Acute aortic syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 28: | Line 28: | ||
*For more information on [[penetrating atherosclerotic aortic ulcer]] causes [[Penetrating atherosclerotic aortic ulcer|click here]]. | *For more information on [[penetrating atherosclerotic aortic ulcer]] causes [[Penetrating atherosclerotic aortic ulcer|click here]]. | ||
==Guidelines== | ==Guidelines== | ||
==2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)<ref name="pmid25173340">{{cite journal |vauthors=Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ |title=2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC) |journal=Eur. Heart J. |volume=35 |issue=41 |pages=2873–926 |date=November 2014 |pmid=25173340 |doi=10.1093/eurheartj/ehu281 |url=}}</ref>== | ===2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)<ref name="pmid25173340">{{cite journal |vauthors=Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ |title=2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC) |journal=Eur. Heart J. |volume=35 |issue=41 |pages=2873–926 |date=November 2014 |pmid=25173340 |doi=10.1093/eurheartj/ehu281 |url=}}</ref>=== | ||
{| border="4" | |||
|+ | |||
! style="background: #FFFF00; width: 150px;" | Recomendacations !! style="background: #FFFF00; width: 150px;" | Class !! style="background: #FFFF00; width: 150px;" | Level !! style="background: #FFFF00; width: 150px;" | References | |||
|- | |||
! colspan="4" align="left" |History and clinical assessment | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0; " align="left" |In all patients with suspected | |||
AAS, pre-test probability | |||
assessment is recommended, | |||
according to the patient’s | |||
condition, symptoms, and | |||
clinical features. | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #0000CD;" align="center" |'''B''' | |||
|" align="center" |<ref name="EvangelistaIsselbacher2018">{{cite journal|last1=Evangelista|first1=Arturo|last2=Isselbacher|first2=Eric M.|last3=Bossone|first3=Eduardo|last4=Gleason|first4=Thomas G.|last5=Eusanio|first5=Marco Di|last6=Sechtem|first6=Udo|last7=Ehrlich|first7=Marek P.|last8=Trimarchi|first8=Santi|last9=Braverman|first9=Alan C.|last10=Myrmel|first10=Truls|last11=Harris|first11=Kevin M.|last12=Hutchinson|first12=Stuart|last13=O’Gara|first13=Patrick|last14=Suzuki|first14=Toru|last15=Nienaber|first15=Christoph A.|last16=Eagle|first16=Kim A.|title=Insights From the International Registry of Acute Aortic Dissection|journal=Circulation|volume=137|issue=17|year=2018|pages=1846–1860|issn=0009-7322|doi=10.1161/CIRCULATIONAHA.117.031264}}</ref> | |||
|- | |||
! colspan="4" align="left" | Laboratory testing | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0; " align="left" |In case of suspicion of AAS, | |||
the interpretation of | |||
biomarkers should always be | |||
considered along with the pretest | |||
clinical probability. | |||
| style="padding: 5px 5px; background: #FFA500;" align="center" |'''IIa''' | |||
| style="padding: 5px 5px; background: #0000CD;" align="center" |'''B''' | |||
| | |||
|- | |||
! style="padding: 5px 5px; " align="left" |In case of low clinical | |||
probability of AAS, negative D-dimer | |||
levels should be | |||
considered as ruling out the | |||
diagnosis. | |||
| style="padding: 5px 5px; background: #FFA500;" align="center" |'''IIa''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
| align="center" |<ref name="EggebrechtMehta2008">{{cite journal|last1=Eggebrecht|first1=Holger|last2=Mehta|first2=Rajendra H.|last3=Metozounve|first3=Huguette|last4=Huptas|first4=Sebastian|last5=Herold|first5=Ulf|last6=Jakob|first6=Heinz G.|last7=Erbel|first7=Raimund|title=Clinical Implications of Systemic Inflammatory Response Syndrome Following Thoracic Aortic Stent-Graft Placement|journal=Journal of Endovascular Therapy|volume=15|issue=2|year=2008|pages=135–143|issn=1526-6028|doi=10.1583/07-2284.1}}</ref><ref name="SutherlandEscano2008">{{cite journal|last1=Sutherland|first1=Alexander|last2=Escano|first2=Jude|last3=Coon|first3=Troy P.|title=D-dimer as the Sole Screening Test for Acute Aortic Dissection: A Review of the Literature|journal=Annals of Emergency Medicine|volume=52|issue=4|year=2008|pages=339–343|issn=01960644|doi=10.1016/j.annemergmed.2007.12.026}}</ref><ref name="SuzukiBossone2013">{{cite journal|last1=Suzuki|first1=Toru|last2=Bossone|first2=Eduardo|last3=Sawaki|first3=Daigo|last4=Jánosi|first4=Rolf Alexander|last5=Erbel|first5=Raimund|last6=Eagle|first6=Kim|last7=Nagai|first7=Ryozo|title=Biomarkers of aortic diseases|journal=American Heart Journal|volume=165|issue=1|year=2013|pages=15–25|issn=00028703|doi=10.1016/j.ahj.2012.10.006}}</ref><ref name="TaylorIyer2013">{{cite journal|last1=Taylor|first1=R. Andrew|last2=Iyer|first2=Neel S.|title=A decision analysis to determine a testing threshold for computed tomographic angiography and d-dimer in the evaluation of aortic dissection|journal=The American Journal of Emergency Medicine|volume=31|issue=7|year=2013|pages=1047–1055|issn=07356757|doi=10.1016/j.ajem.2013.03.039}}</ref> | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0; " align="left" |In case of intermediate clinical | |||
probability of AAS with a | |||
positive (point-of-care) D-dimer | |||
test, further imaging | |||
tests should be considered. | |||
| style="padding: 5px 5px; background: #FFA500;" align="center" |'''IIa''' | |||
| style="padding: 5px 5px; background: #0000CD;" align="center" |'''B''' | |||
| align="center" |<ref name="EggebrechtMehta2008">{{cite journal|last1=Eggebrecht|first1=Holger|last2=Mehta|first2=Rajendra H.|last3=Metozounve|first3=Huguette|last4=Huptas|first4=Sebastian|last5=Herold|first5=Ulf|last6=Jakob|first6=Heinz G.|last7=Erbel|first7=Raimund|title=Clinical Implications of Systemic Inflammatory Response Syndrome Following Thoracic Aortic Stent-Graft Placement|journal=Journal of Endovascular Therapy|volume=15|issue=2|year=2008|pages=135–143|issn=1526-6028|doi=10.1583/07-2284.1}}</ref><ref name="SutherlandEscano2008">{{cite journal|last1=Sutherland|first1=Alexander|last2=Escano|first2=Jude|last3=Coon|first3=Troy P.|title=D-dimer as the Sole Screening Test for Acute Aortic Dissection: A Review of the Literature|journal=Annals of Emergency Medicine|volume=52|issue=4|year=2008|pages=339–343|issn=01960644|doi=10.1016/j.annemergmed.2007.12.026}}</ref> | |||
|- | |||
! style="padding: 5px 5px;" align="left" |In patients with high probability | |||
(risk score 2 or 3) of AD, | |||
testing of D-dimers is not | |||
recommended. | |||
| style="padding: 5px 5px; background: #F08080;" align="center" |'''III''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
| | |||
|- | |||
! colspan="4" align="left" |Imaging | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0; " align="left" |TTE is recommended as an | |||
initial imaging investigation. | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
! style="padding: 5px 5px; " align="left" |In unstabled patients with a | |||
suspicion of AAS, the following | |||
imaging modalities are | |||
recommended according to | |||
local availability and expertise: | |||
! | |||
! | |||
! | |||
|- | |||
!TOE | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
!CT | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0; " align="left" |In stable patients with a | |||
suspicion of AAS, the | |||
following imaging modalities | |||
are recommended (or should | |||
be considered) according to | |||
local availability and expertise: | |||
! | |||
! | |||
! | |||
|- | |||
!CT | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
!MRI | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
!TOE | |||
| style="padding: 5px 5px; background: #FFA500;" align="center" |'''IIa''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0; " align="left" |In case of initially negative | |||
imaging with the persistence of | |||
suspicion of AAS, repetitive | |||
imaging (CT or MRI) is | |||
recommended. | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
! style="padding: 5px 5px;" align="left" |Chest X-ray maybe | |||
considered in cases of low | |||
clinical probability of AAS. | |||
| style="padding: 5px 5px; background: #FFA500;" align="center" |'''IIb''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|- | |||
! style="padding: 5px 5px; background: #FFFFE0;" align="left" |In case of uncomplicated | |||
Type B AD treated medically, | |||
repeated imaging (CT or | |||
MRI)e during the first days is | |||
recommended. | |||
| style="padding: 5px 5px; background: #90EE90;" align="center" |'''I''' | |||
| style="padding: 5px 5px; background: #6495ED;" align="center" |'''C''' | |||
! | |||
|} | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Revision as of 04:08, 25 December 2019
 |
|
Acute aortic syndrome Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2]
Overview
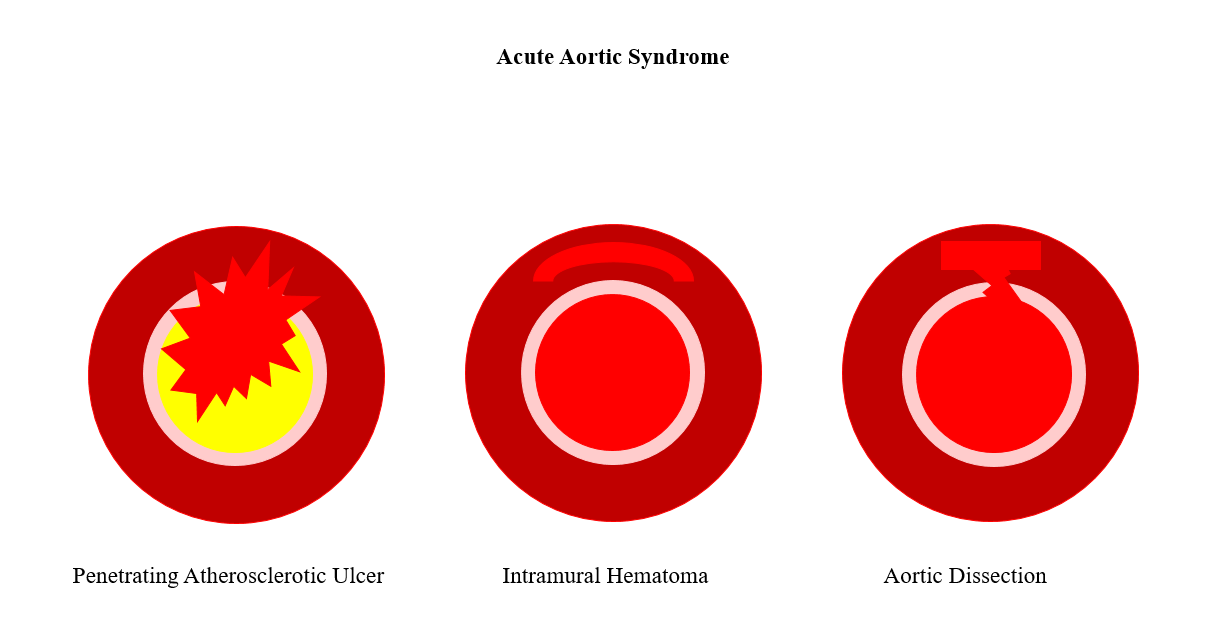
Acute aortic syndrome (AAS) describes a constellation of emergency conditions with a similar clinical feature that involves the aorta. These include aortic dissection, intramural thrombus, and penetrating atherosclerotic aortic ulcer. It is possible for AAS to lead to acute coronary syndrome. The term was introduced in 2001.
Classification
Acute aortic syndromes is classified into 5 entities as follows:[1][2]
- Type I: classic aortic dissection involving an intimal layer between the true and false lumen (with no communication between the two lumen)
- Type II: aortic dissection with medial rupture and the subsequent intramural hematoma formation
- Type III: subtle aortic dissection with bulging of the aortic wall
- Type IV: aortic dissection due to plaque rupture and subsequent ulceration
- Type V: iatrogenic/traumatic dissection
Differentiating Acute Aortic Syndrome from other Diseases
- Acute aortic syndrome should be differentiated from other conditions causing signs and symptoms such as chest pain, dyspnea, back pain and etc.
- For more information on the differential diagnosis of the acute aortic syndrome click here.
Causes
- Causes include aortic dissection, intramural hematoma, penetrating atherosclerotic ulcer or a thoracic aneurysm that has become unstable.[3]
- Basically, AAS can be caused by a breakdown on the wall of the aorta that involves the tunica intima and/or media.[4]
- For more information on aortic dissection causes click here.
- For more information on aortic intramural hematoma causes click here.
- For more information on penetrating atherosclerotic aortic ulcer causes click here.
Guidelines
2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)[5]
| Recomendacations | Class | Level | References |
|---|---|---|---|
| History and clinical assessment | |||
| In all patients with suspected
AAS, pre-test probability assessment is recommended, according to the patient’s condition, symptoms, and clinical features. |
I | B | [6] |
| Laboratory testing | |||
| In case of suspicion of AAS,
the interpretation of biomarkers should always be considered along with the pretest clinical probability. |
IIa | B | |
| In case of low clinical
probability of AAS, negative D-dimer levels should be considered as ruling out the diagnosis. |
IIa | C | [7][8][9][10] |
| In case of intermediate clinical
probability of AAS with a positive (point-of-care) D-dimer test, further imaging tests should be considered. |
IIa | B | [7][8] |
| In patients with high probability
(risk score 2 or 3) of AD, testing of D-dimers is not recommended. |
III | C | |
| Imaging | |||
| TTE is recommended as an
initial imaging investigation. |
I | C | |
| In unstabled patients with a
suspicion of AAS, the following imaging modalities are recommended according to local availability and expertise: |
|||
| TOE | I | C | |
| CT | I | C | |
| In stable patients with a
suspicion of AAS, the following imaging modalities are recommended (or should be considered) according to local availability and expertise: |
|||
| CT | I | C | |
| MRI | I | C | |
| TOE | IIa | C | |
| In case of initially negative
imaging with the persistence of suspicion of AAS, repetitive imaging (CT or MRI) is recommended. |
I | C | |
| Chest X-ray maybe
considered in cases of low clinical probability of AAS. |
IIb | C | |
| In case of uncomplicated
Type B AD treated medically, repeated imaging (CT or MRI)e during the first days is recommended. |
I | C | |
References
- ↑ Erbel, R (2001). "Diagnosis and management of aortic dissection Task Force on Aortic Dissection, European Society of Cardiology". European Heart Journal. 22 (18): 1642–1681. doi:10.1053/euhj.2001.2782. ISSN 0195-668X.
- ↑ "2014 ESC Guidelines on the diagnosis and treatment of aortic diseases". European Heart Journal. 35 (41): 2873–2926. 2014. doi:10.1093/eurheartj/ehu281. ISSN 0195-668X.
- ↑ Smith AD, Schoenhagen P (January 2008). "CT imaging for acute aortic syndrome". Cleve Clin J Med. 75 (1): 7–9, 12, 15–7 passim. doi:10.3949/ccjm.75.1.7. PMID 18236724.
- ↑ Evangelista Masip A (April 2007). "[Progress in the acute aortic syndrome]". Rev Esp Cardiol (in Spanish; Castilian). 60 (4): 428–39. doi:10.1157/13101646. PMID 17521551.
- ↑ Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwöger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, Allmen RS, Vrints CJ (November 2014). "2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC)". Eur. Heart J. 35 (41): 2873–926. doi:10.1093/eurheartj/ehu281. PMID 25173340.
- ↑ Evangelista, Arturo; Isselbacher, Eric M.; Bossone, Eduardo; Gleason, Thomas G.; Eusanio, Marco Di; Sechtem, Udo; Ehrlich, Marek P.; Trimarchi, Santi; Braverman, Alan C.; Myrmel, Truls; Harris, Kevin M.; Hutchinson, Stuart; O’Gara, Patrick; Suzuki, Toru; Nienaber, Christoph A.; Eagle, Kim A. (2018). "Insights From the International Registry of Acute Aortic Dissection". Circulation. 137 (17): 1846–1860. doi:10.1161/CIRCULATIONAHA.117.031264. ISSN 0009-7322.
- ↑ 7.0 7.1 Eggebrecht, Holger; Mehta, Rajendra H.; Metozounve, Huguette; Huptas, Sebastian; Herold, Ulf; Jakob, Heinz G.; Erbel, Raimund (2008). "Clinical Implications of Systemic Inflammatory Response Syndrome Following Thoracic Aortic Stent-Graft Placement". Journal of Endovascular Therapy. 15 (2): 135–143. doi:10.1583/07-2284.1. ISSN 1526-6028.
- ↑ 8.0 8.1 Sutherland, Alexander; Escano, Jude; Coon, Troy P. (2008). "D-dimer as the Sole Screening Test for Acute Aortic Dissection: A Review of the Literature". Annals of Emergency Medicine. 52 (4): 339–343. doi:10.1016/j.annemergmed.2007.12.026. ISSN 0196-0644.
- ↑ Suzuki, Toru; Bossone, Eduardo; Sawaki, Daigo; Jánosi, Rolf Alexander; Erbel, Raimund; Eagle, Kim; Nagai, Ryozo (2013). "Biomarkers of aortic diseases". American Heart Journal. 165 (1): 15–25. doi:10.1016/j.ahj.2012.10.006. ISSN 0002-8703.
- ↑ Taylor, R. Andrew; Iyer, Neel S. (2013). "A decision analysis to determine a testing threshold for computed tomographic angiography and d-dimer in the evaluation of aortic dissection". The American Journal of Emergency Medicine. 31 (7): 1047–1055. doi:10.1016/j.ajem.2013.03.039. ISSN 0735-6757.