Fungal meningitis laboratory findings: Difference between revisions
Ahmed Younes (talk | contribs) |
Ahmed Younes (talk | contribs) No edit summary |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} [[User:Rim Halaby|Rim Halaby]]; {{PTD}} | {{CMG}}; {{AE}} [[User:Rim Halaby|Rim Halaby]]; {{PTD}} | ||
==Overview== | ==Overview== | ||
A [[lumbar puncture]] is essential for the diagnosis of [[fungal meningitis]] and initiation of the appropriate treatment. The [[cerebrospinal fluid | A [[lumbar puncture]] is essential for the diagnosis of [[fungal meningitis]] and initiation of the appropriate treatment. The [[cerebrospinal fluid|cerebrospinal fluid (CSF)]] of a patient having [[fungal meningitis]] is distinguished by the presence of [[lymphocytosis]], [[Low blood sugar|low glucose level]] and high proteins level. Specific [[CSF]] stains and cultures as well as [[Serology|serologies]] help in determining the specific nature of the causative fungi. | ||
Biopsy of skin lesions, chest radiography, [[ophthalmologic]] examination, computed tomography or [[MRI]] of the brain, in addition to cultures of [[CSF]], blood, and [[sputum]], may provide essential diagnostic clues. | [[Biopsy]] of skin lesions, [[chest radiography]], [[ophthalmologic]] examination, [[computed tomography]] or [[MRI]] of the brain, in addition to cultures of [[CSF]], [[blood]], and [[sputum]], may provide essential diagnostic clues. | ||
==Laboratory Findings== | ==Laboratory Findings== | ||
| Line 10: | Line 10: | ||
Analysis of the [[CSF]] in suspected [[fungal meningitis]] should include:<ref name="pmid1569350">{{cite journal| author=White M, Cirrincione C, Blevins A, Armstrong D| title=Cryptococcal meningitis: outcome in patients with AIDS and patients with neoplastic disease. | journal=J Infect Dis | year= 1992 | volume= 165 | issue= 5 | pages= 960-3 | pmid=1569350 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1569350 }} </ref><ref name="pmid23083311">{{cite journal| author=Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC et al.| title=The index case for the fungal meningitis outbreak in the United States. | journal=N Engl J Med | year= 2012 | volume= 367 | issue= 22 | pages= 2119-25 | pmid=23083311 | doi=10.1056/NEJMoa1212292 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23083311 }} </ref><ref name="pmid11051295">{{cite journal| author=Gottfredsson M, Perfect JR| title=Fungal meningitis. | journal=Semin Neurol | year= 2000 | volume= 20 | issue= 3 | pages= 307-22 | pmid=11051295 | doi=10.1055/s-2000-9394 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11051295 }} </ref><ref name="pmid16291364">{{cite journal| author=Banarer M, Cost K, Rychwalski P, Bryant KA| title=Chronic lymphocytic meningitis in an adolescent. | journal=J Pediatr | year= 2005 | volume= 147 | issue= 5 | pages= 686-90 | pmid=16291364 | doi=10.1016/j.jpeds.2005.07.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16291364 }} </ref> | Analysis of the [[CSF]] in suspected [[fungal meningitis]] should include:<ref name="pmid1569350">{{cite journal| author=White M, Cirrincione C, Blevins A, Armstrong D| title=Cryptococcal meningitis: outcome in patients with AIDS and patients with neoplastic disease. | journal=J Infect Dis | year= 1992 | volume= 165 | issue= 5 | pages= 960-3 | pmid=1569350 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1569350 }} </ref><ref name="pmid23083311">{{cite journal| author=Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC et al.| title=The index case for the fungal meningitis outbreak in the United States. | journal=N Engl J Med | year= 2012 | volume= 367 | issue= 22 | pages= 2119-25 | pmid=23083311 | doi=10.1056/NEJMoa1212292 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23083311 }} </ref><ref name="pmid11051295">{{cite journal| author=Gottfredsson M, Perfect JR| title=Fungal meningitis. | journal=Semin Neurol | year= 2000 | volume= 20 | issue= 3 | pages= 307-22 | pmid=11051295 | doi=10.1055/s-2000-9394 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11051295 }} </ref><ref name="pmid16291364">{{cite journal| author=Banarer M, Cost K, Rychwalski P, Bryant KA| title=Chronic lymphocytic meningitis in an adolescent. | journal=J Pediatr | year= 2005 | volume= 147 | issue= 5 | pages= 686-90 | pmid=16291364 | doi=10.1016/j.jpeds.2005.07.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16291364 }} </ref> | ||
====Opening pressure measurement==== | |||
This has prognostic and therapeutic value especially in [[Cryptococcal Meningitis|cryptococcal]] meningitis although it is not commonly done or recorded. | This has prognostic and therapeutic value especially in [[Cryptococcal Meningitis|cryptococcal]] meningitis although it is not commonly done or recorded. | ||
====Cell count with differential==== | |||
Most patients have [[pleocytosis|mononuclear pleocytosis]] in the range of 20 to 500 cells/mm3 however some patients have [[Polymorphonuclear cells|polymorphonuclear]] [[neutrophils]] as the predominant cell type in caese of [[aspergillosis]] and | Most patients have [[pleocytosis|mononuclear pleocytosis]] in the range of 20 to 500 cells/mm3 however some patients have [[Polymorphonuclear cells|polymorphonuclear]] [[neutrophils]] as the predominant cell type in caese of [[aspergillosis]] and | ||
[[eosinophilia]] when [[Cryptococcus|Cryptococcus immitis]] is suspected<ref name="pmid1569350">{{cite journal| author=White M, Cirrincione C, Blevins A, Armstrong D| title=Cryptococcal meningitis: outcome in patients with AIDS and patients with neoplastic disease. | journal=J Infect Dis | year= 1992 | volume= 165 | issue= 5 | pages= 960-3 | pmid=1569350 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1569350 }} </ref><ref name="pmid23083311">{{cite journal| author=Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC et al.| title=The index case for the fungal meningitis outbreak in the United States. | journal=N Engl J Med | year= 2012 | volume= 367 | issue= 22 | pages= 2119-25 | pmid=23083311 | doi=10.1056/NEJMoa1212292 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23083311 }} </ref> | [[eosinophilia]] when [[Cryptococcus|Cryptococcus immitis]] is suspected<ref name="pmid1569350">{{cite journal| author=White M, Cirrincione C, Blevins A, Armstrong D| title=Cryptococcal meningitis: outcome in patients with AIDS and patients with neoplastic disease. | journal=J Infect Dis | year= 1992 | volume= 165 | issue= 5 | pages= 960-3 | pmid=1569350 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1569350 }} </ref><ref name="pmid23083311">{{cite journal| author=Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC et al.| title=The index case for the fungal meningitis outbreak in the United States. | journal=N Engl J Med | year= 2012 | volume= 367 | issue= 22 | pages= 2119-25 | pmid=23083311 | doi=10.1056/NEJMoa1212292 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23083311 }} </ref> | ||
In patients who are [[immunosuppressed]], the cell count may be markedly decreased to less than 20 cells/mm3. | In patients who are [[immunosuppressed]], the cell count may be markedly decreased to less than 20 cells/mm3. | ||
====Glucose concentration==== | |||
Glucose concentrations are usually decreased by may vary depending on the clinical state of the patient. | Glucose concentrations are usually decreased by may vary depending on the clinical state of the patient. | ||
====[[Protein]] concentrations==== | |||
[[Protein|CSF protein]] levels are usually increased | [[Protein|CSF protein]] levels are usually increased | ||
*[[Gram stain]] | *[[Gram stain]] | ||
* India ink | * India ink | ||
*Culture | *Culture | ||
===Other CSF Findings and Serology Tests Specific to Each Particular Fungi=== | ===Other CSF Findings and Serology Tests Specific to Each Particular Fungi=== | ||
*''[[Aspergillus]] | *''[[Aspergillus|Aspergillus spp]].'' | ||
**CSF culture may grow [[Aspergillus fumigatus]] complex or may be sterile<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | **CSF culture may grow [[Aspergillus fumigatus]] complex or may be [[sterile]]<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | ||
**Gomori-Grocott staining may | **Gomori-Grocott staining may reveal [[Hyphae|hyaline septate hyphae]]<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | ||
**Baseline serum and [[CSF]] 1,3-β-d-[[glucan]] (BDG) measurements are positive whereas serum and [[CSF]] [[galactomannan]] (GM) antigen test results are negative in an ''[[Aspergillus fumigatus]]''-specific [[PCR]] assay.<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | **Baseline serum and [[CSF]] 1,3-β-d-[[glucan]] (BDG) measurements are positive whereas serum and [[CSF]] [[galactomannan]] (GM) [[antigen]] test results are negative in an ''[[Aspergillus fumigatus]]''-specific [[PCR]] assay.<ref name="pmid26392507">{{cite journal| author=Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R et al.| title=Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole. | journal=Antimicrob Agents Chemother | year= 2015 | volume= 59 | issue= 12 | pages= 7857-61 | pmid=26392507 | doi=10.1128/AAC.01506-15 | pmc=4649149 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26392507 }} </ref> | ||
*''[[Blastomyces dermatitidis]]'' | *''[[Blastomyces dermatitidis]]'' | ||
**Fungal stain and culture of CSF | **Fungal stain and culture of CSF | ||
**Biopsy and culture of skin and lung lesions | **[[Biopsy]] and [[Culture media|culture]] of skin and lung lesions | ||
**Antibody detection in serum | **[[Antibody]] detection in serum | ||
*''[[Cryptococcus neoformans]]'' | *''[[Cryptococcus neoformans]]'' | ||
**India ink or fungal wet mount of [[CSF]] (budding yeast) | **India ink or fungal wet mount of [[CSF]] ([[Yeast|budding yeast]]) | ||
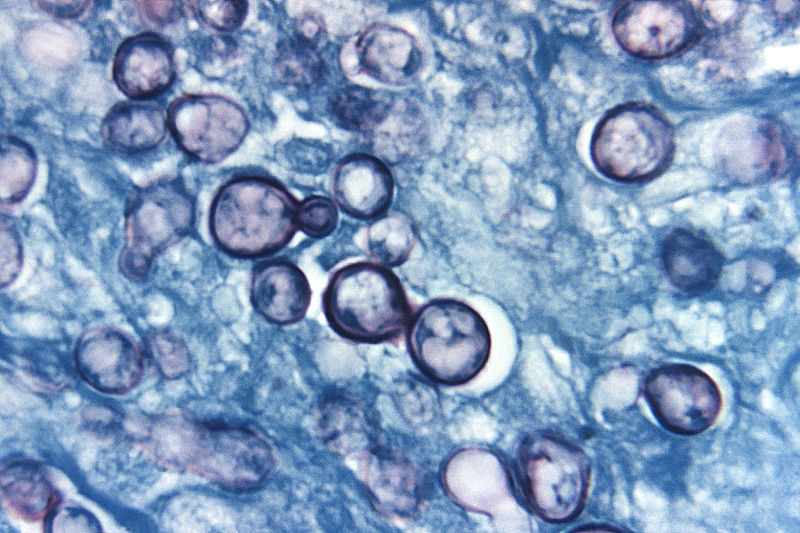
**[[Mucicarmine]] stain provides specific staining of the [[polysaccharide]] cell wall | **[[Mucicarmine]] stain provides specific staining of the [[polysaccharide]] cell wall | ||
**Blood and urine cultures | **[[Blood]] and [[urine]] cultures | ||
**Antigen detection in [[CSF]] | **[[Antigen]] detection in [[CSF]] | ||
*''[[Coccidioides immitis]]'' | *''[[Coccidioides immitis]]'' | ||
**Antibody detection in [[CSF]] and serum | **[[Antibody]] detection in [[CSF]] and [[serum]] | ||
*''[[Candida sp.]]'' | *''[[Candida|Candida sp.]]'' | ||
**Fungal stain and culture of [[CSF]] | **Fungal stain and culture of [[CSF]] | ||
*''[[Histoplasma capsulatum]]'' | *''[[Histoplasma capsulatum]]'' | ||
**Fungal stain and culture of large volumes of [[CSF]] | **Fungal stain and culture of large volumes of [[CSF]] | ||
**Antigen detection in [[CSF]], serum, and urine | **[[Antigen]] detection in [[CSF]], serum, and urine | ||
**Antibody detection in serum and [[CSF]] | **[[Antibody]] detection in serum and [[CSF]] | ||
*''[[Sporothrix schenckii]]'' | *''[[Sporothrix schenckii]]'' | ||
**Antibody detection in [[CSF]] and serum | **[[Antibody]] detection in [[CSF]] and serum | ||
**[[CSF]] culture<ref>Koroshetz WJ. Chapter 382. Chronic and Recurrent Meningitis. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.</ref> | **[[CSF]] culture<ref>Koroshetz WJ. Chapter 382. Chronic and Recurrent Meningitis. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.</ref> | ||
| Line 70: | Line 70: | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Cells''' | | style="padding: 5px 5px; background: #DCDCDC;" |'''Cells''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Lymphocyte]]:[[Monocyte]] 7:3''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Granulocyte]] > [[Lymphocyte]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Lymphocyte]] > [[Granulocyte]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''Lympho.> | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Lymphocyte|Lympho]].>[[Granulocyte]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''Lymphocytes''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Lymphocyte|Lymphocytes]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''Lymphocytes''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Lymphocyte|Lymphocytes]]''' | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Total protein (mg/dl''') | | style="padding: 5px 5px; background: #DCDCDC;" |'''Total [[protein]] (mg/dl''') | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''45-60''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''45-60''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''Typically 100-500''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''Typically 100-500''' | ||
| Line 85: | Line 85: | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''>50''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''>50''' | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Glucose ratio (CSF/plasma)<ref name="pmid24326618">{{cite journal| author=Chow E, Troy SB| title=The differential diagnosis of hypoglycorrhachia in adult patients. | journal=Am J Med Sci | year= 2014 | volume= 348 | issue= 3 | pages= 186-90 | pmid=24326618 | doi=10.1097/MAJ.0000000000000217 | pmc=4065645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24326618 }} </ref>''' | | style="padding: 5px 5px; background: #DCDCDC;" |'''[[Glucose]] ratio ([[CSF]]/[[Plasma|plasma)]]<ref name="pmid24326618">{{cite journal| author=Chow E, Troy SB| title=The differential diagnosis of hypoglycorrhachia in adult patients. | journal=Am J Med Sci | year= 2014 | volume= 348 | issue= 3 | pages= 186-90 | pmid=24326618 | doi=10.1097/MAJ.0000000000000217 | pmc=4065645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24326618 }} </ref>''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''> 0.5''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''> 0.5''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''< 0.3''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''< 0.3''' | ||
| Line 93: | Line 93: | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''<0.5''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''<0.5''' | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Lactate (mmols/l)<ref name="pmid22880096">{{cite journal| author=Leen WG, Willemsen MA, Wevers RA, Verbeek MM| title=Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice. | journal=PLoS One | year= 2012 | volume= 7 | issue= 8 | pages= e42745 | pmid=22880096 | doi=10.1371/journal.pone.0042745 | pmc=3412827 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22880096 }} </ref>''' | | style="padding: 5px 5px; background: #DCDCDC;" |'''[[Lactate]] (mmols/l)<ref name="pmid22880096">{{cite journal| author=Leen WG, Willemsen MA, Wevers RA, Verbeek MM| title=Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice. | journal=PLoS One | year= 2012 | volume= 7 | issue= 8 | pages= e42745 | pmid=22880096 | doi=10.1371/journal.pone.0042745 | pmc=3412827 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22880096 }} </ref>''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''< 2.1''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''< 2.1''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''> 2.1''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''> 2.1''' | ||
| Line 103: | Line 103: | ||
| style="padding: 5px 5px; background: #DCDCDC;" |'''Others''' | | style="padding: 5px 5px; background: #DCDCDC;" |'''Others''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''ICP:6-12 (cm H2O)''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''ICP:6-12 (cm H2O)''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''CSF gram stain, CSF culture, CSF bacterial antigen''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Gram stain|CSF gram stain]], [[Culture medium|CSF culture]], [[CSF]] [[Antigen|bacterial antigen]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''PCR of HSV-DNA, VZV''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[PCR]] of [[HSV|HSV-DNA]], [[VZV]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''CSF gram stain, CSF india ink''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[Gram stain|CSF gram stain]], CSF india ink''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''PCR of TBC-DNA''' | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[PCR]] of TBC-[[DNA]]''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" |'''CSF | | style="padding: 5px 5px; background: #F5F5F5;" |'''[[CSF]] [[tumor markers]] such as [[Alpha fetoprotein|alpha fetoproteins]], [[CEA]]''' | ||
|- | |- | ||
|} | |} | ||
===Nonspecific tests=== | ===Nonspecific tests=== | ||
| Line 116: | Line 115: | ||
===Fungal Stains=== | ===Fungal Stains=== | ||
<gallery> | <gallery> | ||
Blastomycosis.JPG|Blastomyces: Broad based budding | Blastomycosis.JPG|Blastomyces: Broad based budding - By Joel Mills - A feltöltő saját munkája, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=927183 | ||
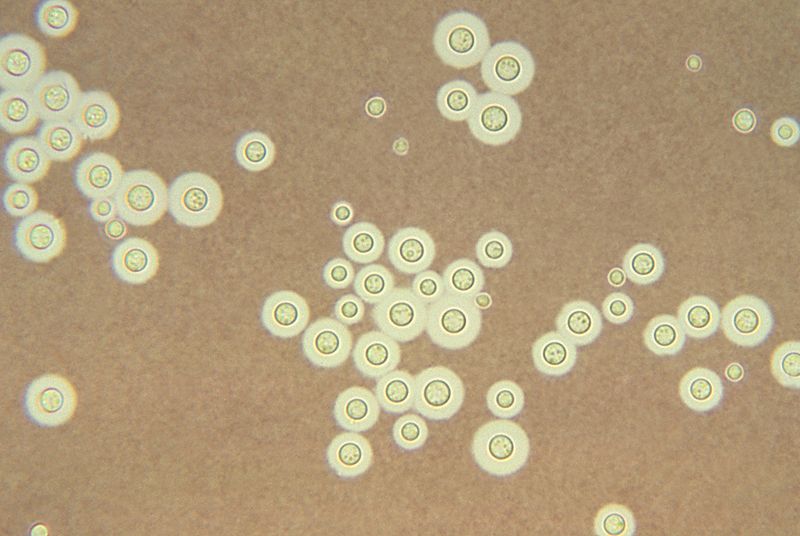
Cryptococcus_neoformans_India_ink_staining.jpg|Cryptococcus: clear halo visualized by the india ink stain | Cryptococcus_neoformans_India_ink_staining.jpg|Cryptococcus: clear halo visualized by the india ink stain - Source: https://www.cdc.gov/ | ||
Histoplasma_capsulatum.jpg|Histoplama capsulatum | Histoplasma_capsulatum.jpg|Histoplama capsulatum - Di Photo Credit:Content Providers(s): CDC/Dr. Libero Ajello - This media comes from the Centers for Disease Control and Prevention's Public Health Image Library (PHIL), with identification number #4221.Note: Not all PHIL images are public domain; be sure to check copyright status and credit authors and content providers.English | Slovenščina | +/−, Pubblico dominio, https://commons.wikimedia.org/w/index.php?curid=759394 | ||
</gallery> | </gallery> | ||
| Line 128: | Line 127: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 20:08, 21 September 2017
|
Fungal meningitis Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Fungal meningitis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Fungal meningitis laboratory findings |
|
Risk calculators and risk factors for Fungal meningitis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby; Prince Tano Djan, BSc, MBChB [2]
Overview
A lumbar puncture is essential for the diagnosis of fungal meningitis and initiation of the appropriate treatment. The cerebrospinal fluid (CSF) of a patient having fungal meningitis is distinguished by the presence of lymphocytosis, low glucose level and high proteins level. Specific CSF stains and cultures as well as serologies help in determining the specific nature of the causative fungi. Biopsy of skin lesions, chest radiography, ophthalmologic examination, computed tomography or MRI of the brain, in addition to cultures of CSF, blood, and sputum, may provide essential diagnostic clues.
Laboratory Findings
The General Characteristic CSF Findings in Fungal Meningitis:
Analysis of the CSF in suspected fungal meningitis should include:[1][2][3][4]
Opening pressure measurement
This has prognostic and therapeutic value especially in cryptococcal meningitis although it is not commonly done or recorded.
Cell count with differential
Most patients have mononuclear pleocytosis in the range of 20 to 500 cells/mm3 however some patients have polymorphonuclear neutrophils as the predominant cell type in caese of aspergillosis and eosinophilia when Cryptococcus immitis is suspected[1][2] In patients who are immunosuppressed, the cell count may be markedly decreased to less than 20 cells/mm3.
Glucose concentration
Glucose concentrations are usually decreased by may vary depending on the clinical state of the patient.
Protein concentrations
CSF protein levels are usually increased
- Gram stain
- India ink
- Culture
Other CSF Findings and Serology Tests Specific to Each Particular Fungi
- Aspergillus spp.
- CSF culture may grow Aspergillus fumigatus complex or may be sterile[5]
- Gomori-Grocott staining may reveal hyaline septate hyphae[5]
- Baseline serum and CSF 1,3-β-d-glucan (BDG) measurements are positive whereas serum and CSF galactomannan (GM) antigen test results are negative in an Aspergillus fumigatus-specific PCR assay.[5]
- Blastomyces dermatitidis
- Cryptococcus neoformans
- India ink or fungal wet mount of CSF (budding yeast)
- Mucicarmine stain provides specific staining of the polysaccharide cell wall
- Blood and urine cultures
- Antigen detection in CSF
- Coccidioides immitis
- Candida sp.
- Fungal stain and culture of CSF
- Histoplasma capsulatum
- Sporothrix schenckii
Laboratory findings differentiating fungal meningitis from other causes of meningitis by cerebrospinal fluid examination:[7][8][9][10][11]
| Cerebrospinal fluid level | Normal level | Bacterial meningitis[10] | Viral meningitis[10] | Fungal meningitis | Tuberculous meningitis[12] | Malignant meningitis[7] |
|---|---|---|---|---|---|---|
| Cells/ul | < 5 | >300 | 10-1000 | 10-500 | 50-500 | >4 |
| Cells | Lymphocyte:Monocyte 7:3 | Granulocyte > Lymphocyte | Lymphocyte > Granulocyte | Lympho.>Granulocyte | Lymphocytes | Lymphocytes |
| Total protein (mg/dl) | 45-60 | Typically 100-500 | Normal or slightly high | High | Typically 100-200 | >50 |
| Glucose ratio (CSF/plasma)[8] | > 0.5 | < 0.3 | > 0.6 | <0.3 | < 0.5 | <0.5 |
| Lactate (mmols/l)[9] | < 2.1 | > 2.1 | < 2.1 | >3.2 | > 2.1 | >2.1 |
| Others | ICP:6-12 (cm H2O) | CSF gram stain, CSF culture, CSF bacterial antigen | PCR of HSV-DNA, VZV | CSF gram stain, CSF india ink | PCR of TBC-DNA | CSF tumor markers such as alpha fetoproteins, CEA |
Nonspecific tests
Other nonspecific test example complete blood count, blood culture and electrolyte level may help in assessing the general picture of the patient.
Fungal Stains
-
Blastomyces: Broad based budding - By Joel Mills - A feltöltő saját munkája, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=927183
-
Cryptococcus: clear halo visualized by the india ink stain - Source: https://www.cdc.gov/
-
+/−, Pubblico dominio, https://commons.wikimedia.org/w/index.php?curid=759394
Cryptococcosis (PAS stain)
{{#ev:youtube|ZG0AcmtBLe4}}
References
- ↑ 1.0 1.1 White M, Cirrincione C, Blevins A, Armstrong D (1992). "Cryptococcal meningitis: outcome in patients with AIDS and patients with neoplastic disease". J Infect Dis. 165 (5): 960–3. PMID 1569350.
- ↑ 2.0 2.1 Pettit AC, Kropski JA, Castilho JL, Schmitz JE, Rauch CA, Mobley BC; et al. (2012). "The index case for the fungal meningitis outbreak in the United States". N Engl J Med. 367 (22): 2119–25. doi:10.1056/NEJMoa1212292. PMID 23083311.
- ↑ Gottfredsson M, Perfect JR (2000). "Fungal meningitis". Semin Neurol. 20 (3): 307–22. doi:10.1055/s-2000-9394. PMID 11051295.
- ↑ Banarer M, Cost K, Rychwalski P, Bryant KA (2005). "Chronic lymphocytic meningitis in an adolescent". J Pediatr. 147 (5): 686–90. doi:10.1016/j.jpeds.2005.07.010. PMID 16291364.
- ↑ 5.0 5.1 5.2 Morgand M, Rammaert B, Poirée S, Bougnoux ME, Tran H, Kania R; et al. (2015). "Chronic Invasive Aspergillus Sinusitis and Otitis with Meningeal Extension Successfully Treated with Voriconazole". Antimicrob Agents Chemother. 59 (12): 7857–61. doi:10.1128/AAC.01506-15. PMC 4649149. PMID 26392507.
- ↑ Koroshetz WJ. Chapter 382. Chronic and Recurrent Meningitis. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012.
- ↑ 7.0 7.1 Le Rhun E, Taillibert S, Chamberlain MC (2013). "Carcinomatous meningitis: Leptomeningeal metastases in solid tumors". Surg Neurol Int. 4 (Suppl 4): S265–88. doi:10.4103/2152-7806.111304. PMC 3656567. PMID 23717798.
- ↑ 8.0 8.1 Chow E, Troy SB (2014). "The differential diagnosis of hypoglycorrhachia in adult patients". Am J Med Sci. 348 (3): 186–90. doi:10.1097/MAJ.0000000000000217. PMC 4065645. PMID 24326618.
- ↑ 9.0 9.1 Leen WG, Willemsen MA, Wevers RA, Verbeek MM (2012). "Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice". PLoS One. 7 (8): e42745. doi:10.1371/journal.pone.0042745. PMC 3412827. PMID 22880096.
- ↑ 10.0 10.1 10.2 Negrini B, Kelleher KJ, Wald ER (2000). "Cerebrospinal fluid findings in aseptic versus bacterial meningitis". Pediatrics. 105 (2): 316–9. PMID 10654948.
- ↑ Brouwer MC, Tunkel AR, van de Beek D (2010). "Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis". Clin Microbiol Rev. 23 (3): 467–92. doi:10.1128/CMR.00070-09. PMC 2901656. PMID 20610819.
- ↑ Caudie C, Tholance Y, Quadrio I, Peysson S (2010). "[Contribution of CSF analysis to diagnosis and follow-up of tuberculous meningitis]". Ann Biol Clin (Paris). 68 (1): 107–11. doi:10.1684/abc.2010.0407. PMID 20146981.