant cardio-inhibitory component). This prolonged monitoring (up to 3 years) can help correlate bradycardia conduction disorders with symptoms. An EPS is an invasive catheter based procedure that is employed to detect and anatomically locate conduction disorders. An increased HH interval is seen in intrinsic paroxysmal AV Block. Certain maneuvers cause an increase in vagal surge and may precipitate symptoms in extrinsic vagal paroxysmal AV block. These include carotid sinus massage and tilt table testing.
Implantable Loop Recorder
- Implantable loop recorders are useful tools as they help correlate electrical tracings with the patients symptoms during an acute event.
- By giving an inkling of the etiology of the syncope, it helps guide therapy strategies, such as adopting permanent stimulation devices in patients with paroxysmal AV block.[1]
- According to the European Society of Cardiology, the indication for implantable loop recorders are as follows :
- In the early phase of evaluation in patients with recurrent syncope of uncertain origin, absence of high risk criteria and a high likelihood of recurrence within the battery life of the device
- In patients with suspected or certain reflex syncope presenting with frequent or severe syncopal episodes
- In patients whom epilepsy was suspected but the treatment has proven ineffective.
- In patients with unexplained falls. "ESC Guidelines on Syncope (Diagnosis and Management of)".
- The ISSUE (International Study on Syncope of Unknown Etiology) study conducted by Brignole et al monitored 198 patients with an implantable loop recorder and classified the first syncope event following implantation.
- The ISSUE classification has pathophysiological implications in terms of the event being neutrally mediated (type 1A or type 1B or type 2), due to an intrinsic conduction defect (type 1C), secondary to orthostatic hypotension (type 4A) or a primary cardiac arrhythmia (types 4B, 4C or 4D).[2]
- The ISSUE 2 study (characterized by a frequently injured elderly population with a history of recurrent syncope) demonstrated the importance of implantable loop recorders (ILR) as a diagnostic modality by showing that the recurrence rate in syncope patients treated with ILR based therapy was much lower than those treated with no-specific therapy.
- In addition, a recurrence rate of 5% was noted in those treated with cardiac pacing.[3]
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay:Recommendation for Implantable Cardiac Monitor
| Recommendation for Implantable Cardiac Monitor |
| "1. In patients with infrequent symptoms (>30 days between symptoms) suspected to be caused by bradycardia, longterm ambulatory monitoring with an implantable cardiac monitor (ICM) is reasonable if initial noninvasive evaluation is nondiagnostic.(Level of Evidence: C-LD) " |
- An Implantable Cardiac Monitor is almost exclusively used in the diagnosis of bradycardia related disorders such as high-grade atrioventricular block, sinus node dysfunction and neurocardiogenic syncope (with a predominant cardio-inhibitory component).
- This prolonged monitoring (up to 3 years) can help correlate bradycardia conduction disorders with symptoms[4].
Electrophysiologic studies (EPS)
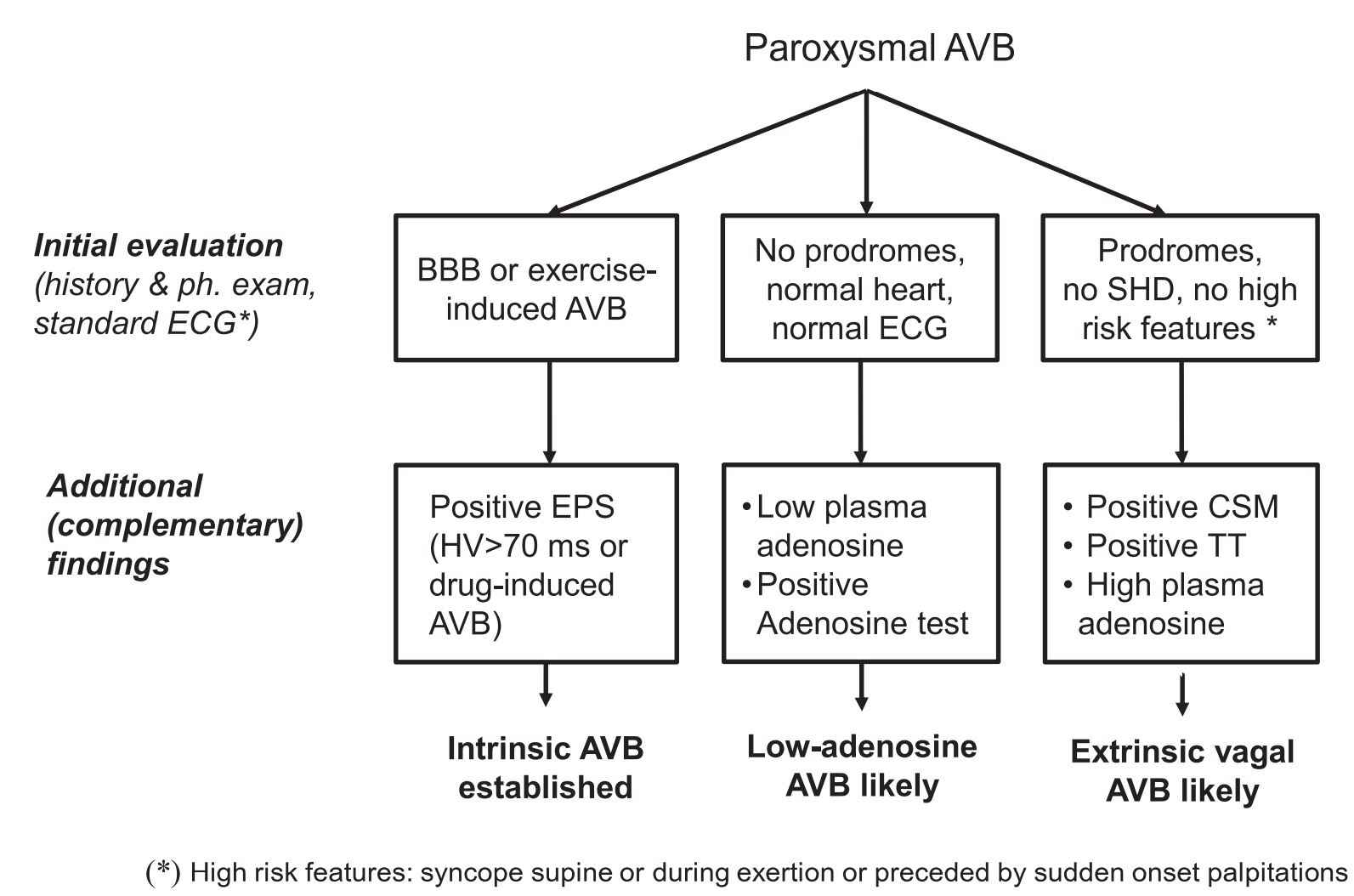
- The decision to perform an EPS requires a global risk assessment.
- The application of this study is most important in diagnosing I-AVB.
- According to the European Society of Cardiology, indications for EPS are as follows :
- In patients with syncope and previous myocardial infarction or other scar related conditions, EPS is indicated when syncope remains unexplained after non- invasive evaluation.
- In patients with syncope and asymptomatic sinus bradycardia, EPS may be considered in a few instances where no invasive tests (eg. ECG monitoring) have failed to show a correlation between syncope and bradycardia.
- In patients with syncope preceded by sudden and brief palpitations, EPS may be considered when syncope remains unexplained after non invasive evaluation. "ESC Guidelines on Syncope (Diagnosis and Management of)".
EPS guided therapy
- In patients with unexplained syncope and bifasicular bundle branch block, a pacemaker is indicated in the presence of either a baseline H-V interval of more than or equal to 70ms, or second or third degree His- Purkinje block during incremental atrial pacing, or with pharmacological challenge.
- In patients with unexplained syncope and previous myocardial infarction or scar related condition, it is recommended to manage induction of sustained monomorphic ventricular tachycardia according to the current European Society of Cardiology Guidelines for Ventricular Arrhythmias.
- In patients without structural heart disease with syncope preceded by sudden and brief palpitations, it is recommended to manage the induction of rapid SVT or VT, which reproduces hypotensive or spontaneous symptoms, with appropriate therapy according to the current European Society of Cardiology Guidelines.
- In patients with syncope and asymptomatic sinus bradycardia, a pacemaker should be considered is a prolonged sinus node recovery time is present."ESC Guidelines on Syncope (Diagnosis and Management of)".
- A 42 month follow up was performed by Gronda et al in 155 patients, majority of whom had a history of previous syncope.
- Electrophysiologic study findings of basal HV greater than or equal to 65 ms , HV value greater than or equal to 120 ms or 2nd-3rd degree atrioventricular block during ajmaline test and HV prolonged greater than 10 ms or 2nd-3rd degree atrioventricular block during atrial pacing correlated to an increased risk of developing advanced atrioventricular block below the AV node.[5]
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay
| Recommendation for Electrophysiology Testing |
| "1. In patients with symptoms suspected to be attributable to bradycardia, an electrophysiology study (EPS) may be considered in selected patients for diagnosis of, and elucidation of bradycardia mechanism, if initial noninvasive evaluation is nondiagnostic(Level of Evidence: C-LD)[4]" |
- An EPS is an invasive catheter based procedure that is employed to detect and anatomically locate conduction disorders.
- It is well tolerated, has a low complication risk and not usually employed as a first line study in the diagnosis of bradycardia related disorders. [4]
Vagal Maneuvers : Carotid Sinus massage and Tilt Table testing
- Though not specific,tilt table testing (TT) and other vagal maneuvers such as the vasalva maneuver, eye ball pressure and immersing one's face in cold water can be used in the diagnosis of EV-AVB.
- The Syncope Unit Project-2 study found an increase recurrence rate in patients who did not undergo tilt table testing. This highlights the utility of TT as a screening test for reflex syncope.[6]
- A positive response is indicated as a marker of hypotensive susceptibility which involves a decrease in both preload and afterload.
- Having said that, a negative test does not rule out the possibility of an extrinsic vagal paroxysmal AV block.
- A carotid sinus massage is indicated in patients more than 40 years of age with syncope of unknown origin compatible with reflex mechanism.
- Carotid sinus sensitivity is confirmed if carotid sinus massage causes bradycardia (asystole) and/or hypotension that reproduce spontaneous symptoms and patients have clinical features compatible with reflex mechanism of syncope. "ESC Guidelines on Syncope (Diagnosis and Management of)".
References
- ↑ Guerrero-Márquez FJ, Arana-Rueda E, Pedrote A (2016). "Idiopathic Paroxysmal Atrio-Ventricular Block. What is The Mechanism?". J Atr Fibrillation. 9 (3): 1449. doi:10.4022/jafib.1449. PMC 5368548. PMID 28496928.
- ↑ Brignole M, Moya A, Menozzi C, Garcia-Civera R, Sutton R (2005). "Proposed electrocardiographic classification of spontaneous syncope documented by an implantable loop recorder". Europace. 7 (1): 14–8. doi:10.1016/j.eupc.2004.11.001. PMID 15670961.
- ↑ Brignole M, Sutton R, Menozzi C, Garcia-Civera R, Moya A, Wieling W; et al. (2006). "Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope". Eur Heart J. 27 (9): 1085–92. doi:10.1093/eurheartj/ehi842. PMID 16569653.
- ↑ 4.0 4.1 4.2 Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR; et al. (2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society". J Am Coll Cardiol. 74 (7): 932–987. doi:10.1016/j.jacc.2018.10.043. PMID 30412710.
- ↑ Gronda M, Magnani A, Occhetta E, Sauro G, D'Aulerio M, Carfora A; et al. (1984). "Electrophysiological study of atrio-ventricular block and ventricular conduction defects. Prognostic and therapeutical implications". G Ital Cardiol. 14 (10): 768–73. PMID 6519386.
- ↑ Brignole M, Arabia F, Ammirati F, Tomaino M, Quartieri F, Rafanelli M; et al. (2016). "Standardized algorithm for cardiac pacing in older patients affected by severe unpredictable reflex syncope: 3-year insights from the Syncope Unit Project 2 (SUP 2) study". Europace. 18 (9): 1427–33. doi:10.1093/europace/euv343. PMID 26612880.