Primitive neuroectodermal tumor: Difference between revisions
| (13 intermediate revisions by the same user not shown) | |||
| Line 30: | Line 30: | ||
*[[Histopathological|Histopathologically]], primitive neuroectodermal tumors should be [[Differentiate|differentiated]] from other [[tumors]] causing small, round, blue cell [[tumors]] involving [[bone]] and [[soft tissue]], including [[lymphoma]], small cell [[osteosarcoma]], undifferentiated [[neuroblastoma]], desmoplastic small round cell tumors, mesenchymal [[chondrosarcoma]], [[rhabdomyosarcoma]], and poorly differentiated [[synovial]] [[sarcoma]].<ref name="pmid1848471">{{cite journal |vauthors=Ambros IM, Ambros PF, Strehl S, Kovar H, Gadner H, Salzer-Kuntschik M |title=MIC2 is a specific marker for Ewing's sarcoma and peripheral primitive neuroectodermal tumors. Evidence for a common histogenesis of Ewing's sarcoma and peripheral primitive neuroectodermal tumors from MIC2 expression and specific chromosome aberration |journal=Cancer |volume=67 |issue=7 |pages=1886–93 |date=April 1991 |pmid=1848471 |doi=10.1002/1097-0142(19910401)67:7<1886::aid-cncr2820670712>3.0.co;2-u |url=}}</ref> | *[[Histopathological|Histopathologically]], primitive neuroectodermal tumors should be [[Differentiate|differentiated]] from other [[tumors]] causing small, round, blue cell [[tumors]] involving [[bone]] and [[soft tissue]], including [[lymphoma]], small cell [[osteosarcoma]], undifferentiated [[neuroblastoma]], desmoplastic small round cell tumors, mesenchymal [[chondrosarcoma]], [[rhabdomyosarcoma]], and poorly differentiated [[synovial]] [[sarcoma]].<ref name="pmid1848471">{{cite journal |vauthors=Ambros IM, Ambros PF, Strehl S, Kovar H, Gadner H, Salzer-Kuntschik M |title=MIC2 is a specific marker for Ewing's sarcoma and peripheral primitive neuroectodermal tumors. Evidence for a common histogenesis of Ewing's sarcoma and peripheral primitive neuroectodermal tumors from MIC2 expression and specific chromosome aberration |journal=Cancer |volume=67 |issue=7 |pages=1886–93 |date=April 1991 |pmid=1848471 |doi=10.1002/1097-0142(19910401)67:7<1886::aid-cncr2820670712>3.0.co;2-u |url=}}</ref> | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*The | *The incidence of PNETs is from birth to 20 years of age approximately 0.29 per 100,000.<ref name="ViseeSoltner2005">{{cite journal|last1=Visee|first1=S|last2=Soltner|first2=C|last3=Rialland|first3=X|last4=Machet|first4=M C|last5=Loussouarn|first5=D|last6=Milinkevitch|first6=S|last7=Pasco-Papon|first7=A|last8=Mercier|first8=P|last9=Rousselet|first9=M C|title=Supratentorial primitive neuroectodermal tumours of the brain: multidirectional differentiation does not influence prognosis. A clinicopathological report of 18 patients|journal=Histopathology|volume=46|issue=4|year=2005|pages=403–412|issn=0309-0167|doi=10.1111/j.1365-2559.2005.02101.x}}</ref> | ||
*The [[prevalence]] of primitive neuroectodermal tumors remains unknown. | *The [[prevalence]] of primitive neuroectodermal tumors remains unknown. | ||
*PNETs are more common among children. | *PNETs are more common among children. | ||
| Line 36: | Line 36: | ||
*PNETs are more prevalent in Hispanic and white races. | *PNETs are more prevalent in Hispanic and white races. | ||
==Risk Factors== | ==Risk Factors== | ||
* | *The most potent risk factor in the development of PNET is prenatal exposure to [[alcohol]] prenatal.<ref name=":2">{{Cite journal|last=G R Bunin, J D Buckley, C P Boesel, L B Rorke and A T Meadows|first=|date=1994|title=Risk factors for astrocytic glioma and primitive neuroectodermal tumor of the brain in young children: a report from the Children's Cancer Group.|url=http://cebp.aacrjournals.org/content/3/3/197.full-text.pdf|journal=Cancer Epidemiol Biomarkers Prev.|volume=|pages=|via=}}</ref> | ||
*Children who had lived in farms for at least 1 year showed an increased risk for PNET. | *Children who had lived in farms for at least 1 year showed an increased risk for PNET. | ||
*Certain [[syndromes]] seem to play the role of a [[risk factor]] for PNETs including the following: | *Certain [[syndromes]] seem to play the role of a [[risk factor]] for PNETs including the following: | ||
| Line 51: | Line 51: | ||
*If left untreated, [[patients]] with primitive neuroectodermal tumors may develop [[metastases]].<ref>{{Cite journal|last=Smoll NR.|first=|date=2012|title=Relative survival of childhood and adult medulloblastomas and primitive neuroectodermal tumors (PNETs).|url=|journal=Cancer|volume=|pages=|via=}}</ref> | *If left untreated, [[patients]] with primitive neuroectodermal tumors may develop [[metastases]].<ref>{{Cite journal|last=Smoll NR.|first=|date=2012|title=Relative survival of childhood and adult medulloblastomas and primitive neuroectodermal tumors (PNETs).|url=|journal=Cancer|volume=|pages=|via=}}</ref> | ||
*Common [[complications]] of the primitive neuroectodermal tumor include [[increased intracranial pressure]], [[cranial nerve palsy]], and [[seizures]]. | *Common [[complications]] of the primitive neuroectodermal tumor include [[increased intracranial pressure]], [[cranial nerve palsy]], and [[seizures]]. | ||
*[[Prognosis]] is generally poor, and the 5-year [[survival rate]] of [[patients]] with PNET less than 35% in adults and 64% in children. | *[[Prognosis]] is generally poor, and the 5-year [[survival rate]] of [[patients]] with PNET less than 35% in adults and 64% in [[children]]. | ||
*[[Prognosis]] is better in adult patients. | *[[Prognosis]] is better in adult [[Patient|patients]]. | ||
*Features associated with favorable [[prognosis]] include early [[diagnosis]], combination treatment approach including [[tumor]] resection, [[chemotherapy]] and [[radiotherapy]], intratumoral [[calcification]], [[Ki-67 (Biology)|Ki-67]] <30%, elevated [[LDH]], [[tumor]] volume >100 cc, and [[axial]] location. | *Features associated with favorable [[prognosis]] include early [[diagnosis]], combination treatment approach including [[tumor]] resection, [[chemotherapy]] and [[radiotherapy]], intratumoral [[calcification]], [[Ki-67 (Biology)|Ki-67]] <30%, elevated [[LDH]], [[tumor]] volume >100 [[Mili litr|cc]], and [[axial]] location. | ||
== Diagnosis == | == Diagnosis == | ||
=== History and Symptoms === | === History and Symptoms === | ||
* The majority of [[patients]] with primitive neuroectodermal tumors remain [[asymptomatic]] for years.<ref name="pmid2776115">{{cite journal |vauthors=Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA |title=Extraosseous Ewing's sarcoma. A study of 42 cases |journal=Cancer |volume=64 |issue=7 |pages=1548–53 |date=October 1989 |pmid=2776115 |doi=10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w |url=}}</ref><ref name="pmid20959975">{{cite journal |vauthors=Li X, Zhang W, Song T, Sun C, Shen Y |title=Primitive neuroectodermal tumor arising in the abdominopelvic region: CT features and pathology characteristics |journal=Abdom Imaging |volume=36 |issue=5 |pages=590–5 |date=October 2011 |pmid=20959975 |doi=10.1007/s00261-010-9655-z |url=}}</ref> | * The majority of [[patients]] with primitive neuroectodermal tumors remain [[asymptomatic]] for years.<ref name="pmid2776115">{{cite journal |vauthors=Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA |title=Extraosseous Ewing's sarcoma. A study of 42 cases |journal=Cancer |volume=64 |issue=7 |pages=1548–53 |date=October 1989 |pmid=2776115 |doi=10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w |url=}}</ref><ref name="pmid20959975">{{cite journal |vauthors=Li X, Zhang W, Song T, Sun C, Shen Y |title=Primitive neuroectodermal tumor arising in the abdominopelvic region: CT features and pathology characteristics |journal=Abdom Imaging |volume=36 |issue=5 |pages=590–5 |date=October 2011 |pmid=20959975 |doi=10.1007/s00261-010-9655-z |url=}}</ref> | ||
*Clinical presentation of primitive neuroectodermal tumors is often non-specific and depend on the site of the [[tumor]]. | *[[Clinical]] presentation of primitive neuroectodermal tumors is often non-specific and depend on the site of the [[tumor]]. | ||
*Patients with PNETs may present with only constitutional [[symptoms]] such as [[fever]], severe [[pain]], and [[paresthesia]]. | *Patients with PNETs may present with only constitutional [[symptoms]] such as [[fever]], severe [[pain]], and [[paresthesia]]. | ||
*Other symptoms of primitive neuroectodermal tumor may include the following: | *Other [[Symptom|symptoms]] of primitive neuroectodermal tumor may include the following: | ||
**[[Morning headache]] | **[[Morning headache]] | ||
**[[Restlessness]] | **[[Restlessness]] | ||
**Recurrent [[vomiting]] | **Recurrent [[vomiting]] | ||
| Line 71: | Line 71: | ||
=== Physical Examination === | === Physical Examination === | ||
*Physical examination may be remarkable for [[papilledema]], [[strabismus]], [[nystagmus]], [[ataxia|imbalance]], motor [[weakness]], facial [[sensory loss]], third, fourth, and sixth [[cranial nerve palsies]], [[hemiplegia]], [[hepatosplenomegaly]], and [[lymphadenopathy|adenopathy]].<ref name="pmid2776115">{{cite journal |vauthors=Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA |title=Extraosseous Ewing's sarcoma. A study of 42 cases |journal=Cancer |volume=64 |issue=7 |pages=1548–53 |date=October 1989 |pmid=2776115 |doi=10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w |url=}}</ref> | *[[Physical examination]] may be remarkable for [[papilledema]], [[strabismus]], [[nystagmus]], [[ataxia|imbalance]], motor [[weakness]], facial [[sensory loss]], third, fourth, and sixth [[cranial nerve palsies]], [[hemiplegia]], [[hepatosplenomegaly]], and [[lymphadenopathy|adenopathy]].<ref name="pmid2776115">{{cite journal |vauthors=Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA |title=Extraosseous Ewing's sarcoma. A study of 42 cases |journal=Cancer |volume=64 |issue=7 |pages=1548–53 |date=October 1989 |pmid=2776115 |doi=10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w |url=}}</ref> | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
*Laboratory findings | *[[Laboratory]] findings consistent with the [[diagnosis]] of primitive neuroectodermal tumor include elevated [[erythrocyte sedimentation rate]], positive [[C-reactive protein]], [[anemia]], [[leukocytosis]], [[thrombocytosis]], [[hypoalbuminemia]], increased [[Lactate dehydrogenase|LDH]] levels.<ref name="pmid3992134">{{cite journal |vauthors=Bacci G, Capanna R, Orlandi M, Mancini I, Bettelli G, Dallari D, Campanacci M |title=Prognostic significance of serum lactic acid dehydrogenase in Ewing's tumor of bone |journal=Ric Clin Lab |volume=15 |issue=1 |pages=89–96 |date=1985 |pmid=3992134 |doi= |url=}}</ref> | ||
*[[Neuroblastoma]] may be associated with an elevated level of [[urinary]] [[catecholamines]].<ref name="pmid16732582">{{cite journal |vauthors=Strenger V, Kerbl R, Dornbusch HJ, Ladenstein R, Ambros PF, Ambros IM, Urban C |title=Diagnostic and prognostic impact of urinary catecholamines in neuroblastoma patients |journal=Pediatr Blood Cancer |volume=48 |issue=5 |pages=504–9 |date=May 2007 |pmid=16732582 |doi=10.1002/pbc.20888 |url=}}</ref> | *[[Neuroblastoma]] may be associated with an elevated level of [[urinary]] [[catecholamines]].<ref name="pmid16732582">{{cite journal |vauthors=Strenger V, Kerbl R, Dornbusch HJ, Ladenstein R, Ambros PF, Ambros IM, Urban C |title=Diagnostic and prognostic impact of urinary catecholamines in neuroblastoma patients |journal=Pediatr Blood Cancer |volume=48 |issue=5 |pages=504–9 |date=May 2007 |pmid=16732582 |doi=10.1002/pbc.20888 |url=}}</ref> | ||
| Line 97: | Line 97: | ||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*There is no | *There is no treatment for PNET. | ||
*Chemotherapy is controversial in the treatment of PNET. | *[[Chemotherapy]] is controversial in the treatment of PNET. | ||
*For the management of peripheral form of PNET, systemic [[chemotherapy]] has been associated with a better [[prognosis]] and is generally recommended.<ref name="AlonsoYi2017">{{cite journal|last1=Alonso|first1=Marta M.|last2=Yi|first2=Xiaoping|last3=Liu|first3=Wenguang|last4=Zhang|first4=Youming|last5=Xiao|first5=Desheng|last6=Yin|first6=Hongling|last7=Long|first7=Xueying|last8=Li|first8=Li|last9=Zai|first9=Hongyan|last10=Chen|first10=Minfeng|last11=Li|first11=Wenzheng|last12=Sun|first12=Lunquan|title=Radiological features of primitive neuroectodermal tumors in intra-abdominal and retroperitoneal regions: A series of 18 cases|journal=PLOS ONE|volume=12|issue=3|year=2017|pages=e0173536|issn=1932-6203|doi=10.1371/journal.pone.0173536}}</ref> | *For the management of peripheral form of PNET, [[systemic]] [[chemotherapy]] has been associated with a better [[prognosis]] and is generally recommended.<ref name="AlonsoYi2017">{{cite journal|last1=Alonso|first1=Marta M.|last2=Yi|first2=Xiaoping|last3=Liu|first3=Wenguang|last4=Zhang|first4=Youming|last5=Xiao|first5=Desheng|last6=Yin|first6=Hongling|last7=Long|first7=Xueying|last8=Li|first8=Li|last9=Zai|first9=Hongyan|last10=Chen|first10=Minfeng|last11=Li|first11=Wenzheng|last12=Sun|first12=Lunquan|title=Radiological features of primitive neuroectodermal tumors in intra-abdominal and retroperitoneal regions: A series of 18 cases|journal=PLOS ONE|volume=12|issue=3|year=2017|pages=e0173536|issn=1932-6203|doi=10.1371/journal.pone.0173536}}</ref> | ||
=== Surgery === | === Surgery === | ||
* | *The feasibility of surgery depends on the site of the [[tumor]], at diagnosis. Maximum resection must be performed. | ||
=== Primary Prevention === | === Primary Prevention === | ||
*There are no [[Primary prevention|primary preventive]] measures available for primitive neuroectodermal tumors. | *There are no [[Primary prevention|primary preventive]] measures available for primitive neuroectodermal tumors. | ||
Latest revision as of 17:02, 14 November 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Gertrude Djouka, M.D.[2], Maria Fernanda Villarreal, M.D. [3]
Synonyms and keywords: Primitive neuroectodermal tumors; PNET; CNS PNET; Askin tumor; Peripheral neuroepithelioma; Ependymoblastoma
Overview
Primitive neuroectodermal tumor (also known as "PNET") is a rare type of malignant tumor originating from neuroectoderm. Neuroectoderm is normally involved in the development of the nervous system. Apart from central nervous system (CNS), PNETs can involve other tissues originating from the neuroectoderm such as muscles and bones. PNET was first discovered by James Ewing, an American pathologist, in 1921. However, the term PNETs was more commonly described in 1973 by Hart and Earle. In fact, PNETs are members of the Ewing tumor family. Primitive neuroectodermal tumor are classified into 3 subtypes. Histopathologically, PNETs should be differentiated from other tumors causing small round blue cell tumors involving bone and soft tissue. PNETs are more common among children. Clinical presentation of primitive neuroectodermal tumors is often non-specific and depend on the site of the tumor. Physical examination may be remarkable for papilledema, strabismus, nystagmus, imbalance, motor weakness, facial sensory loss, third, fourth, and sixth cranial nerve palsies, hemiplegia, hepatosplenomegaly, and adenopathy. On CT, findings associated with the diagnosis of PNETs, may include a large irregular mass with heterogeneous contrast enhancement. On MRI, findings of the PNETs may include highly variable and can be hypo-intense to isointense, but usually, hypo-intense on T1-weighted images and high signal solid components on T2-weighted images. For the management of peripheral form of PNET, systemic chemotherapy has been associated with a better prognosis and is generally recommended.
Historical Perspective
- Primitive neuroectodermal tumor was first discovered by James Ewing, an American pathologist, in 1921.[1]
- In 1983 the term PNET was first used by Rorke to describe all undifferentiated CNS tumors with neuroepithelial origin, irrespective of their site.[2]
Classification
- Primitive neuroectodermal tumor may be classified into 3 sub-types:[3]
- Central primitive neuroectodermal tumors (PNETs) which include tumors of CNS origin.
- Peripheral primitive neuroectodermal tumors (pPNETs) which include tumors with soft tissue and bone origin. These tumors are also called Ewing family of tumors (EFTs) and classified into Ewing sarcoma, malignant peripheral primitive neuroectodermal tumors, Askin tumor, and less common tumors (eg, neuroectodermal tumor, ectomesenchymoma, peripheral medulloepithelioma).[4][5]
- Neuroblastoma which is derived from the autonomic nervous system.
Pathophysiology
- The pathogenesis of peripheral primitive neuroectodermal tumor is characterized by the chromosomal translocation t(11;22)(q24q12).[6][7]
- This translocation fuses the EWS gene on chromosome 22 with the FLI1 gene on chromosome 11.
- The EWS-FLI1 gene has been associated with the development of PNET involving the synthesis of adrenal pathway.
- On gross pathology, white, hemorrhagic and necrotic mass are characteristic of PNET.[8]
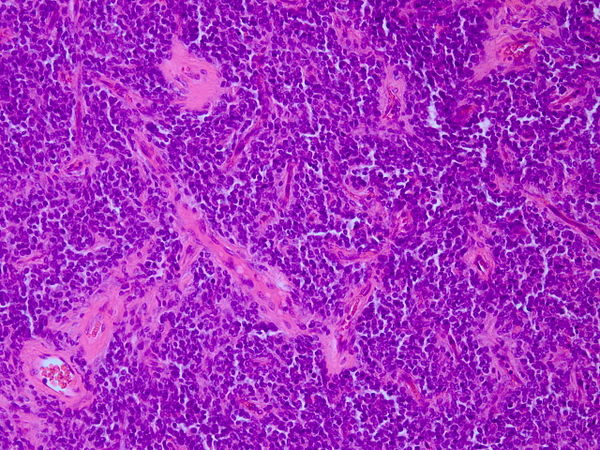 |
- On microscopic histopathological analysis, characteristic findings of the primitive neuroectodermal tumor, include small blue cell tumor with abundant mitotic figures, Homer-Wright rosettes, in which tumor cells surround neutrophils, fibrosis, and short and round or spindle-shaped nuclei.[9][10]
- Immunohistochemical analysis can also be positive for CD99, CD56, Neuron-specific enolase (NSE), S-100 protein, synaptophysin, and chromogranin A.[11]
Differentiating Primitive Neuroectodermal Tumor from Other Diseases
- Primitive neuroectodermal tumor must be differentiated from other diseases that cause seizures or an increase in intracranial pressure, such as astrocytoma, ependymoma, oligodendroglioma, intracranial teratoma, meningitis, encephalitis, and other brain tumors.
- Histopathologically, primitive neuroectodermal tumors should be differentiated from other tumors causing small, round, blue cell tumors involving bone and soft tissue, including lymphoma, small cell osteosarcoma, undifferentiated neuroblastoma, desmoplastic small round cell tumors, mesenchymal chondrosarcoma, rhabdomyosarcoma, and poorly differentiated synovial sarcoma.[12]
Epidemiology and Demographics
- The incidence of PNETs is from birth to 20 years of age approximately 0.29 per 100,000.[13]
- The prevalence of primitive neuroectodermal tumors remains unknown.
- PNETs are more common among children.
- PNETs are more prevalent in men than women.[14]
- PNETs are more prevalent in Hispanic and white races.
Risk Factors
- The most potent risk factor in the development of PNET is prenatal exposure to alcohol prenatal.[15]
- Children who had lived in farms for at least 1 year showed an increased risk for PNET.
- Certain syndromes seem to play the role of a risk factor for PNETs including the following:
Natural History, Complications and Prognosis
- If left untreated, patients with primitive neuroectodermal tumors may develop metastases.[16]
- Common complications of the primitive neuroectodermal tumor include increased intracranial pressure, cranial nerve palsy, and seizures.
- Prognosis is generally poor, and the 5-year survival rate of patients with PNET less than 35% in adults and 64% in children.
- Prognosis is better in adult patients.
- Features associated with favorable prognosis include early diagnosis, combination treatment approach including tumor resection, chemotherapy and radiotherapy, intratumoral calcification, Ki-67 <30%, elevated LDH, tumor volume >100 cc, and axial location.
Diagnosis
History and Symptoms
- The majority of patients with primitive neuroectodermal tumors remain asymptomatic for years.[17][18]
- Clinical presentation of primitive neuroectodermal tumors is often non-specific and depend on the site of the tumor.
- Patients with PNETs may present with only constitutional symptoms such as fever, severe pain, and paresthesia.
- Other symptoms of primitive neuroectodermal tumor may include the following:
- Morning headache
- Restlessness
- Recurrent vomiting
- Diplopia
- Frequent falls
- Positional dizziness
- Forgetfulness
- Progressive visual disturbances
Physical Examination
- Physical examination may be remarkable for papilledema, strabismus, nystagmus, imbalance, motor weakness, facial sensory loss, third, fourth, and sixth cranial nerve palsies, hemiplegia, hepatosplenomegaly, and adenopathy.[17]
Laboratory Findings
- Laboratory findings consistent with the diagnosis of primitive neuroectodermal tumor include elevated erythrocyte sedimentation rate, positive C-reactive protein, anemia, leukocytosis, thrombocytosis, hypoalbuminemia, increased LDH levels.[19]
- Neuroblastoma may be associated with an elevated level of urinary catecholamines.[20]
Electrocardiogram
- There are no ECG findings associated with primitive neuroectodermal tumors.
X-ray
- There are no x-ray findings associated with primitive neuroectodermal tumors.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with primitive neuroectodermal tumors.
CT
- On CT, findings associated with the diagnosis of primitive neuroectodermal tumor, may include a large irregular mass with heterogeneous contrast enhancement. Cystic components and calcification are also common.[21]
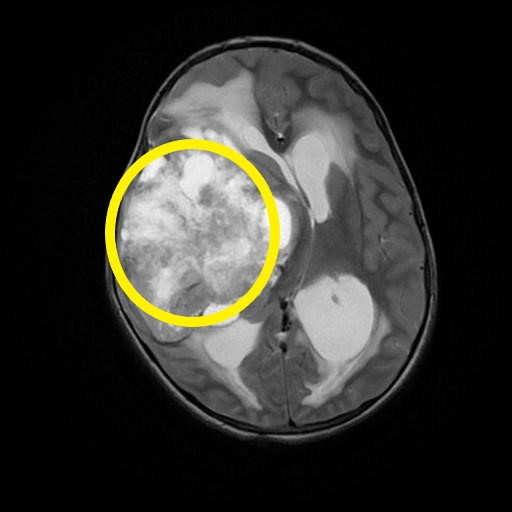 |
MRI
- MRI is the imaging modality of choice for primitive neuroectodermal tumors.[22]
- On MRI, findings of the primitive neuroectodermal tumor may include highly variable and can be hypo-intense to isointense, but usually, hypo-intense on T1-weighted images and high signal solid components on T2-weighted images.
Other Imaging Findings
- There are no other imaging findings associated with primitive neuroectodermal tumors.
Other Diagnostic Studies
- There are no other diagnostic studies associated with primitive neuroectodermal tumors.
Treatment
Medical Therapy
- There is no treatment for PNET.
- Chemotherapy is controversial in the treatment of PNET.
- For the management of peripheral form of PNET, systemic chemotherapy has been associated with a better prognosis and is generally recommended.[11]
Surgery
- The feasibility of surgery depends on the site of the tumor, at diagnosis. Maximum resection must be performed.
Primary Prevention
- There are no primary preventive measures available for primitive neuroectodermal tumors.
Secondary Prevention
- There are no secondary preventive measures available for primitive neuroectodermal tumors.
References
- ↑ Yagnik, Vipul D; Dawka, Sushil (2019). "
Extraskeletal Ewing's sarcoma/peripheral primitive neuroectodermal tumor of the small bowel presenting with gastrointestinal perforation
". Clinical and Experimental Gastroenterology. Volume 12: 279–285. doi:10.2147/CEG.S203697. ISSN 1178-7023. - ↑ Rorke LB. (1983). "The cerebellar medulloblastoma and its relationship to primitive neuroectodermal tumors". J Neuropathol Exp Neuro.
- ↑ Batsakis, John G.; MacKay, Bruce; El-Naggar, Adel K. (2016). "Ewing's Sarcoma and Peripheral Primitive Neuroectodermal Tumor: An Interim Report". Annals of Otology, Rhinology & Laryngology. 105 (10): 838–843. doi:10.1177/000348949610501014. ISSN 0003-4894.
- ↑ Castro, E. C.; Parwani, A. V. (2012). "Ewing Sarcoma/Primitive Neuroectodermal Tumor of the Kidney: Two Unusual Presentations of a Rare Tumor". Case Reports in Medicine. 2012: 1–7. doi:10.1155/2012/190581. ISSN 1687-9627.
- ↑ Triarico S, Attinà G, Maurizi P, Mastrangelo S, Nanni L, Briganti V, Meacci E, Margaritora S, Balducci M, Ruggiero A (July 2018). "Multimodal treatment of pediatric patients with Askin's tumors: our experience". World J Surg Oncol. 16 (1): 140. doi:10.1186/s12957-018-1434-2. PMC 6044084. PMID 30005673.
- ↑ Zucman J, Delattre O, Desmaze C, Plougastel B, Joubert I, Melot T; et al. (1992). "Cloning and characterization of the Ewing's sarcoma and peripheral neuroepithelioma t(11;22) translocation breakpoints". Genes Chromosomes Cancer. 5 (4): 271–7. PMID 1283315.
- ↑ Delattre O, Zucman J, Plougastel B, Desmaze C, Melot T, Peter M; et al. (1992). "Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours". Nature. 359 (6391): 162–5. doi:10.1038/359162a0. PMID 1522903.
- ↑ Novo J, Bitterman P, Guirguis A (2015). "Central-type primitive neuroectodermal tumor of the uterus: Case report of remission of stage IV disease using adjuvant cisplatin/etoposide/bevacizumab chemotherapy and review of the literature". Gynecol Oncol Rep. 14: 26–30. doi:10.1016/j.gore.2015.09.002. PMC 4688884. PMID 26793768.
- ↑ Jürgens HF (1994). "Ewing's sarcoma and peripheral primitive neuroectodermal tumor". Curr Opin Oncol. 6 (4): 391–6. PMID 7803540.
- ↑ de Alava E, Gerald WL (2000). "Molecular biology of the Ewing's sarcoma/primitive neuroectodermal tumor family". J Clin Oncol. 18 (1): 204–13. doi:10.1200/JCO.2000.18.1.204. PMID 10623711.
- ↑ 11.0 11.1 Alonso, Marta M.; Yi, Xiaoping; Liu, Wenguang; Zhang, Youming; Xiao, Desheng; Yin, Hongling; Long, Xueying; Li, Li; Zai, Hongyan; Chen, Minfeng; Li, Wenzheng; Sun, Lunquan (2017). "Radiological features of primitive neuroectodermal tumors in intra-abdominal and retroperitoneal regions: A series of 18 cases". PLOS ONE. 12 (3): e0173536. doi:10.1371/journal.pone.0173536. ISSN 1932-6203.
- ↑ Ambros IM, Ambros PF, Strehl S, Kovar H, Gadner H, Salzer-Kuntschik M (April 1991). "MIC2 is a specific marker for Ewing's sarcoma and peripheral primitive neuroectodermal tumors. Evidence for a common histogenesis of Ewing's sarcoma and peripheral primitive neuroectodermal tumors from MIC2 expression and specific chromosome aberration". Cancer. 67 (7): 1886–93. doi:10.1002/1097-0142(19910401)67:7<1886::aid-cncr2820670712>3.0.co;2-u. PMID 1848471.
- ↑ Visee, S; Soltner, C; Rialland, X; Machet, M C; Loussouarn, D; Milinkevitch, S; Pasco-Papon, A; Mercier, P; Rousselet, M C (2005). "Supratentorial primitive neuroectodermal tumours of the brain: multidirectional differentiation does not influence prognosis. A clinicopathological report of 18 patients". Histopathology. 46 (4): 403–412. doi:10.1111/j.1365-2559.2005.02101.x. ISSN 0309-0167.
- ↑ Ohba S, Yoshida K, Hirose Y, Ikeda E, Kawase T. (2008). "A supratentorial primitive neuroectodermal tumor in an adult: a case report and review of the literature". J Neurooncol.
- ↑ G R Bunin, J D Buckley, C P Boesel, L B Rorke and A T Meadows (1994). "Risk factors for astrocytic glioma and primitive neuroectodermal tumor of the brain in young children: a report from the Children's Cancer Group" (PDF). Cancer Epidemiol Biomarkers Prev.
- ↑ Smoll NR. (2012). "Relative survival of childhood and adult medulloblastomas and primitive neuroectodermal tumors (PNETs)". Cancer.
- ↑ 17.0 17.1 Rud NP, Reiman HM, Pritchard DJ, Frassica FJ, Smithson WA (October 1989). "Extraosseous Ewing's sarcoma. A study of 42 cases". Cancer. 64 (7): 1548–53. doi:10.1002/1097-0142(19891001)64:7<1548::aid-cncr2820640733>3.0.co;2-w. PMID 2776115.
- ↑ Li X, Zhang W, Song T, Sun C, Shen Y (October 2011). "Primitive neuroectodermal tumor arising in the abdominopelvic region: CT features and pathology characteristics". Abdom Imaging. 36 (5): 590–5. doi:10.1007/s00261-010-9655-z. PMID 20959975.
- ↑ Bacci G, Capanna R, Orlandi M, Mancini I, Bettelli G, Dallari D, Campanacci M (1985). "Prognostic significance of serum lactic acid dehydrogenase in Ewing's tumor of bone". Ric Clin Lab. 15 (1): 89–96. PMID 3992134.
- ↑ Strenger V, Kerbl R, Dornbusch HJ, Ladenstein R, Ambros PF, Ambros IM, Urban C (May 2007). "Diagnostic and prognostic impact of urinary catecholamines in neuroblastoma patients". Pediatr Blood Cancer. 48 (5): 504–9. doi:10.1002/pbc.20888. PMID 16732582.
- ↑ Xiao H, Bao F, Tan H, Wang B, Liu W, Gao J, Gao X (2016). "CT and clinical findings of peripheral primitive neuroectodermal tumour in children". Br J Radiol. 89 (1060): 20140450. doi:10.1259/bjr.20140450. PMC 4846188. PMID 26847997.
- ↑ Shi H, Kong X, Xu H, Xu L, Liu D (2004). "MRI features of intracranial primitive neuroectodermal tumors in adults: comparing with histopathological findings". J. Huazhong Univ. Sci. Technol. Med. Sci. 24 (1): 99–102. PMID 15165129.