|
|
| Line 5: |
Line 5: |
|
| |
|
| ==Overview== | | ==Overview== |
| '''Glucose-6-phosphate dehydrogenase (G6PD) deficiency''' is an [[Sex-linked|X-linked recessive]] [[hereditary disease]] featuring abnormally low levels of the [[G6PD]] enzyme, which plays an important role in [[red blood cell]] function. Individuals with the disease may exhibit non-immune [[hemolytic anemia]] in response to a number of causes. It is closely linked to '''[[favism]]''', a disorder characterized by a hemolytic reaction to consumption of [[Vicia faba|broad bean]]s, with a name derived from the [[Italian language|Italian]] name of the broad bean (''fava''). Sometimes the name, [[favism]], is alternatively used to refer to the enzyme
| | |
| deficiency as a whole.
| |
| ==Pathophysiology== | | ==Pathophysiology== |
|
| |
|
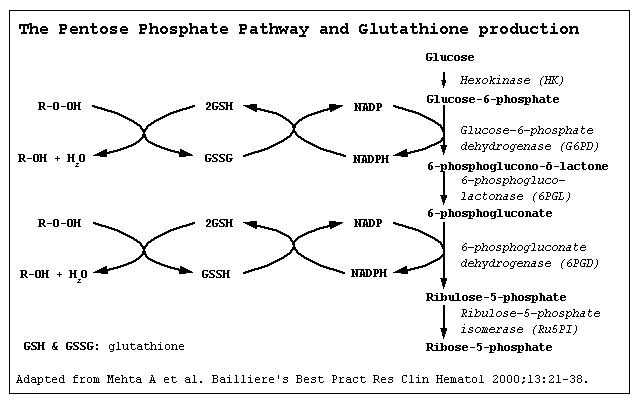
| * [[Glucose-6-phosphate dehydrogenase]] ([[G6PD]]) is an [[enzyme]] in the [[pentose phosphate pathway]], a [[metabolic pathway]] that supplies reducing energy to cells (most notably [[erythrocyte]]s) by maintaining the level of the [[co-enzyme]] [[nicotinamide adenine dinucleotide phosphate|nicotinamide adenine dinucleotide phosphate]] (NADPH). | | * |
| * The NADPH in turn maintains the level of [[glutathione]] in these cells that helps protect the red blood cells against [[oxidation|oxidative]] damage. G6PD converts [[glucose-6-phosphate]] into [[6-phosphoglucono-δ-lactone]] and is the rate-limiting enzyme of the ''pentose phosphate pathway''.
| |
| * Patients with [[G6PD deficiency]] are at risk of [[hemolytic anemia]] in states of [[oxidative stress]]. This can be in severe infection, [[medication]] and certain foods. [[Broad bean]]s contain high levels of vicine, divicine, convicine and isouramil — all are [[oxidant]]s.
| |
| * In states of oxidative stress, all remaining [[glutathione]] is consumed. Enzymes and other proteins (including [[hemoglobin]]) are subsequently damaged by the oxidants, leading to [[electrolyte]] imbalance, membrane cross-bonding and [[phagocytosis]] and [[spleen|splenic]] sequestration of red blood cells. The hemoglobin is metabolized to [[bilirubin]] (causing [[jaundice]] at high concentrations) or excreted directly by the [[kidney]] (causing [[acute renal failure]] in severe cases).
| |
| * Deficiency of G6PD in the alternative pathway causes the build up of glucose and thus there is an increase of [[advanced glycation endproduct]]s (AGE). The deficiency also causes a reduction of NADPH which is necessary for the formation of Nitric Oxide (NO). The high prevalence of [[diabetes mellitus type 2]] and [[hypertension]] in Afro-Caribbeans in the West could be directly related to G6PD deficiency.<ref>{{cite journal |author=Gaskin RS, Estwick D, Peddi R |title=G6PD deficiency: its role in the high prevalence of hypertension and diabetes mellitus |journal=Ethnicity & disease |volume=11 |issue=4 |pages=749–54 |year=2001 |pmid=11763298 |doi=}}</ref>
| |
| * Some other epidemiological reports have pointed out, however, that G6PD seems to decrease the susceptibility to [[cancer]], [[cardiovascular disease]] and [[stroke]].
| |
| * Although female carriers can have a mild form of G6PD deficiency (dependent on the degree of inactivation of the unaffected X chromosome - see ''[[lyonization]]''), homozygous females have been described; in these females there is co-incidence of a [[rare disease|rare]] [[immunology|immune disorder]] termed [[chronic granulomatous disease]] (CGD).
| |
|
| |
|
| [[image:G6PD_mechanism.png|550px|left|Mechanism of G6PD]] | | [[image:G6PD_mechanism.png|550px|left|Mechanism of G6PD]] |
| <br clear="center"/> | | <br clear="center" /> |
|
| |
|
| ==References== | | ==References== |