Paroxysmal AV block history and symptoms
|
Paroxysmal AV block Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Paroxysmal AV block history and symptoms On the Web |
|
American Roentgen Ray Society Images of Paroxysmal AV block history and symptoms |
|
Risk calculators and risk factors for Paroxysmal AV block history and symptoms |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akash Daswaney, M.B.B.S[2]
Overview
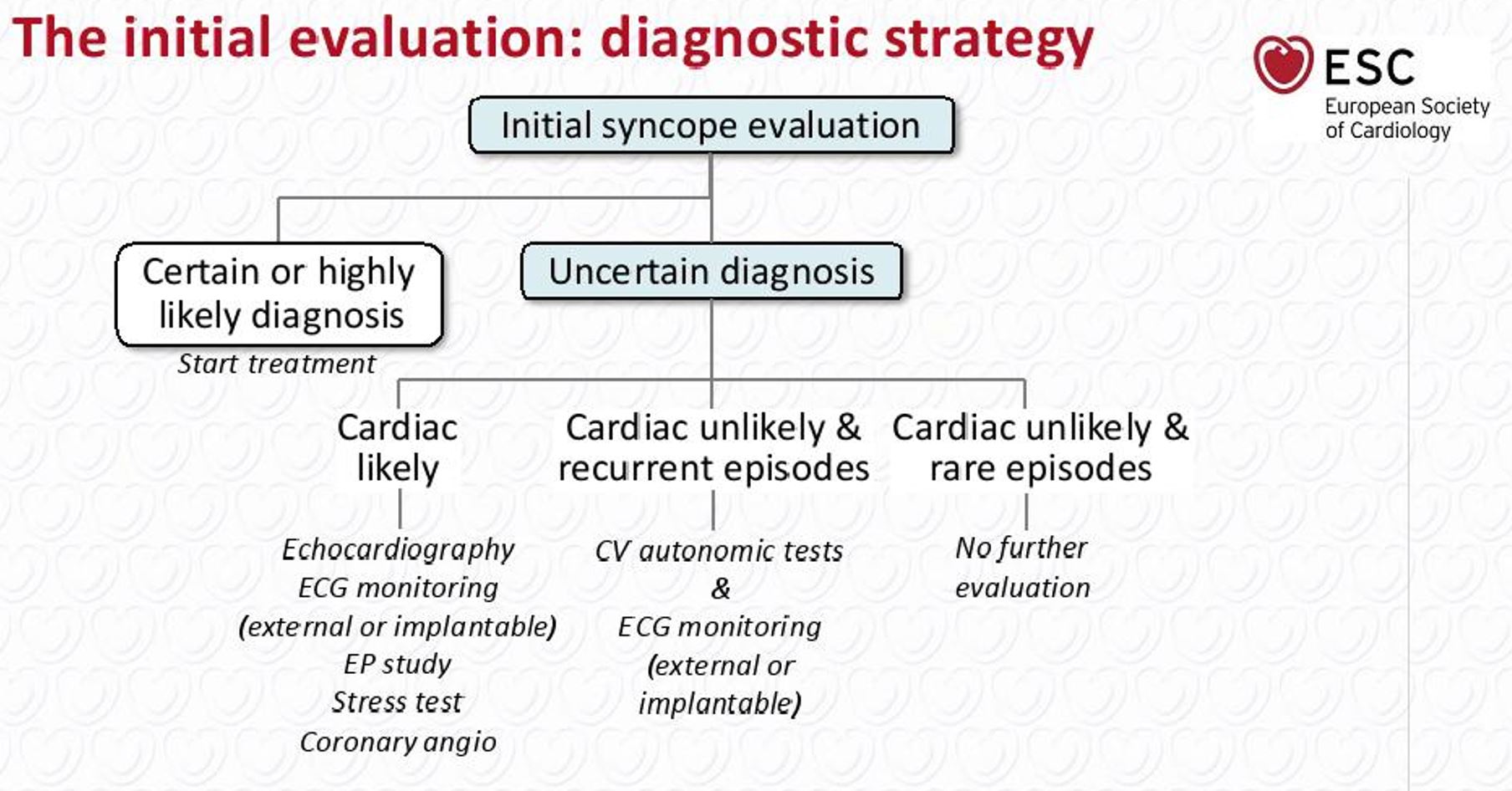
An initial evaluation strategy of taking a detailed history, physical examination, risk stratification, ECG recording and BP measurement should help decide what investigations should be ordered (based on whether the syncope is cardiac related, reflex/neutrally mediated, secondary to cerebrovascular disease or due to orthostatic hypotension). The majority of patients with paroxysmal AV Block present with presyncope, syncope, with or without a prodrome or are asymptomatic.
Initial Approach
- The pathway to conclusively diagnosing a patient with paroxysmal AV block is not straightforward.
- Since most patients present with a history of recurrent unexplained syncope and fortuitous timing would be required to document classical ECG findings during an acute episode, it would be best to treat it as a diagnosis of exclusion.
- An initial evaluation strategy of taking a detailed history, physical examination, risk stratification, ECG recording and BP measurement should help decide what investigations should be ordered (based on whether the syncope is cardiac related, reflex/neutrally mediated, secondary to cerebrovascular disease or due to orthostatic hypotension). "ESC Guidelines on Syncope (Diagnosis and Management of)".
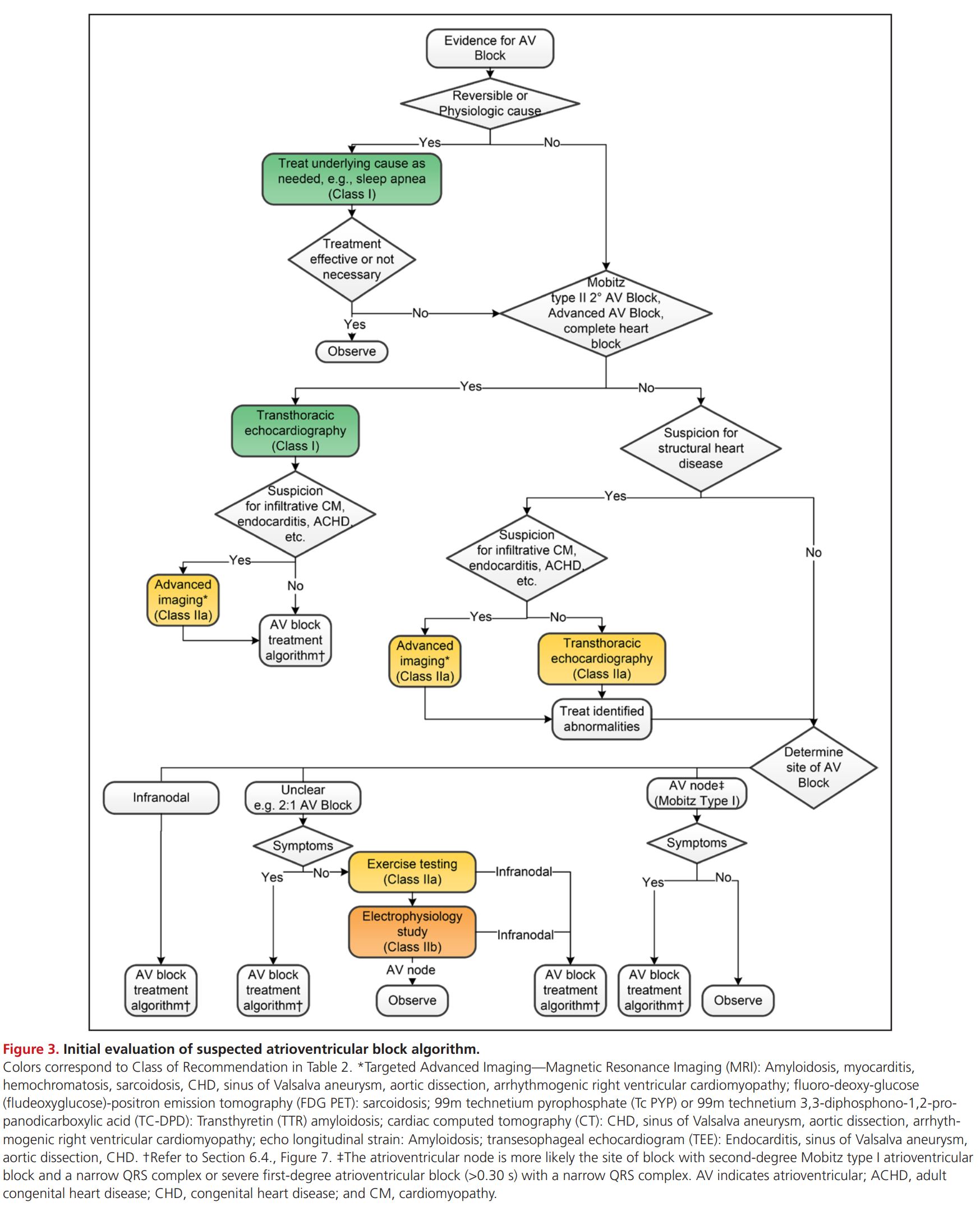
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Approach to AV Block
History and Symptoms
- History of syncope, presyncope, duration of each episode, number of episodes, activities during the syncopal episode, aggravating or relieving factors, history of past medical illnesses, prodrome/ recovery phase description in terms of signs, symptoms and duration are important points to be addressed whilst taking a history of a syncope patient.
- A study of 341 syncope patients showed that the time between the first and last syncopal episode being less than 4 years, syncope during effort or supine position, a history of palpitations, convulsions or blurring of vision were important predictors of a cardiac syncope.
- Similarly, duration of prodrome > 10 seconds history of pallor, nausea, diaphoresis, dizziness, presyncope, abdominal discomfort and time between first and last syncopal episode being more than 4 years were important predictors of a neutrally mediated syncope.[2]
- Based on a detailed history, one can decide whether a cardiac syncope was secondary to a rhythm dysfunction, structural cause or ischemia related and would warrant a work up of an ECG, Holter monitoring, echocardiography, electrophysiologic study, or an exercise stress test. [2]
- Similarly, neutrally mediated syncope maybe vasovagal, situational, secondary to increased carotid sinus sensitivity or non classical and orthostatic hypotension may be due to a primary or secondary autonomic failure, secondary to drugs or hypovolemia. This may be further explored by a carotid sinus massage, tilt table testing, adenosine plasma levels or an adenosine triphosphate stimulation test."ESC Guidelines on Syncope (Diagnosis and Management of)".
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Recommendation for History and Physical Examination of Patients With Documented or Suspected Bradycardia or Conduction Disorders
| Recommendation for History and Physical Examination of Patients With Documented or Suspected Bradycardia or Conduction Disorders |
| "1. In patients with suspected bradycardia or conduction disorders a comprehensive history and physical examination should be
performed. (Level of Evidence: C- EO)[1]" |
- Important aspects of one’s history include the frequency, timing, duration, severity, longevity, circumstances, triggers (eg, urination, defecation, cough, prolonged standing, shaving, tight collars, and head turning) and alleviating factors of symptoms suspicious for bradycardia or conduction disorders.
- A thorough family history, medical history, cardiovascular history and review of symptoms should also be done. [1]
References
- ↑ 1.0 1.1 1.2 Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR; et al. (2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society". J Am Coll Cardiol. 74 (7): 932–987. doi:10.1016/j.jacc.2018.10.043. PMID 30412710.
- ↑ 2.0 2.1 Alboni P, Brignole M, Menozzi C, Raviele A, Del Rosso A, Dinelli M, Solano A, Bottoni N (June 2001). "Diagnostic value of history in patients with syncope with or without heart disease". J. Am. Coll. Cardiol. 37 (7): 1921–8. doi:10.1016/s0735-1097(01)01241-4. PMID 11401133.