Temsirolimus: Difference between revisions
No edit summary |
m (Protected "Temsirolimus": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
|authorTag={{Ammu}} | |authorTag={{Ammu}} | ||
|genericName=Temsirolimus | |genericName=Temsirolimus | ||
|aOrAn= | |aOrAn=an | ||
|drugClass=antineoplastic | |drugClass=[[antineoplastic agent]] | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=advanced renal cell carcinoma | |indication=advanced [[renal cell carcinoma]] | ||
|adverseReactions=edema, rash, hyperglycemia, hyperlipidemia , hypertriglyceridemia ,hypophosphatemia, inflammatory disease of mucous membrane , loss of appetite , nausea, decreased hemoglobin , decreased lymphocyte count, decreased platelet count, leukopenia, neutropenia, alkaline phosphatase raised, AST/SGOT level raised, asthenia , serum creatinine raised | |adverseReactions=[[edema]], [[rash]], [[hyperglycemia]], [[hyperlipidemia]], [[hypertriglyceridemia]], [[hypophosphatemia]], inflammatory disease of mucous membrane, loss of appetite, [[nausea]], decreased [[hemoglobin]], decreased [[lymphocyte]] count, decreased [[platelet]] count, [[leukopenia]], [[neutropenia]], [[alkaline phosphatase]] raised, [[AST]]/[[SGOT]] level raised, [[asthenia]], serum [[creatinine]] raised | ||
|blackBoxWarningTitle=<span style="color:#FF0000;">ConditionName: </span> | |blackBoxWarningTitle=<span style="color:#FF0000;">ConditionName: </span> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | |blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | ||
| Line 15: | Line 15: | ||
<!--FDA-Labeled Indications and Dosage (Adult)--> | <!--FDA-Labeled Indications and Dosage (Adult)--> | ||
|fdaLIADAdult=* | |fdaLIADAdult=* Temsirolimus is indicated for the treatment of advanced renal cell carcinoma. | ||
=====Advanced Renal Cell Carcinoma===== | =====Advanced Renal Cell Carcinoma===== | ||
* The recommended dose of | * The recommended dose of Temsirolimus for advanced renal cell carcinoma is 25 mg infused over a 30 – 60 minute period once a week. | ||
* Treatment should continue until disease progression or unacceptable toxicity occurs. | * Treatment should continue until disease progression or unacceptable toxicity occurs. | ||
=====Premedication===== | =====Premedication===== | ||
* Patients should receive prophylactic intravenous diphenhydramine 25 to 50 mg (or similar antihistamine) approximately 30 minutes before the start of each dose of | * Patients should receive prophylactic intravenous diphenhydramine 25 to 50 mg (or similar antihistamine) approximately 30 minutes before the start of each dose of Temsirolimus. | ||
=====Dosage Interruption/Adjustment===== | =====Dosage Interruption/Adjustment===== | ||
* | * Temsirolimus should be held for absolute neutrophil count (ANC) <1,000/mm3, platelet count <75,000/mm3, or NCI CTCAE grade 3 or greater adverse reactions. Once toxicities have resolved to grade 2 or less, Temsirolimus may be restarted with the dose reduced by 5 mg/week to a dose no lower than 15 mg/week. | ||
=====Dose Modification Guidelines===== | =====Dose Modification Guidelines===== | ||
* Hepatic Impairment | * Hepatic Impairment | ||
:* Use caution when treating patients with hepatic impairment. If | :* Use caution when treating patients with hepatic impairment. If Temsirolimus must be given in patients with mild hepatic impairment (bilirubin >1 – 1.5×ULN or AST >ULN but bilirubin ≤ULN), reduce the dose of Temsirolimus to 15 mg/week. Temsirolimus is contraindicated in patients with bilirubin >1.5×ULN. | ||
* Concomitant Strong CYP3A4 Inhibitors | * Concomitant Strong [[CYP3A4]] Inhibitors | ||
:* The concomitant use of strong CYP3A4 inhibitors should be avoided (e.g. ketoconazole, itraconazole, clarithromycin, atazanavir, indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, and voriconazole). Grapefruit juice may also increase plasma concentrations of sirolimus (a major metabolite of temsirolimus) and should be avoided. If patients must be co-administered a strong CYP3A4 inhibitor, based on pharmacokinetic studies, a | :* The concomitant use of strong [[CYP3A4]] inhibitors should be avoided (e.g. [[ketoconazole]], [[itraconazole]], [[clarithromycin]], [[atazanavir]], [[indinavir]], [[nefazodone]], [[nelfinavir]], [[ritonavir]], [[saquinavir]], [[telithromycin]], and [[voriconazole]]). Grapefruit juice may also increase plasma concentrations of sirolimus (a major metabolite of temsirolimus) and should be avoided. If patients must be co-administered a strong [[CYP3A4]] inhibitor, based on pharmacokinetic studies, a Temsirolimus dose reduction to 12.5 mg/week should be considered. This dose of Temsirolimus is predicted to adjust the AUC to the range observed without inhibitors. However, there are no clinical data with this dose adjustment in patients receiving strong [[CYP3A4]] inhibitors. If the strong inhibitor is discontinued, a washout period of approximately 1 week should be allowed before the Temsirolimus dose is adjusted back to the dose used prior to initiation of the strong [[CYP3A4]] inhibitor. | ||
* Concomitant Strong CYP3A4 Inducers | * Concomitant Strong [[CYP3A4]] Inducers | ||
:* The use of concomitant strong CYP3A4 inducers should be avoided (e.g. dexamethasone, phenytoin, carbamazepine, rifampin, rifabutin, | :* The use of concomitant strong [[CYP3A4]] inducers should be avoided (e.g. [[dexamethasone]], [[phenytoin]], [[carbamazepine]], [[rifampin]], [[rifabutin]], [[rifampicin]], [[phenobarbital]]). If patients must be co-administered a strong [[CYP3A4]] inducer, based on pharmacokinetic studies, a Temsirolimus dose increase from 25 mg/week up to 50 mg/week should be considered. This dose of Temsirolimus is predicted to adjust the AUC to the range observed without inducers. However, there are no clinical data with this dose adjustment in patients receiving strong [[CYP3A4]] inducers. If the strong inducer is discontinued the temsirolimus dose should be returned to the dose used prior to initiation of the strong [[CYP3A4]] inducer. | ||
=====Instructions for Preparation===== | =====Instructions for Preparation===== | ||
* | * Temsirolimus must be stored under refrigeration at 2°–8°C (36°–46°F) and protected from light. During handling and preparation of admixtures, Temsirolimus should be protected from excessive room light and sunlight. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. | ||
* In order to minimize the patient exposure to the plasticizer DEHP (di-2-ethylhexyl phthalate), which may be leached from PVC infusion bags or sets, the final | * In order to minimize the patient exposure to the plasticizer DEHP (di-2-ethylhexyl phthalate), which may be leached from PVC infusion bags or sets, the final Temsirolimus dilution for infusion should be stored in bottles (glass, polypropylene) or plastic bags (polypropylene, polyolefin) and administered through polyethylene-lined administration sets. | ||
* | * Temsirolimus 25 mg/mL injection must be diluted with the supplied diluent before further dilution in 0.9% Sodium Chloride Injection, USP. | ||
* Please note that both the | * Please note that both the Temsirolimus injection and diluent vials contain an overfill to ensure the recommended volume can be withdrawn. | ||
* Follow this two-step dilution process in an aseptic manner. | * Follow this two-step dilution process in an aseptic manner. | ||
* Step 1 | * Step 1 | ||
:* DILUTION OF | :* DILUTION OF Temsirolimus INJECTION 25 MG/ML WITH SUPPLIED DILUENT | ||
:* Each Vial of | :* Each Vial of Temsirolimus (temsirolimus) must first be mixed with 1.8 mL of the enclosed diluent. The resultant solution contains 30 mg/3 mL (10 mg/mL). | ||
:* Mix well by inversion of the vial. Allow sufficient time for the air bubbles to subside. The solution should be clear to slightly turbid, colorless to light-yellow solution, essentially free from visual particulates. | :* Mix well by inversion of the vial. Allow sufficient time for the air bubbles to subside. The solution should be clear to slightly turbid, colorless to light-yellow solution, essentially free from visual particulates. | ||
:* The concentrate-diluent mixture is stable below 25°C for up to 24 hours. | :* The concentrate-diluent mixture is stable below 25°C for up to 24 hours. | ||
| Line 45: | Line 45: | ||
:* Withdraw precisely the required amount of concentrate-diluent mixture containing temsirolimus 10 mg/mL as prepared in Step 1 from the vial (i.e., 2.5 mL for a temsirolimus dose of 25 mg) and further dilute into an infusion bag containing 250 mL of 0.9% Sodium Chloride Injection, USP. | :* Withdraw precisely the required amount of concentrate-diluent mixture containing temsirolimus 10 mg/mL as prepared in Step 1 from the vial (i.e., 2.5 mL for a temsirolimus dose of 25 mg) and further dilute into an infusion bag containing 250 mL of 0.9% Sodium Chloride Injection, USP. | ||
Mix by inversion of the bag or bottle, avoiding excessive shaking, as this may cause foaming. | Mix by inversion of the bag or bottle, avoiding excessive shaking, as this may cause foaming. | ||
:* The resulting solution should be inspected visually for particulate matter and discoloration prior to administration. The admixture of | :* The resulting solution should be inspected visually for particulate matter and discoloration prior to administration. The admixture of Temsirolimus in 0.9% Sodium Chloride Injection, USP should be protected from excessive room light and sunlight. | ||
=====Administration===== | =====Administration===== | ||
* Administration of the final diluted solution should be completed within six hours from the time that | * Administration of the final diluted solution should be completed within six hours from the time that Temsirolimus is first added to 0.9% Solution Chloride Injection, USP. | ||
* | * Temsirolimus is infused over a 30- to 60-minute period once weekly. The use of an infusion pump is the preferred method of administration to ensure accurate delivery of the product. | ||
* Appropriate administration materials should be composed of glass, polyolefin, or polyethylene to avoid excessive loss of product and diethylhexylpthalate (DEHP) extraction. The administration materials should consist of non-DEHP, non-polyvinylchloride (PVC) tubing with appropriate filter. In the case when a PVC administration set has to be used, it should not contain DEHP. An in-line polyethersulfone filter with a pore size of not greater than 5 microns is recommended for administration to avoid the possibility of particles bigger than 5 microns being infused. | * Appropriate administration materials should be composed of glass, polyolefin, or polyethylene to avoid excessive loss of product and diethylhexylpthalate (DEHP) extraction. The administration materials should consist of non-DEHP, non-polyvinylchloride (PVC) tubing with appropriate filter. In the case when a PVC administration set has to be used, it should not contain DEHP. An in-line polyethersulfone filter with a pore size of not greater than 5 microns is recommended for administration to avoid the possibility of particles bigger than 5 microns being infused. | ||
* If the administration set available does not have an in-line filter incorporated, a polyethersulfone filter should be added at the set (i.e., an end-filter) before the admixture reaches the vein of the patient. Different end-filters can be used, ranging in filter pore size from 0.2 microns up to 5 microns. The use of both an in-line and end-filter is not recommended. | * If the administration set available does not have an in-line filter incorporated, a polyethersulfone filter should be added at the set (i.e., an end-filter) before the admixture reaches the vein of the patient. Different end-filters can be used, ranging in filter pore size from 0.2 microns up to 5 microns. The use of both an in-line and end-filter is not recommended. | ||
* | * Temsirolimus, when diluted, contains polysorbate 80, which is known to increase the rate of DEHP extraction from PVC. This should be considered during the preparation and administration of Temsirolimus, including storage time elapsed when in direct contact with PVC following constitution. | ||
=====Compatibilities and Incompatibilities===== | =====Compatibilities and Incompatibilities===== | ||
* Undiluted | * Undiluted Temsirolimus injection should not be added directly to aqueous infusion solutions. Direct addition of Temsirolimus injection to aqueous solutions will result in precipitation of drug. Always combine Temsirolimus injection with DILUENT for Temsirolimus before adding to infusion solutions. | ||
* It is recommended that | * It is recommended that Temsirolimus be administered in 0.9% Sodium Chloride Injection after combining with diluent. The stability of Temsirolimus in other infusion solutions has not been evaluated. Addition of other drugs or nutritional agents to admixtures of Temsirolimus in 0.9% Sodium Chloride Injection has not been evaluated and should be avoided. Temsirolimus is degraded by both acids and bases, and thus combinations of temsirolimus with agents capable of modifying solution pH should be avoided. | ||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | ||
| Line 65: | Line 65: | ||
<!--Contraindications--> | <!--Contraindications--> | ||
|contraindications=* | |contraindications=* Temsirolimus is contraindicated in patients with bilirubin >1.5×ULN | ||
|warnings======Hypersensitivity/Infusion Reactions===== | |warnings======Hypersensitivity/Infusion Reactions===== | ||
* Hypersensitivity/infusion reactions, including but not limited to flushing, chest pain, dyspnea, hypotension, apnea, loss of consciousness, hypersensitivity and anaphylaxis, have been associated with the administration of temsirolimus. | * [[Hypersensitivity]]/infusion reactions, including but not limited to flushing, chest pain, dyspnea, hypotension, apnea, loss of consciousness, hypersensitivity and [[anaphylaxis]], have been associated with the administration of temsirolimus. | ||
* These reactions can occur very early in the first infusion, but may also occur with subsequent infusions. Patients should be monitored throughout the infusion and appropriate supportive care should be available. Temsirolimus infusion should be interrupted in all patients with severe infusion reactions and appropriate medical therapy administered. | * These reactions can occur very early in the first infusion, but may also occur with subsequent infusions. Patients should be monitored throughout the infusion and appropriate supportive care should be available. Temsirolimus infusion should be interrupted in all patients with severe infusion reactions and appropriate medical therapy administered. | ||
* | * Temsirolimus should be used with caution in persons with known hypersensitivity to temsirolimus or its metabolites (including sirolimus), polysorbate 80, or to any other component (including the excipients) of Temsirolimus. | ||
* An H1 antihistamine should be administered to patients before the start of the intravenous temsirolimus infusion. | * An [[H1]] antihistamine should be administered to patients before the start of the intravenous temsirolimus infusion. Temsirolimus should be used with caution in patients with known hypersensitivity to an antihistamine, or patients who cannot receive an antihistamine for other medical reasons. | ||
* If a patient develops a hypersensitivity | * If a patient develops a [[hypersensitivity reactions]] during the Temsirolimus infusion, the infusion should be stopped and the patient should be observed for at least 30 to 60 minutes (depending on the severity of the reaction). At the discretion of the physician, treatment may be resumed with the administration of an [[H1]]-receptor antagonist (such as diphenhydramine), if not previously administered, and/or an [[H2]]-receptor antagonist (such as intravenous [[famotidine]] 20 mg or intravenous [[ranitidine]] 50 mg) approximately 30 minutes before restarting the Temsirolimus infusion. The infusion may then be resumed at a slower rate (up to 60 minutes). | ||
* A benefit-risk assessment should be done prior to the continuation of temsirolimus therapy in patients with severe or life-threatening reactions. | * A benefit-risk assessment should be done prior to the continuation of temsirolimus therapy in patients with severe or life-threatening reactions. | ||
=====Hepatic Impairment===== | =====Hepatic Impairment===== | ||
* The safety and pharmacokinetics of | * The safety and pharmacokinetics of Temsirolimus were evaluated in a dose escalation phase 1 study in 110 patients with normal or varying degrees of hepatic impairment. Patients with baseline bilirubin >1.5×ULN experienced greater toxicity than patients with baseline bilirubin ≤1.5×ULN when treated with Temsirolimus. The overall frequency of ≥ grade 3 adverse reactions and deaths, including deaths due to progressive disease, were greater in patients with baseline bilirubin >1.5×ULN due to increased risk of death. | ||
* Use caution when treating patients with mild hepatic impairment. Concentrations of temsirolimus and its metabolite sirolimus were increased in patients with elevated AST or bilirubin levels. If | * Use caution when treating patients with mild hepatic impairment. Concentrations of temsirolimus and its metabolite sirolimus were increased in patients with elevated AST or bilirubin levels. If Temsirolimus must be given in patients with mild hepatic impairment (bilirubin >1 – 1.5×ULN or AST >ULN but bilirubin ≤ULN), reduce the dose of Temsirolimus to 15 mg/week. | ||
=====Hyperglycemia/Glucose Intolerance===== | =====Hyperglycemia/Glucose Intolerance===== | ||
* The use of | * The use of Temsirolimus is likely to result in increases in serum glucose. In the phase 3 trial, 89% of patients receiving Temsirolimus had at least one elevated serum glucose while on treatment, and 26% of patients reported hyperglycemia as an adverse event. This may result in the need for an increase in the dose of, or initiation of, insulin and/or oral hypoglycemic agent therapy. Serum glucose should be tested before and during treatment with Temsirolimus. Patients should be advised to report excessive thirst or any increase in the volume or frequency of urination. | ||
=====Infections===== | =====Infections===== | ||
* The use of | * The use of Temsirolimus may result in immunosuppression. Patients should be carefully observed for the occurrence of infections, including opportunistic infections. | ||
* Pneumocystis jiroveci pneumonia (PJP), including fatalities, has been reported in patients who received temsirolimus. This may be associated with concomitant use of corticosteroids or other immunosuppressive agents. Prophylaxis of PJP should be considered when concomitant use of corticosteroids or other immunosuppressive agents are required. | * Pneumocystis jiroveci pneumonia (PJP), including fatalities, has been reported in patients who received temsirolimus. This may be associated with concomitant use of [[corticosteroids]] or other immunosuppressive agents. Prophylaxis of PJP should be considered when concomitant use of corticosteroids or other immunosuppressive agents are required. | ||
=====Interstitial Lung Disease===== | =====Interstitial Lung Disease===== | ||
* Cases of interstitial lung disease, some resulting in death, occurred in patients who received | * Cases of interstitial lung disease, some resulting in death, occurred in patients who received Temsirolimus. Some patients were asymptomatic, or had minimal symptoms, with infiltrates detected on computed tomography scan or chest radiograph. Others presented with symptoms such as dyspnea, cough, hypoxia, and fever. Some patients required discontinuation of Temsirolimus and/or treatment with corticosteroids and/or antibiotics, while some patients continued treatment without additional intervention. Patients should be advised to report promptly any new or worsening respiratory symptoms. | ||
* It is recommended that patients undergo baseline radiographic assessment by lung computed tomography scan or chest radiograph prior to the initiation of | * It is recommended that patients undergo baseline radiographic assessment by lung computed tomography scan or chest radiograph prior to the initiation of Temsirolimus therapy. Follow such assessments periodically, even in the absence of clinical respiratory symptoms. | ||
* It is recommended that patients be followed closely for occurrence of clinical respiratory symptoms. If clinically significant respiratory symptoms develop, consider withholding | * It is recommended that patients be followed closely for occurrence of clinical respiratory symptoms. If clinically significant respiratory symptoms develop, consider withholding Temsirolimus administration until after recovery of symptoms and improvement of radiographic findings related to pneumonitis. Empiric treatment with corticosteroids and/or antibiotics may be considered. Opportunistic infections such as PJP should be considered in the differential diagnosis. For patients who require use of [[corticosteroids]], prophylaxis of PJP may be considered. | ||
=====Hyperlipemia===== | =====Hyperlipemia===== | ||
* The use of | * The use of Temsirolimus is likely to result in increases in serum triglycerides and cholesterol. In the phase 3 trial, 87% of patients receiving Temsirolimus had at least one elevated serum cholesterol value and 83% had at least one elevated serum triglyceride value. This may require initiation, or increase in the dose, of lipid-lowering agents. Serum cholesterol and triglycerides should be tested before and during treatment with Temsirolimus. | ||
=====Bowel Perforation===== | =====Bowel Perforation===== | ||
* Cases of fatal bowel perforation occurred in patients who received | * Cases of fatal bowel perforation occurred in patients who received Temsirolimus. * These patients presented with fever, abdominal pain, metabolic acidosis, bloody stools, diarrhea, and/or acute abdomen. Patients should be advised to report promptly any new or worsening abdominal pain or blood in their stools. | ||
=====Renal Failure===== | =====Renal Failure===== | ||
* Cases of rapidly progressive and sometimes fatal acute renal failure not clearly related to disease progression occurred in patients who received | * Cases of rapidly progressive and sometimes fatal acute renal failure not clearly related to disease progression occurred in patients who received Temsirolimus. Some of these cases were not responsive to dialysis. | ||
=====Wound Healing Complications===== | =====Wound Healing Complications===== | ||
* Use of | * Use of Temsirolimus has been associated with abnormal wound healing. Therefore, caution should be exercised with the use of Temsirolimus in the perioperative period. | ||
=====Intracerebral Hemorrhage===== | =====Intracerebral Hemorrhage===== | ||
* Patients with central nervous system tumors (primary CNS tumor or metastases) and/or receiving anticoagulation therapy may be at an increased risk of developing intracerebral bleeding (including fatal outcomes) while receiving | * Patients with central nervous system tumors (primary CNS tumor or metastases) and/or receiving anticoagulation therapy may be at an increased risk of developing intracerebral bleeding (including fatal outcomes) while receiving Temsirolimus. | ||
=====Co-administration with Inducers or Inhibitors of CYP3A Metabolism===== | =====Co-administration with Inducers or Inhibitors of CYP3A Metabolism===== | ||
* Agents Inducing CYP3A Metabolism | * Agents Inducing CYP3A Metabolism | ||
:* Strong inducers of CYP3A4/5 such as dexamethasone, carbamazepine, phenytoin, phenobarbital, rifampin, rifabutin, and | :* Strong inducers of [[CYP3A4]]/5 such as [[dexamethasone]], [[carbamazepine]], [[phenytoin]], [[phenobarbital]], [[rifampin]], [[rifabutin]], and [[rifampicin]] may decrease exposure of the active metabolite, sirolimus. If alternative treatment cannot be administered, a dose adjustment should be considered. [[St. John's Wort]] may decrease Temsirolimus plasma concentrations unpredictably. Patients receiving Temsirolimus should not take [[St. John's Wort]] concomitantly. | ||
* Agents Inhibiting CYP3A Metabolism | * Agents Inhibiting CYP3A Metabolism | ||
:* Strong CYP3A4 inhibitors such as atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, and telithromycin may increase blood concentrations of the active metabolite sirolimus. If alternative treatments cannot be administered, a dose adjustment should be considered. | :* Strong [[CYP3A4]] inhibitors such as [[atazanavir]], [[clarithromycin]], [[indinavir]], [[itraconazole]], [[ketoconazole]], [[nefazodone]], [[nelfinavir]], [[ritonavir]], [[saquinavir]], and [[telithromycin]] may increase blood concentrations of the active metabolite sirolimus. If alternative treatments cannot be administered, a dose adjustment should be considered. | ||
=====Concomitant use of | =====Concomitant use of Temsirolimus with sunitinib===== | ||
* The combination of | * The combination of [[Temsirolimus]] and sunitinib resulted in dose-limiting toxicity. Dose-limiting toxicities (Grade 3/4 erythematous maculopapular rash, and gout/cellulitis requiring hospitalization) were observed in two out of three patients treated in the first cohort of a phase 1 study at doses of Temsirolimus 15 mg IV per week and sunitinib 25 mg oral per day (Days 1–28 followed by a 2-week rest). | ||
=====Vaccinations===== | =====Vaccinations===== | ||
* The use of live vaccines and close contact with those who have received live vaccines should be avoided during treatment with | * The use of live vaccines and close contact with those who have received live vaccines should be avoided during treatment with Temsirolimus. Examples of live vaccines are: intranasal influenza, measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid vaccines. | ||
=====Use in Pregnancy===== | =====Use in Pregnancy===== | ||
* There are no adequate and well-controlled studies of | * There are no adequate and well-controlled studies of Temsirolimus in pregnant women. However, based on its mechanism of action, Temsirolimus may cause fetal harm when administered to a pregnant woman. Temsirolimus administered daily as an oral formulation caused embryo-fetal and intrauterine toxicities in rats and rabbits at human sub-therapeutic exposures. | ||
* If this drug is used during pregnancy or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant throughout treatment and for 3 months after | * If this drug is used during pregnancy or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant throughout treatment and for 3 months after Temsirolimus therapy has stopped. | ||
* Men should be counseled regarding the effects of | * Men should be counseled regarding the effects of Temsirolimus on the fetus and sperm prior to starting treatment. Men with partners of childbearing potential should use reliable contraception throughout treatment and are recommended to continue this for 3 months after the last dose of Temsirolimus. | ||
=====Elderly Patients===== | =====Elderly Patients===== | ||
* Based on the results of a phase 3 study, elderly patients may be more likely to experience certain adverse reactions including diarrhea, edema, and pneumonia. | * Based on the results of a phase 3 study, elderly patients may be more likely to experience certain adverse reactions including diarrhea, edema, and pneumonia. | ||
=====Monitoring Laboratory Tests===== | =====Monitoring Laboratory Tests===== | ||
* In the randomized, phase 3 trial, complete blood counts (CBCs) were checked weekly, and chemistry panels were checked every two weeks. Laboratory monitoring for patients receiving | * In the randomized, phase 3 trial, complete blood counts (CBCs) were checked weekly, and chemistry panels were checked every two weeks. Laboratory monitoring for patients receiving Temsirolimus may need to be performed more or less frequently at the physician's discretion. | ||
|clinicalTrials=* Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice. | |clinicalTrials=* Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice. | ||
* In the phase 3 randomized, open-label study of interferon alfa (IFN-α) alone, | * In the phase 3 randomized, open-label study of interferon alfa ([[IFN-α]]) alone, Temsirolimus alone, and Temsirolimus and [[IFN-α]], a total of 616 patients were treated. Two hundred patients received [[IFN-α]] weekly, 208 received Temsirolimus 25 mg weekly, and 208 patients received a combination of Temsirolimus and [[IFN-α]] weekly. | ||
* Treatment with the combination of | * Treatment with the combination of Temsirolimus 15 mg and [[IFN-α]] was associated with an increased incidence of multiple adverse reactions and did not result in a significant increase in overall survival when compared with [[IFN-α]] alone. | ||
* Table 1 shows the percentage of patients experiencing treatment emergent adverse reactions. Reactions reported in at least 10% of patients who received | * Table 1 shows the percentage of patients experiencing treatment emergent adverse reactions. Reactions reported in at least 10% of patients who received Temsirolimus 25 mg alone or [[IFN-α]] alone are listed. Table 2 shows the percentage of patients experiencing selected laboratory abnormalities. Data for the same adverse reactions and laboratory abnormalities in the [[IFN-α]] alone arm are shown for comparison: | ||
: [[File:Tero 01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:Tero 01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
* Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice. | * Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice. | ||
* In the phase 3 randomized, open-label study of interferon alfa (IFN-α) alone, | * In the phase 3 randomized, open-label study of interferon alfa ([[IFN-α]]) alone, Temsirolimus alone, and Temsirolimus and [[IFN-α]], a total of 616 patients were treated. Two hundred patients received [[IFN-α]] weekly, 208 received Temsirolimus 25 mg weekly, and 208 patients received a combination of Temsirolimus and [[IFN-α]] weekly. | ||
* Treatment with the combination of | * Treatment with the combination of Temsirolimus 15 mg and [[IFN-α]] was associated with an increased incidence of multiple adverse reactions and did not result in a significant increase in overall survival when compared with [[IFN-α]] alone. | ||
* Table 1 shows the percentage of patients experiencing treatment emergent adverse reactions. Reactions reported in at least 10% of patients who received | * Table 1 shows the percentage of patients experiencing treatment emergent adverse reactions. Reactions reported in at least 10% of patients who received Temsirolimus 25 mg alone or [[IFN-α]] alone are listed. Table 2 shows the percentage of patients experiencing selected laboratory abnormalities. Data for the same adverse reactions and laboratory abnormalities in the [[IFN-α]] alone arm are shown for comparison: | ||
: [[File:Tero 02.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:Tero 02.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
|postmarketing=* The following adverse reactions have been identified during post approval use of | |postmarketing=* The following adverse reactions have been identified during post approval use of Temsirolimus. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to readily estimate their frequency or establish a causal relationship to drug exposure. | ||
* The following adverse reactions have been observed in patients receiving temsirolimus: rhabdomyolysis, Stevens-Johnson Syndrome, and complex regional pain syndrome (reflex sympathetic dystrophy). | * The following adverse reactions have been observed in patients receiving temsirolimus: [[rhabdomyolysis]], [[Stevens-Johnson Syndrome]], and complex regional pain syndrome (reflex sympathetic dystrophy). | ||
* There are also post-marketing reports of temsirolimus extravasations resulting in swelling, pain, warmth, and erythema. | * There are also post-marketing reports of temsirolimus extravasations resulting in swelling, pain, warmth, and erythema. | ||
|drugInteractions======Agents Inducing CYP3A Metabolism===== | |drugInteractions======Agents Inducing CYP3A Metabolism===== | ||
* Co-administration of | * Co-administration of Temsirolimus with rifampin, a potent [[CYP3A4]]/5 inducer, had no significant effect on temsirolimus Cmax (maximum concentration) and AUC (area under the concentration versus the time curve) after intravenous administration, but decreased sirolimus Cmax by 65% and AUC by 56% compared to Temsirolimus treatment alone. If alternative treatment cannot be administered, a dose adjustment should be considered. | ||
=====Agents Inhibiting CYP3A Metabolism===== | =====Agents Inhibiting CYP3A Metabolism===== | ||
* Co-administration of | * Co-administration of Temsirolimus with ketoconazole, a potent [[CYP3A4]] inhibitor, had no significant effect on temsirolimus Cmax or AUC; however, sirolimus AUC increased 3.1-fold, and Cmax increased 2.2-fold compared to Temsirolimus alone. If alternative treatment cannot be administered, a dose adjustment should be considered. | ||
=====Interactions with Drugs Metabolized by CYP2D6===== | =====Interactions with Drugs Metabolized by CYP2D6===== | ||
* The concentration of desipramine, a CYP2D6 substrate, was unaffected when 25 mg of | * The concentration of desipramine, a CYP2D6 substrate, was unaffected when 25 mg of Temsirolimus was co-administered. No clinically significant effect is anticipated when temsirolimus is co-administered with agents that are metabolized by CYP2D6 or [[CYP3A4]]. | ||
|FDAPregCat=D | |FDAPregCat=D | ||
|useInPregnancyFDA=* Women of childbearing potential should be advised to avoid becoming pregnant throughout treatment and for 3 months after | |useInPregnancyFDA=* Women of childbearing potential should be advised to avoid becoming pregnant throughout treatment and for 3 months after Temsirolimus therapy has stopped. | ||
* Temsirolimus can cause fetal harm when administered to a pregnant woman. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. | * Temsirolimus can cause fetal harm when administered to a pregnant woman. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. | ||
* Temsirolimus administered daily as an oral formulation caused embryo-fetal and intrauterine toxicities in rats and rabbits at human sub-therapeutic exposures. Embryo-fetal adverse effects in rats consisted of reduced fetal weight and reduced ossifications, and in rabbits included reduced fetal weight, omphalocele, bifurcated sternabrae, notched ribs, and incomplete ossifications. | * Temsirolimus administered daily as an oral formulation caused embryo-fetal and intrauterine toxicities in rats and rabbits at human sub-therapeutic exposures. Embryo-fetal adverse effects in rats consisted of reduced fetal weight and reduced ossifications, and in rabbits included reduced fetal weight, omphalocele, bifurcated sternabrae, notched ribs, and incomplete ossifications. | ||
| Line 140: | Line 140: | ||
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | ||
|useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | |useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | ||
|useInNursing=* It is not known whether | |useInNursing=* It is not known whether Temsirolimus is excreted into human milk, and due to the potential for tumorigenicity shown for sirolimus (active metabolite of Temsirolimus) in animal studies, a decision should be made whether to discontinue nursing or discontinue Temsirolimus, taking into account the importance of the drug to the mother. | ||
|useInPed=* Limited data are available on the use of temsirolimus in pediatric patients. The effectiveness of temsirolimus in pediatric patients with advanced recurrent/refractory solid tumors has not been established. | |useInPed=* Limited data are available on the use of temsirolimus in pediatric patients. The effectiveness of temsirolimus in pediatric patients with advanced recurrent/refractory solid tumors has not been established. | ||
* | * Temsirolimus was studied in 71 patients (59 patients ages 1 to 17 years and 12 patients ages 18 to 21 years) with relapsed/refractory solid tumors in a phase 1–2 safety and exploratory pharmacodynamic study. | ||
* In phase 1, 19 pediatric patients with advanced recurrent/refractory solid tumors received | * In phase 1, 19 pediatric patients with advanced recurrent/refractory solid tumors received Temsirolimus at doses ranging from 10 mg/m2 to 150 mg/m2 as a 60-minute intravenous infusion once weekly in three-week cycles. | ||
* In phase 2, 52 pediatric patients with recurrent/relapsed neuroblastoma, rhabdomyosarcoma, or high grade glioma received | * In phase 2, 52 pediatric patients with recurrent/relapsed neuroblastoma, rhabdomyosarcoma, or high grade glioma received Temsirolimus at a weekly dose of 75 mg/m2. One of 19 patients with neuroblastoma achieved a partial response. There were no objective responses in pediatric patients with recurrent/relapsed rhabdomyosarcoma or high grade glioma. | ||
* Adverse reactions associated with | * Adverse reactions associated with Temsirolimus were similar to those observed in adults. The most common adverse reactions (≥20%) in pediatric patients receiving the 75 mg/m2 dose included thrombocytopenia, infections, asthenia/fatigue, fever, pain, leukopenia, rash, anemia, hyperlipidemia, increased cough, stomatitis, anorexia, increased plasma levels of alanine aminotransferase and aspartate aminotransferase, hypercholesterolemia, hyperglycemia, abdominal pain, headache, arthralgia, upper respiratory infection, nausea and vomiting, neutropenia, hypokalemia, and hypophosphatemia. | ||
* Pharmacokinetics | * Pharmacokinetics | ||
:* In phase 1 of the above mentioned pediatric trial, the single dose and multiple dose total systemic exposure (AUC) of temsirolimus and sirolimus were less than dose-proportional over the dose range of 10 to 150 mg/m2. | :* In phase 1 of the above mentioned pediatric trial, the single dose and multiple dose total systemic exposure (AUC) of temsirolimus and sirolimus were less than dose-proportional over the dose range of 10 to 150 mg/m2. | ||
:* In the phase 2 portion, the multiple dose (Day 1, Cycle 2) pharmacokinetics of | :* In the phase 2 portion, the multiple dose (Day 1, Cycle 2) pharmacokinetics of Temsirolimus 75 mg/m2 were characterized in an additional 35 patients ages 28 days to 21 years (median age of 8 years). The geometric mean body surface adjusted clearance of temsirolimus and sirolimus was 9.45 L/h/m2 and 9.26 L/h/m2, respectively. The mean elimination half-life of temsirolimus and sirolimus was 31 hours and 44 hours, respectively. | ||
:* The exposure (AUCss) to temsirolimus and sirolimus was approximately 6-fold and 2-fold higher, respectively than the exposure in adult patients receiving a 25 mg intravenous infusion. | :* The exposure (AUCss) to temsirolimus and sirolimus was approximately 6-fold and 2-fold higher, respectively than the exposure in adult patients receiving a 25 mg intravenous infusion. | ||
|useInGeri=* Clinical studies of | |useInGeri=* Clinical studies of Temsirolimus did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Based on the results of a phase 3 study, elderly patients may be more likely to experience certain adverse reactions including [[diarrhea]], [[edema]], and [[pneumonia]]. | ||
|useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | |useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | ||
|useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | |useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | ||
|useInRenalImpair=* No clinical studies were conducted with | |useInRenalImpair=* No clinical studies were conducted with Temsirolimus in patients with decreased renal function. Less than 5% of total radioactivity was excreted in the urine following a 25 mg intravenous dose of [14C]-labeled temsirolimus in healthy subjects. Renal impairment is not expected to markedly influence drug exposure, and no dosage adjustment of Temsirolimus is recommended in patients with renal impairment. | ||
* | * Temsirolimus has not been studied in patients undergoing hemodialysis. | ||
|useInHepaticImpair=* | |useInHepaticImpair=* Temsirolimus was evaluated in a dose escalation phase 1 study in 110 patients with normal or varying degrees of hepatic impairment as defined by AST and bilirubin levels and patients with liver transplant (Table 3). Patients with moderate and severe hepatic impairment had increased rates of adverse reactions and deaths, including deaths due to progressive disease, during the study (Table 3). | ||
: [[File:Tero 03.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:Tero 03.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
|useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | |useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | ||
| Line 164: | Line 164: | ||
* Intravenous | * Intravenous | ||
|monitoring=* Monitor for symptoms or radiographic changes of interstitial lung disease (ILD). If ILD is suspected, discontinue | |monitoring=* Monitor for symptoms or radiographic changes of interstitial lung disease (ILD). If ILD is suspected, discontinue Temsirolimus, and consider use of corticosteroids and/or antibiotics. | ||
* Monitor renal function at baseline and while on | * Monitor renal function at baseline and while on Temsirolimus. | ||
* In the randomized, phase 3 trial, complete blood counts (CBCs) were checked weekly, and chemistry panels were checked every two weeks. Laboratory monitoring for patients receiving | * In the randomized, phase 3 trial, complete blood counts (CBCs) were checked weekly, and chemistry panels were checked every two weeks. Laboratory monitoring for patients receiving Temsirolimus may need to be performed more or less frequently at the physician's discretion. | ||
|IVCompat=There is limited information regarding <i>IV Compatibility</i> of {{PAGENAME}} in the drug label. | |IVCompat=There is limited information regarding <i>IV Compatibility</i> of {{PAGENAME}} in the drug label. | ||
<!--Overdosage--> | <!--Overdosage--> | ||
|overdose=* There is no specific treatment for | |overdose=* There is no specific treatment for Temsirolimus intravenous overdose. Temsirolimus has been administered to patients with cancer in phase 1 and 2 trials with repeated intravenous doses as high as 220 mg/m2. The risk of several serious adverse events, including thrombosis, bowel perforation, interstitial lung disease (ILD), seizure, and psychosis, is increased with doses of Temsirolimus greater than 25 mg. | ||
|drugBox=<!-- | |drugBox={{Drugbox2 | ||
| Verifiedfields = changed | |||
| verifiedrevid = 409344559 | |||
| IUPAC_name = (1''R'',2''R'',4''S'')-4-{(2''R'')-2-[(3''S'',6''R'',7''E'',9''R'',10''R'',12''R'',14''S'',15''E'',17''E'',19''E'',21''S'',23''S'',26''R'',27''R'',34a''S'')-9,27-dihydroxy-10,21-dimethoxy-6,8,12,14,20,26-hexamethyl-1,5,11,28,29-pentaoxo-1,4,5,6,9,10,11,12,13,14,21,22,23,24,25,26,27,28,29,31,32,33,34,34a-tetracosahydro-3''H''-23,27-epoxypyrido[2,1-''c''][1,4]oxazacyclohentriacontin-3-yl]propyl}-2-methoxycyclohexyl 3-hydroxy-2-(hydroxymethyl)-2-methylpropanoate | |||
| image = Tero 05 Structure.png | |||
<!--Clinical data--> | |||
| tradename = Torisel | |||
| Drugs.com = {{drugs.com|monograph|temsirolimus}} | |||
| MedlinePlus = a607071 | |||
| licence_EU = Torisel | |||
| licence_US = Torisel | |||
| pregnancy_AU = D | |||
| pregnancy_US = D | |||
| pregnancy_category = | |||
| legal_AU = S4 | |||
| legal_CA = Rx-only | |||
| legal_UK = POM | |||
| legal_US = Rx-only | |||
| legal_status = | |||
| routes_of_administration = Intravenous | |||
<!--Pharmacokinetic data--> | |||
| bioavailability = | |||
| protein_bound = | |||
| metabolism = | |||
| elimination_half-life = | |||
| excretion = | |||
<!--Identifiers--> | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 162635-04-3 | |||
| ATC_prefix = L01 | |||
| ATC_suffix = XE09 | |||
| PubChem = 6918289 | |||
| DrugBank_Ref = {{drugbankcite|changed|drugbank}} | |||
| DrugBank = DB06287 | |||
| ChemSpiderID_Ref = {{chemspidercite|changed|chemspider}} | |||
| ChemSpiderID = 21468899 | |||
| UNII_Ref = {{fdacite|changed|FDA}} | |||
| UNII = 624KN6GM2T | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = D06068 | |||
| ChEMBL_Ref = {{ebicite|changed|EBI}} | |||
| ChEMBL = 1201182 | |||
<!--Chemical data--> | |||
| chemical_formula = | |||
| C=56 | H=87 | N=1 | O=16 | |||
| molecular_weight = 1030.28 | |||
}} | |||
|mechAction=* Temsirolimus is an inhibitor of mTOR (mammalian target of rapamycin). Temsirolimus binds to an intracellular protein (FKBP-12), and the protein-drug complex inhibits the activity of mTOR that controls cell division. Inhibition of mTOR activity resulted in a G1 growth arrest in treated tumor cells. When mTOR was inhibited, its ability to phosphorylate p70S6k and S6 ribosomal protein, which are downstream of mTOR in the PI3 kinase/AKT pathway was blocked. | |mechAction=* Temsirolimus is an inhibitor of mTOR (mammalian target of rapamycin). Temsirolimus binds to an intracellular protein (FKBP-12), and the protein-drug complex inhibits the activity of mTOR that controls cell division. Inhibition of mTOR activity resulted in a G1 growth arrest in treated tumor cells. When mTOR was inhibited, its ability to phosphorylate p70S6k and S6 ribosomal protein, which are downstream of mTOR in the PI3 kinase/AKT pathway was blocked. | ||
* In in vitro studies using renal cell carcinoma cell lines, temsirolimus inhibited the activity of mTOR and resulted in reduced levels of the hypoxia-inducible factors HIF-1 and HIF-2 alpha, and the vascular endothelial growth factor. | * In in vitro studies using renal cell carcinoma cell lines, temsirolimus inhibited the activity of mTOR and resulted in reduced levels of the hypoxia-inducible factors HIF-1 and HIF-2 alpha, and the vascular endothelial growth factor. | ||
| Line 178: | Line 228: | ||
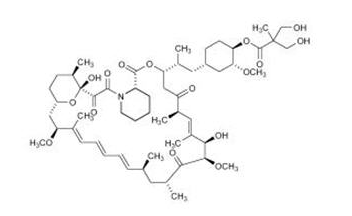
* The chemical name of temsirolimus is (3S,6R,7E,9R,10R,12R,14S,15E,17E,19E,21S,23S,26R,27R,34aS)-9,10,12,13,14,21,22,23,24,25,26,27,32,33,34,34a-Hexadecahydro-9,27-dihydroxy-3-[(1R)-2-[(1S,3R,4R)-4-hydroxy-3-methoxycyclohexyl]-1-methylethyl]-10,21-dimethoxy-6,8,12,14,20,26-hexamethyl-23, 27-epoxy-3H-pyrido[2,1-c][1,4]oxaazacyclohentriacontine-1,5,11,28,29(4H,6H,31H)-pentone 4'-[2,2-bis(hydroxymethyl)propionate]; or Rapamycin, 42-[3-hydroxy-2-(hydroxymethyl)-2-methylpropanoate]. | * The chemical name of temsirolimus is (3S,6R,7E,9R,10R,12R,14S,15E,17E,19E,21S,23S,26R,27R,34aS)-9,10,12,13,14,21,22,23,24,25,26,27,32,33,34,34a-Hexadecahydro-9,27-dihydroxy-3-[(1R)-2-[(1S,3R,4R)-4-hydroxy-3-methoxycyclohexyl]-1-methylethyl]-10,21-dimethoxy-6,8,12,14,20,26-hexamethyl-23, 27-epoxy-3H-pyrido[2,1-c][1,4]oxaazacyclohentriacontine-1,5,11,28,29(4H,6H,31H)-pentone 4'-[2,2-bis(hydroxymethyl)propionate]; or Rapamycin, 42-[3-hydroxy-2-(hydroxymethyl)-2-methylpropanoate]. | ||
: [[File:Tero 05 Structure.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:Tero 05 Structure.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
* | * Temsirolimus (temsirolimus) injection, 25 mg/mL, is a clear, colorless to light yellow, non-aqueous, ethanolic, sterile solution. Temsirolimus (temsirolimus) injection requires two dilutions prior to intravenous infusion. Temsirolimus (temsirolimus) injection should be diluted only with the supplied DILUENT for Temsirolimus®. | ||
* DILUENT for | * DILUENT for Temsirolimus® is a sterile, non-aqueous solution that is supplied with Temsirolimus injection, as a kit. | ||
* | * Temsirolimus (temsirolimus) injection, 25 mg/mL: | ||
* Active ingredient: temsirolimus (25 mg/mL) | * Active ingredient: temsirolimus (25 mg/mL) | ||
* Inactive ingredients: dehydrated alcohol (39.5% w/v), dl-alpha-tocopherol (0.075% w/v), propylene glycol (50.3% w/v), and anhydrous citric acid (0.0025% w/v). | * Inactive ingredients: dehydrated alcohol (39.5% w/v), dl-alpha-tocopherol (0.075% w/v), propylene glycol (50.3% w/v), and anhydrous citric acid (0.0025% w/v). | ||
=====DILUENT for | =====DILUENT for Temsirolimus®===== | ||
* Inactive ingredients | * Inactive ingredients | ||
:* Polysorbate 80 (40.0% w/v), polyethylene glycol 400 (42.8% w/v) and dehydrated alcohol (19.9% w/v). | :* Polysorbate 80 (40.0% w/v), polyethylene glycol 400 (42.8% w/v) and dehydrated alcohol (19.9% w/v). | ||
* After the | * After the Temsirolimus (temsirolimus) injection vial has been diluted with DILUENT for Temsirolimus®, in accordance with the instructions in section 2.5, the solution contains 35.2% alcohol. | ||
* | * Temsirolimus (temsirolimus) injection and DILUENT for Temsirolimus® are filled in clear glass vials with butyl rubber stoppers. | ||
<!--Pharmacodynamics--> | <!--Pharmacodynamics--> | ||
|PD=* Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for | |PD=* Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for Temsirolimus. In a randomized, single-blinded, crossover study, 58 healthy subjects received Temsirolimus 25 mg, placebo, and a single oral dose of moxifloxacin 400 mg. | ||
* A supratherapeutic | * A supratherapeutic Temsirolimus dose was not studied in this randomized QT trial. The largest difference between the upper bound 2-sided 90% CI for the mean difference between Temsirolimus and placebo-corrected QT interval was less than 10 ms. In a different trial in 69 patients with a hematologic malignancy, Temsirolimus doses up to 175 mg were studied. No patient with a normal QTcF at baseline had an increase in QTcF >60 ms. Additionally, there were no patients with a QTcF interval greater than 500 ms. | ||
|PK=* Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for | |PK=* Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for Temsirolimus. In a randomized, single-blinded, crossover study, 58 healthy subjects received Temsirolimus 25 mg, placebo, and a single oral dose of [[moxifloxacin]] 400 mg. | ||
* A supratherapeutic | * A supratherapeutic Temsirolimus dose was not studied in this randomized QT trial. The largest difference between the upper bound 2-sided 90% CI for the mean difference between Temsirolimus and placebo-corrected QT interval was less than 10 ms. In a different trial in 69 patients with a hematologic malignancy, Temsirolimus doses up to 175 mg were studied. No patient with a normal QTcF at baseline had an increase in QTcF >60 ms. Additionally, there were no patients with a QTcF interval greater than 500 ms. | ||
|nonClinToxic=* Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for | |nonClinToxic=* Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for Temsirolimus. In a randomized, single-blinded, crossover study, 58 healthy subjects received Temsirolimus 25 mg, placebo, and a single oral dose of moxifloxacin 400 mg. A supratherapeutic Temsirolimus dose was not studied in this randomized QT trial. | ||
* The largest difference between the upper bound 2-sided 90% CI for the mean difference between | * The largest difference between the upper bound 2-sided 90% CI for the mean difference between Temsirolimus and placebo-corrected QT interval was less than 10 ms. In a different trial in 69 patients with a hematologic malignancy, Temsirolimus doses up to 175 mg were studied. No patient with a normal QTcF at baseline had an increase in QTcF >60 ms. Additionally, there were no patients with a QTcF interval greater than 500 ms. | ||
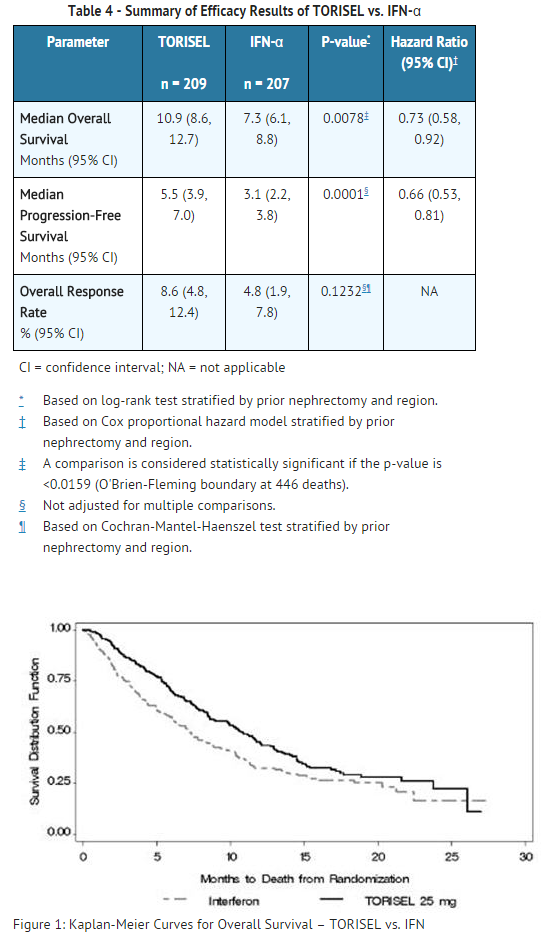
|clinicalStudies=* A phase 3, multi-center, three-arm, randomized, open-label study was conducted in previously untreated patients with advanced renal cell carcinoma (clear cell and non-clear cell histologies). The objectives were to compare Overall Survival (OS), Progression-Free Survival (PFS), Objective Response Rate (ORR), and safety in patients receiving IFN-α to those receiving | |clinicalStudies=* A phase 3, multi-center, three-arm, randomized, open-label study was conducted in previously untreated patients with advanced renal cell carcinoma (clear cell and non-clear cell histologies). The objectives were to compare Overall Survival (OS), Progression-Free Survival (PFS), Objective Response Rate (ORR), and safety in patients receiving [[IFN-α]] to those receiving Temsirolimus or Temsirolimus plus [[IFN-α]]. | ||
* Patients in this study had 3 or more of 6 pre-selected prognostic risk factors (less than one year from time of initial renal cell carcinoma diagnosis to randomization, Karnofsky performance status of 60 or 70, hemoglobin less than the lower limit of normal, corrected calcium of greater than 10 mg/dL, lactate dehydrogenase >1.5 times the upper limit of normal, more than one metastatic organ site). Patients were stratified for prior nephrectomy status within three geographic regions and were randomly assigned (1:1:1) to receive IFN-α alone (n = 207), | * Patients in this study had 3 or more of 6 pre-selected prognostic risk factors (less than one year from time of initial renal cell carcinoma diagnosis to randomization, Karnofsky performance status of 60 or 70, hemoglobin less than the lower limit of normal, corrected calcium of greater than 10 mg/dL, lactate dehydrogenase >1.5 times the upper limit of normal, more than one metastatic organ site). Patients were stratified for prior nephrectomy status within three geographic regions and were randomly assigned (1:1:1) to receive [[IFN-α]] alone (n = 207), Temsirolimus alone (25 mg weekly; n = 209), or the combination arm (n = 210). | ||
* The ITT population for this interim analysis included 626 patients. Demographics were comparable between the three treatment arms with regard to age, gender, and race. The mean age of all groups was 59 years (range 23–86). Sixty-nine percent were male and 31% were female. The racial distribution for all groups was 91% White, 4% Black, 2% Asian, and 3% other. Sixty-seven percent of patients had a history of prior nephrectomy. | * The ITT population for this interim analysis included 626 patients. Demographics were comparable between the three treatment arms with regard to age, gender, and race. The mean age of all groups was 59 years (range 23–86). Sixty-nine percent were male and 31% were female. The racial distribution for all groups was 91% White, 4% Black, 2% Asian, and 3% other. Sixty-seven percent of patients had a history of prior nephrectomy. | ||
* The median duration of treatment in the | * The median duration of treatment in the Temsirolimus arm was 17 weeks (range 1–126 weeks). The median duration of treatment on the IFN arm was 8 weeks (range 1–124 weeks). | ||
* There was a statistically significant improvement in OS (time from randomization to death) in the | * There was a statistically significant improvement in OS (time from randomization to death) in the Temsirolimus 25 mg arm compared to [[IFN-α]]. The combination of Temsirolimus 15 mg and [[IFN-α]] did not result in a significant increase in OS when compared with [[IFN-α]] alone. Figure 1 is a Kaplan-Meier plot of OS in this study. The evaluations of PFS (time from randomization to disease progression or death) and ORR, were based on blinded independent radiologic assessment of tumor response. Efficacy results are summarized in Table 4. | ||
: [[File:Tero 04 CS.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | : [[File:Tero 04 CS.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
|howSupplied=* NDC 0008-1179-01 | |howSupplied=* NDC 0008-1179-01 Temsirolimus® (temsirolimus) injection, 25 mg/mL. | ||
|storage=* Each kit is supplied in a single carton containing one single-use vial of 25 mg/mL of temsirolimus and one DILUENT vial which includes a deliverable volume of 1.8 mL, and must be stored at 2°–8° C (36°–46° F). Protect from light. | |storage=* Each kit is supplied in a single carton containing one single-use vial of 25 mg/mL of temsirolimus and one DILUENT vial which includes a deliverable volume of 1.8 mL, and must be stored at 2°–8° C (36°–46° F). Protect from light. | ||
|packLabel= | |packLabel=[[File:Tero06.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
[[File:Tero07.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
[[File:Tero08.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
[[File:Tero09.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
|fdaPatientInfo=* Each kit is supplied in a single carton containing one single-use vial of 25 mg/mL of temsirolimus and one DILUENT vial which includes a deliverable volume of 1.8 mL, and must be stored at 2°–8° C (36°–46° F). Protect from light. | |fdaPatientInfo=* Each kit is supplied in a single carton containing one single-use vial of 25 mg/mL of temsirolimus and one DILUENT vial which includes a deliverable volume of 1.8 mL, and must be stored at 2°–8° C (36°–46° F). Protect from light. | ||
|alcohol=* Alcohol-{{PAGENAME}} interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=* Alcohol-{{PAGENAME}} interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
<!--Brand Names--> | <!--Brand Names--> | ||
|brandNames=* | |brandNames=*Temsirolimus ®<ref>{{Cite web | title = Temsirolimus- temsirolimus | url =http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=95b7dc92-2180-42f1-8699-3c28f609e674#section-5.16 }}</ref> | ||
<!--Look-Alike Drug Names--> | <!--Look-Alike Drug Names--> | ||
|drugShortage= | |drugShortage= | ||
}} | }} | ||
| Line 227: | Line 277: | ||
{{LabelImage | {{LabelImage | ||
|fileName=Tero09.png | |fileName=Tero09.png | ||
}} | }} | ||
<!--Pill Image--> | <!--Pill Image--> | ||
<!--Label Display Image--> | <!--Label Display Image--> | ||
<!--Category--> | <!--Category--> | ||
[[Category:Drug]] | [[Category:Drug]] | ||
[[Category:Chemotherapeutic agents]] | |||
Latest revision as of 17:13, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Temsirolimus is an antineoplastic agent that is FDA approved for the treatment of advanced renal cell carcinoma. Common adverse reactions include edema, rash, hyperglycemia, hyperlipidemia, hypertriglyceridemia, hypophosphatemia, inflammatory disease of mucous membrane, loss of appetite, nausea, decreased hemoglobin, decreased lymphocyte count, decreased platelet count, leukopenia, neutropenia, alkaline phosphatase raised, AST/SGOT level raised, asthenia, serum creatinine raised.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Temsirolimus is indicated for the treatment of advanced renal cell carcinoma.
Advanced Renal Cell Carcinoma
- The recommended dose of Temsirolimus for advanced renal cell carcinoma is 25 mg infused over a 30 – 60 minute period once a week.
- Treatment should continue until disease progression or unacceptable toxicity occurs.
Premedication
- Patients should receive prophylactic intravenous diphenhydramine 25 to 50 mg (or similar antihistamine) approximately 30 minutes before the start of each dose of Temsirolimus.
Dosage Interruption/Adjustment
- Temsirolimus should be held for absolute neutrophil count (ANC) <1,000/mm3, platelet count <75,000/mm3, or NCI CTCAE grade 3 or greater adverse reactions. Once toxicities have resolved to grade 2 or less, Temsirolimus may be restarted with the dose reduced by 5 mg/week to a dose no lower than 15 mg/week.
Dose Modification Guidelines
- Hepatic Impairment
- Use caution when treating patients with hepatic impairment. If Temsirolimus must be given in patients with mild hepatic impairment (bilirubin >1 – 1.5×ULN or AST >ULN but bilirubin ≤ULN), reduce the dose of Temsirolimus to 15 mg/week. Temsirolimus is contraindicated in patients with bilirubin >1.5×ULN.
- Concomitant Strong CYP3A4 Inhibitors
- The concomitant use of strong CYP3A4 inhibitors should be avoided (e.g. ketoconazole, itraconazole, clarithromycin, atazanavir, indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, and voriconazole). Grapefruit juice may also increase plasma concentrations of sirolimus (a major metabolite of temsirolimus) and should be avoided. If patients must be co-administered a strong CYP3A4 inhibitor, based on pharmacokinetic studies, a Temsirolimus dose reduction to 12.5 mg/week should be considered. This dose of Temsirolimus is predicted to adjust the AUC to the range observed without inhibitors. However, there are no clinical data with this dose adjustment in patients receiving strong CYP3A4 inhibitors. If the strong inhibitor is discontinued, a washout period of approximately 1 week should be allowed before the Temsirolimus dose is adjusted back to the dose used prior to initiation of the strong CYP3A4 inhibitor.
- Concomitant Strong CYP3A4 Inducers
- The use of concomitant strong CYP3A4 inducers should be avoided (e.g. dexamethasone, phenytoin, carbamazepine, rifampin, rifabutin, rifampicin, phenobarbital). If patients must be co-administered a strong CYP3A4 inducer, based on pharmacokinetic studies, a Temsirolimus dose increase from 25 mg/week up to 50 mg/week should be considered. This dose of Temsirolimus is predicted to adjust the AUC to the range observed without inducers. However, there are no clinical data with this dose adjustment in patients receiving strong CYP3A4 inducers. If the strong inducer is discontinued the temsirolimus dose should be returned to the dose used prior to initiation of the strong CYP3A4 inducer.
Instructions for Preparation
- Temsirolimus must be stored under refrigeration at 2°–8°C (36°–46°F) and protected from light. During handling and preparation of admixtures, Temsirolimus should be protected from excessive room light and sunlight. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- In order to minimize the patient exposure to the plasticizer DEHP (di-2-ethylhexyl phthalate), which may be leached from PVC infusion bags or sets, the final Temsirolimus dilution for infusion should be stored in bottles (glass, polypropylene) or plastic bags (polypropylene, polyolefin) and administered through polyethylene-lined administration sets.
- Temsirolimus 25 mg/mL injection must be diluted with the supplied diluent before further dilution in 0.9% Sodium Chloride Injection, USP.
- Please note that both the Temsirolimus injection and diluent vials contain an overfill to ensure the recommended volume can be withdrawn.
- Follow this two-step dilution process in an aseptic manner.
- Step 1
- DILUTION OF Temsirolimus INJECTION 25 MG/ML WITH SUPPLIED DILUENT
- Each Vial of Temsirolimus (temsirolimus) must first be mixed with 1.8 mL of the enclosed diluent. The resultant solution contains 30 mg/3 mL (10 mg/mL).
- Mix well by inversion of the vial. Allow sufficient time for the air bubbles to subside. The solution should be clear to slightly turbid, colorless to light-yellow solution, essentially free from visual particulates.
- The concentrate-diluent mixture is stable below 25°C for up to 24 hours.
- Step 2
- DILUTION OF CONCENTRATE-DILUENT MIXTURE WITH 0.9% SODIUM CHLORIDE INJECTION, USP
- Withdraw precisely the required amount of concentrate-diluent mixture containing temsirolimus 10 mg/mL as prepared in Step 1 from the vial (i.e., 2.5 mL for a temsirolimus dose of 25 mg) and further dilute into an infusion bag containing 250 mL of 0.9% Sodium Chloride Injection, USP.
Mix by inversion of the bag or bottle, avoiding excessive shaking, as this may cause foaming.
- The resulting solution should be inspected visually for particulate matter and discoloration prior to administration. The admixture of Temsirolimus in 0.9% Sodium Chloride Injection, USP should be protected from excessive room light and sunlight.
Administration
- Administration of the final diluted solution should be completed within six hours from the time that Temsirolimus is first added to 0.9% Solution Chloride Injection, USP.
- Temsirolimus is infused over a 30- to 60-minute period once weekly. The use of an infusion pump is the preferred method of administration to ensure accurate delivery of the product.
- Appropriate administration materials should be composed of glass, polyolefin, or polyethylene to avoid excessive loss of product and diethylhexylpthalate (DEHP) extraction. The administration materials should consist of non-DEHP, non-polyvinylchloride (PVC) tubing with appropriate filter. In the case when a PVC administration set has to be used, it should not contain DEHP. An in-line polyethersulfone filter with a pore size of not greater than 5 microns is recommended for administration to avoid the possibility of particles bigger than 5 microns being infused.
- If the administration set available does not have an in-line filter incorporated, a polyethersulfone filter should be added at the set (i.e., an end-filter) before the admixture reaches the vein of the patient. Different end-filters can be used, ranging in filter pore size from 0.2 microns up to 5 microns. The use of both an in-line and end-filter is not recommended.
- Temsirolimus, when diluted, contains polysorbate 80, which is known to increase the rate of DEHP extraction from PVC. This should be considered during the preparation and administration of Temsirolimus, including storage time elapsed when in direct contact with PVC following constitution.
Compatibilities and Incompatibilities
- Undiluted Temsirolimus injection should not be added directly to aqueous infusion solutions. Direct addition of Temsirolimus injection to aqueous solutions will result in precipitation of drug. Always combine Temsirolimus injection with DILUENT for Temsirolimus before adding to infusion solutions.
- It is recommended that Temsirolimus be administered in 0.9% Sodium Chloride Injection after combining with diluent. The stability of Temsirolimus in other infusion solutions has not been evaluated. Addition of other drugs or nutritional agents to admixtures of Temsirolimus in 0.9% Sodium Chloride Injection has not been evaluated and should be avoided. Temsirolimus is degraded by both acids and bases, and thus combinations of temsirolimus with agents capable of modifying solution pH should be avoided.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Temsirolimus in adult patients.
Non–Guideline-Supported Use
- Mantle cell lymphoma, Relapsed or refractory [1]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Temsirolimus FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Temsirolimus in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Temsirolimus in pediatric patients.
Contraindications
- Temsirolimus is contraindicated in patients with bilirubin >1.5×ULN
Warnings
Hypersensitivity/Infusion Reactions
- Hypersensitivity/infusion reactions, including but not limited to flushing, chest pain, dyspnea, hypotension, apnea, loss of consciousness, hypersensitivity and anaphylaxis, have been associated with the administration of temsirolimus.
- These reactions can occur very early in the first infusion, but may also occur with subsequent infusions. Patients should be monitored throughout the infusion and appropriate supportive care should be available. Temsirolimus infusion should be interrupted in all patients with severe infusion reactions and appropriate medical therapy administered.
- Temsirolimus should be used with caution in persons with known hypersensitivity to temsirolimus or its metabolites (including sirolimus), polysorbate 80, or to any other component (including the excipients) of Temsirolimus.
- An H1 antihistamine should be administered to patients before the start of the intravenous temsirolimus infusion. Temsirolimus should be used with caution in patients with known hypersensitivity to an antihistamine, or patients who cannot receive an antihistamine for other medical reasons.
- If a patient develops a hypersensitivity reactions during the Temsirolimus infusion, the infusion should be stopped and the patient should be observed for at least 30 to 60 minutes (depending on the severity of the reaction). At the discretion of the physician, treatment may be resumed with the administration of an H1-receptor antagonist (such as diphenhydramine), if not previously administered, and/or an H2-receptor antagonist (such as intravenous famotidine 20 mg or intravenous ranitidine 50 mg) approximately 30 minutes before restarting the Temsirolimus infusion. The infusion may then be resumed at a slower rate (up to 60 minutes).
- A benefit-risk assessment should be done prior to the continuation of temsirolimus therapy in patients with severe or life-threatening reactions.
Hepatic Impairment
- The safety and pharmacokinetics of Temsirolimus were evaluated in a dose escalation phase 1 study in 110 patients with normal or varying degrees of hepatic impairment. Patients with baseline bilirubin >1.5×ULN experienced greater toxicity than patients with baseline bilirubin ≤1.5×ULN when treated with Temsirolimus. The overall frequency of ≥ grade 3 adverse reactions and deaths, including deaths due to progressive disease, were greater in patients with baseline bilirubin >1.5×ULN due to increased risk of death.
- Use caution when treating patients with mild hepatic impairment. Concentrations of temsirolimus and its metabolite sirolimus were increased in patients with elevated AST or bilirubin levels. If Temsirolimus must be given in patients with mild hepatic impairment (bilirubin >1 – 1.5×ULN or AST >ULN but bilirubin ≤ULN), reduce the dose of Temsirolimus to 15 mg/week.
Hyperglycemia/Glucose Intolerance
- The use of Temsirolimus is likely to result in increases in serum glucose. In the phase 3 trial, 89% of patients receiving Temsirolimus had at least one elevated serum glucose while on treatment, and 26% of patients reported hyperglycemia as an adverse event. This may result in the need for an increase in the dose of, or initiation of, insulin and/or oral hypoglycemic agent therapy. Serum glucose should be tested before and during treatment with Temsirolimus. Patients should be advised to report excessive thirst or any increase in the volume or frequency of urination.
Infections
- The use of Temsirolimus may result in immunosuppression. Patients should be carefully observed for the occurrence of infections, including opportunistic infections.
- Pneumocystis jiroveci pneumonia (PJP), including fatalities, has been reported in patients who received temsirolimus. This may be associated with concomitant use of corticosteroids or other immunosuppressive agents. Prophylaxis of PJP should be considered when concomitant use of corticosteroids or other immunosuppressive agents are required.
Interstitial Lung Disease
- Cases of interstitial lung disease, some resulting in death, occurred in patients who received Temsirolimus. Some patients were asymptomatic, or had minimal symptoms, with infiltrates detected on computed tomography scan or chest radiograph. Others presented with symptoms such as dyspnea, cough, hypoxia, and fever. Some patients required discontinuation of Temsirolimus and/or treatment with corticosteroids and/or antibiotics, while some patients continued treatment without additional intervention. Patients should be advised to report promptly any new or worsening respiratory symptoms.
- It is recommended that patients undergo baseline radiographic assessment by lung computed tomography scan or chest radiograph prior to the initiation of Temsirolimus therapy. Follow such assessments periodically, even in the absence of clinical respiratory symptoms.
- It is recommended that patients be followed closely for occurrence of clinical respiratory symptoms. If clinically significant respiratory symptoms develop, consider withholding Temsirolimus administration until after recovery of symptoms and improvement of radiographic findings related to pneumonitis. Empiric treatment with corticosteroids and/or antibiotics may be considered. Opportunistic infections such as PJP should be considered in the differential diagnosis. For patients who require use of corticosteroids, prophylaxis of PJP may be considered.
Hyperlipemia
- The use of Temsirolimus is likely to result in increases in serum triglycerides and cholesterol. In the phase 3 trial, 87% of patients receiving Temsirolimus had at least one elevated serum cholesterol value and 83% had at least one elevated serum triglyceride value. This may require initiation, or increase in the dose, of lipid-lowering agents. Serum cholesterol and triglycerides should be tested before and during treatment with Temsirolimus.
Bowel Perforation
- Cases of fatal bowel perforation occurred in patients who received Temsirolimus. * These patients presented with fever, abdominal pain, metabolic acidosis, bloody stools, diarrhea, and/or acute abdomen. Patients should be advised to report promptly any new or worsening abdominal pain or blood in their stools.
Renal Failure
- Cases of rapidly progressive and sometimes fatal acute renal failure not clearly related to disease progression occurred in patients who received Temsirolimus. Some of these cases were not responsive to dialysis.
Wound Healing Complications
- Use of Temsirolimus has been associated with abnormal wound healing. Therefore, caution should be exercised with the use of Temsirolimus in the perioperative period.
Intracerebral Hemorrhage
- Patients with central nervous system tumors (primary CNS tumor or metastases) and/or receiving anticoagulation therapy may be at an increased risk of developing intracerebral bleeding (including fatal outcomes) while receiving Temsirolimus.
Co-administration with Inducers or Inhibitors of CYP3A Metabolism
- Agents Inducing CYP3A Metabolism
- Strong inducers of CYP3A4/5 such as dexamethasone, carbamazepine, phenytoin, phenobarbital, rifampin, rifabutin, and rifampicin may decrease exposure of the active metabolite, sirolimus. If alternative treatment cannot be administered, a dose adjustment should be considered. St. John's Wort may decrease Temsirolimus plasma concentrations unpredictably. Patients receiving Temsirolimus should not take St. John's Wort concomitantly.
- Agents Inhibiting CYP3A Metabolism
- Strong CYP3A4 inhibitors such as atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, and telithromycin may increase blood concentrations of the active metabolite sirolimus. If alternative treatments cannot be administered, a dose adjustment should be considered.
Concomitant use of Temsirolimus with sunitinib
- The combination of Temsirolimus and sunitinib resulted in dose-limiting toxicity. Dose-limiting toxicities (Grade 3/4 erythematous maculopapular rash, and gout/cellulitis requiring hospitalization) were observed in two out of three patients treated in the first cohort of a phase 1 study at doses of Temsirolimus 15 mg IV per week and sunitinib 25 mg oral per day (Days 1–28 followed by a 2-week rest).
Vaccinations
- The use of live vaccines and close contact with those who have received live vaccines should be avoided during treatment with Temsirolimus. Examples of live vaccines are: intranasal influenza, measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid vaccines.
Use in Pregnancy
- There are no adequate and well-controlled studies of Temsirolimus in pregnant women. However, based on its mechanism of action, Temsirolimus may cause fetal harm when administered to a pregnant woman. Temsirolimus administered daily as an oral formulation caused embryo-fetal and intrauterine toxicities in rats and rabbits at human sub-therapeutic exposures.
- If this drug is used during pregnancy or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant throughout treatment and for 3 months after Temsirolimus therapy has stopped.
- Men should be counseled regarding the effects of Temsirolimus on the fetus and sperm prior to starting treatment. Men with partners of childbearing potential should use reliable contraception throughout treatment and are recommended to continue this for 3 months after the last dose of Temsirolimus.
Elderly Patients
- Based on the results of a phase 3 study, elderly patients may be more likely to experience certain adverse reactions including diarrhea, edema, and pneumonia.
Monitoring Laboratory Tests
- In the randomized, phase 3 trial, complete blood counts (CBCs) were checked weekly, and chemistry panels were checked every two weeks. Laboratory monitoring for patients receiving Temsirolimus may need to be performed more or less frequently at the physician's discretion.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice.
- In the phase 3 randomized, open-label study of interferon alfa (IFN-α) alone, Temsirolimus alone, and Temsirolimus and IFN-α, a total of 616 patients were treated. Two hundred patients received IFN-α weekly, 208 received Temsirolimus 25 mg weekly, and 208 patients received a combination of Temsirolimus and IFN-α weekly.
- Treatment with the combination of Temsirolimus 15 mg and IFN-α was associated with an increased incidence of multiple adverse reactions and did not result in a significant increase in overall survival when compared with IFN-α alone.
- Table 1 shows the percentage of patients experiencing treatment emergent adverse reactions. Reactions reported in at least 10% of patients who received Temsirolimus 25 mg alone or IFN-α alone are listed. Table 2 shows the percentage of patients experiencing selected laboratory abnormalities. Data for the same adverse reactions and laboratory abnormalities in the IFN-α alone arm are shown for comparison:
- Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice.
- In the phase 3 randomized, open-label study of interferon alfa (IFN-α) alone, Temsirolimus alone, and Temsirolimus and IFN-α, a total of 616 patients were treated. Two hundred patients received IFN-α weekly, 208 received Temsirolimus 25 mg weekly, and 208 patients received a combination of Temsirolimus and IFN-α weekly.
- Treatment with the combination of Temsirolimus 15 mg and IFN-α was associated with an increased incidence of multiple adverse reactions and did not result in a significant increase in overall survival when compared with IFN-α alone.
- Table 1 shows the percentage of patients experiencing treatment emergent adverse reactions. Reactions reported in at least 10% of patients who received Temsirolimus 25 mg alone or IFN-α alone are listed. Table 2 shows the percentage of patients experiencing selected laboratory abnormalities. Data for the same adverse reactions and laboratory abnormalities in the IFN-α alone arm are shown for comparison:
Postmarketing Experience
- The following adverse reactions have been identified during post approval use of Temsirolimus. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to readily estimate their frequency or establish a causal relationship to drug exposure.
- The following adverse reactions have been observed in patients receiving temsirolimus: rhabdomyolysis, Stevens-Johnson Syndrome, and complex regional pain syndrome (reflex sympathetic dystrophy).
- There are also post-marketing reports of temsirolimus extravasations resulting in swelling, pain, warmth, and erythema.
Drug Interactions
Agents Inducing CYP3A Metabolism
- Co-administration of Temsirolimus with rifampin, a potent CYP3A4/5 inducer, had no significant effect on temsirolimus Cmax (maximum concentration) and AUC (area under the concentration versus the time curve) after intravenous administration, but decreased sirolimus Cmax by 65% and AUC by 56% compared to Temsirolimus treatment alone. If alternative treatment cannot be administered, a dose adjustment should be considered.
Agents Inhibiting CYP3A Metabolism
- Co-administration of Temsirolimus with ketoconazole, a potent CYP3A4 inhibitor, had no significant effect on temsirolimus Cmax or AUC; however, sirolimus AUC increased 3.1-fold, and Cmax increased 2.2-fold compared to Temsirolimus alone. If alternative treatment cannot be administered, a dose adjustment should be considered.
Interactions with Drugs Metabolized by CYP2D6
- The concentration of desipramine, a CYP2D6 substrate, was unaffected when 25 mg of Temsirolimus was co-administered. No clinically significant effect is anticipated when temsirolimus is co-administered with agents that are metabolized by CYP2D6 or CYP3A4.
Use in Specific Populations
Pregnancy
- Women of childbearing potential should be advised to avoid becoming pregnant throughout treatment and for 3 months after Temsirolimus therapy has stopped.
- Temsirolimus can cause fetal harm when administered to a pregnant woman. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
- Temsirolimus administered daily as an oral formulation caused embryo-fetal and intrauterine toxicities in rats and rabbits at human sub-therapeutic exposures. Embryo-fetal adverse effects in rats consisted of reduced fetal weight and reduced ossifications, and in rabbits included reduced fetal weight, omphalocele, bifurcated sternabrae, notched ribs, and incomplete ossifications.
- In rats, the intrauterine and embryo-fetal adverse effects were observed at the oral dose of 2.7 mg/m2/day (approximately 0.04-fold the AUC in patients with cancer at the human recommended dose). In rabbits, the intrauterine and embryo-fetal adverse effects were observed at the oral dose of ≥7.2 mg/m2/day (approximately 0.12-fold the AUC in patients with cancer at the recommended human dose).
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Temsirolimus in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Temsirolimus during labor and delivery.
Nursing Mothers
- It is not known whether Temsirolimus is excreted into human milk, and due to the potential for tumorigenicity shown for sirolimus (active metabolite of Temsirolimus) in animal studies, a decision should be made whether to discontinue nursing or discontinue Temsirolimus, taking into account the importance of the drug to the mother.
Pediatric Use
- Limited data are available on the use of temsirolimus in pediatric patients. The effectiveness of temsirolimus in pediatric patients with advanced recurrent/refractory solid tumors has not been established.
- Temsirolimus was studied in 71 patients (59 patients ages 1 to 17 years and 12 patients ages 18 to 21 years) with relapsed/refractory solid tumors in a phase 1–2 safety and exploratory pharmacodynamic study.
- In phase 1, 19 pediatric patients with advanced recurrent/refractory solid tumors received Temsirolimus at doses ranging from 10 mg/m2 to 150 mg/m2 as a 60-minute intravenous infusion once weekly in three-week cycles.
- In phase 2, 52 pediatric patients with recurrent/relapsed neuroblastoma, rhabdomyosarcoma, or high grade glioma received Temsirolimus at a weekly dose of 75 mg/m2. One of 19 patients with neuroblastoma achieved a partial response. There were no objective responses in pediatric patients with recurrent/relapsed rhabdomyosarcoma or high grade glioma.
- Adverse reactions associated with Temsirolimus were similar to those observed in adults. The most common adverse reactions (≥20%) in pediatric patients receiving the 75 mg/m2 dose included thrombocytopenia, infections, asthenia/fatigue, fever, pain, leukopenia, rash, anemia, hyperlipidemia, increased cough, stomatitis, anorexia, increased plasma levels of alanine aminotransferase and aspartate aminotransferase, hypercholesterolemia, hyperglycemia, abdominal pain, headache, arthralgia, upper respiratory infection, nausea and vomiting, neutropenia, hypokalemia, and hypophosphatemia.
- Pharmacokinetics
- In phase 1 of the above mentioned pediatric trial, the single dose and multiple dose total systemic exposure (AUC) of temsirolimus and sirolimus were less than dose-proportional over the dose range of 10 to 150 mg/m2.
- In the phase 2 portion, the multiple dose (Day 1, Cycle 2) pharmacokinetics of Temsirolimus 75 mg/m2 were characterized in an additional 35 patients ages 28 days to 21 years (median age of 8 years). The geometric mean body surface adjusted clearance of temsirolimus and sirolimus was 9.45 L/h/m2 and 9.26 L/h/m2, respectively. The mean elimination half-life of temsirolimus and sirolimus was 31 hours and 44 hours, respectively.
- The exposure (AUCss) to temsirolimus and sirolimus was approximately 6-fold and 2-fold higher, respectively than the exposure in adult patients receiving a 25 mg intravenous infusion.
Geriatic Use
- Clinical studies of Temsirolimus did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Based on the results of a phase 3 study, elderly patients may be more likely to experience certain adverse reactions including diarrhea, edema, and pneumonia.
Gender
There is no FDA guidance on the use of Temsirolimus with respect to specific gender populations.
Race
There is no FDA guidance on the use of Temsirolimus with respect to specific racial populations.
Renal Impairment
- No clinical studies were conducted with Temsirolimus in patients with decreased renal function. Less than 5% of total radioactivity was excreted in the urine following a 25 mg intravenous dose of [14C]-labeled temsirolimus in healthy subjects. Renal impairment is not expected to markedly influence drug exposure, and no dosage adjustment of Temsirolimus is recommended in patients with renal impairment.
- Temsirolimus has not been studied in patients undergoing hemodialysis.
Hepatic Impairment
- Temsirolimus was evaluated in a dose escalation phase 1 study in 110 patients with normal or varying degrees of hepatic impairment as defined by AST and bilirubin levels and patients with liver transplant (Table 3). Patients with moderate and severe hepatic impairment had increased rates of adverse reactions and deaths, including deaths due to progressive disease, during the study (Table 3).
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Temsirolimus in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Temsirolimus in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
- Intravenous
Monitoring
- Monitor for symptoms or radiographic changes of interstitial lung disease (ILD). If ILD is suspected, discontinue Temsirolimus, and consider use of corticosteroids and/or antibiotics.
- Monitor renal function at baseline and while on Temsirolimus.
- In the randomized, phase 3 trial, complete blood counts (CBCs) were checked weekly, and chemistry panels were checked every two weeks. Laboratory monitoring for patients receiving Temsirolimus may need to be performed more or less frequently at the physician's discretion.
IV Compatibility
There is limited information regarding IV Compatibility of Temsirolimus in the drug label.
Overdosage
- There is no specific treatment for Temsirolimus intravenous overdose. Temsirolimus has been administered to patients with cancer in phase 1 and 2 trials with repeated intravenous doses as high as 220 mg/m2. The risk of several serious adverse events, including thrombosis, bowel perforation, interstitial lung disease (ILD), seizure, and psychosis, is increased with doses of Temsirolimus greater than 25 mg.
Pharmacology
Mechanism of Action
- Temsirolimus is an inhibitor of mTOR (mammalian target of rapamycin). Temsirolimus binds to an intracellular protein (FKBP-12), and the protein-drug complex inhibits the activity of mTOR that controls cell division. Inhibition of mTOR activity resulted in a G1 growth arrest in treated tumor cells. When mTOR was inhibited, its ability to phosphorylate p70S6k and S6 ribosomal protein, which are downstream of mTOR in the PI3 kinase/AKT pathway was blocked.
- In in vitro studies using renal cell carcinoma cell lines, temsirolimus inhibited the activity of mTOR and resulted in reduced levels of the hypoxia-inducible factors HIF-1 and HIF-2 alpha, and the vascular endothelial growth factor.
Structure
- Temsirolimus, an inhibitor of mTOR, is an antineoplastic agent.
- Temsirolimus is a white to off-white powder with a molecular formula of C56H87NO16 and a molecular weight of 1030.30. It is non-hygroscopic. Temsirolimus is practically insoluble in water and soluble in alcohol. It has no ionizable functional groups, and its solubility is independent of pH.
- The chemical name of temsirolimus is (3S,6R,7E,9R,10R,12R,14S,15E,17E,19E,21S,23S,26R,27R,34aS)-9,10,12,13,14,21,22,23,24,25,26,27,32,33,34,34a-Hexadecahydro-9,27-dihydroxy-3-[(1R)-2-[(1S,3R,4R)-4-hydroxy-3-methoxycyclohexyl]-1-methylethyl]-10,21-dimethoxy-6,8,12,14,20,26-hexamethyl-23, 27-epoxy-3H-pyrido[2,1-c][1,4]oxaazacyclohentriacontine-1,5,11,28,29(4H,6H,31H)-pentone 4'-[2,2-bis(hydroxymethyl)propionate]; or Rapamycin, 42-[3-hydroxy-2-(hydroxymethyl)-2-methylpropanoate].
- Temsirolimus (temsirolimus) injection, 25 mg/mL, is a clear, colorless to light yellow, non-aqueous, ethanolic, sterile solution. Temsirolimus (temsirolimus) injection requires two dilutions prior to intravenous infusion. Temsirolimus (temsirolimus) injection should be diluted only with the supplied DILUENT for Temsirolimus®.
- DILUENT for Temsirolimus® is a sterile, non-aqueous solution that is supplied with Temsirolimus injection, as a kit.
- Temsirolimus (temsirolimus) injection, 25 mg/mL:
- Active ingredient: temsirolimus (25 mg/mL)
- Inactive ingredients: dehydrated alcohol (39.5% w/v), dl-alpha-tocopherol (0.075% w/v), propylene glycol (50.3% w/v), and anhydrous citric acid (0.0025% w/v).
DILUENT for Temsirolimus®
- Inactive ingredients
- Polysorbate 80 (40.0% w/v), polyethylene glycol 400 (42.8% w/v) and dehydrated alcohol (19.9% w/v).
- After the Temsirolimus (temsirolimus) injection vial has been diluted with DILUENT for Temsirolimus®, in accordance with the instructions in section 2.5, the solution contains 35.2% alcohol.
- Temsirolimus (temsirolimus) injection and DILUENT for Temsirolimus® are filled in clear glass vials with butyl rubber stoppers.
Pharmacodynamics
- Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for Temsirolimus. In a randomized, single-blinded, crossover study, 58 healthy subjects received Temsirolimus 25 mg, placebo, and a single oral dose of moxifloxacin 400 mg.
- A supratherapeutic Temsirolimus dose was not studied in this randomized QT trial. The largest difference between the upper bound 2-sided 90% CI for the mean difference between Temsirolimus and placebo-corrected QT interval was less than 10 ms. In a different trial in 69 patients with a hematologic malignancy, Temsirolimus doses up to 175 mg were studied. No patient with a normal QTcF at baseline had an increase in QTcF >60 ms. Additionally, there were no patients with a QTcF interval greater than 500 ms.
Pharmacokinetics
- Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for Temsirolimus. In a randomized, single-blinded, crossover study, 58 healthy subjects received Temsirolimus 25 mg, placebo, and a single oral dose of moxifloxacin 400 mg.
- A supratherapeutic Temsirolimus dose was not studied in this randomized QT trial. The largest difference between the upper bound 2-sided 90% CI for the mean difference between Temsirolimus and placebo-corrected QT interval was less than 10 ms. In a different trial in 69 patients with a hematologic malignancy, Temsirolimus doses up to 175 mg were studied. No patient with a normal QTcF at baseline had an increase in QTcF >60 ms. Additionally, there were no patients with a QTcF interval greater than 500 ms.
Nonclinical Toxicology
- Effects on Electrocardiogram: There were no clinically relevant QT changes observed at the recommended dose for Temsirolimus. In a randomized, single-blinded, crossover study, 58 healthy subjects received Temsirolimus 25 mg, placebo, and a single oral dose of moxifloxacin 400 mg. A supratherapeutic Temsirolimus dose was not studied in this randomized QT trial.
- The largest difference between the upper bound 2-sided 90% CI for the mean difference between Temsirolimus and placebo-corrected QT interval was less than 10 ms. In a different trial in 69 patients with a hematologic malignancy, Temsirolimus doses up to 175 mg were studied. No patient with a normal QTcF at baseline had an increase in QTcF >60 ms. Additionally, there were no patients with a QTcF interval greater than 500 ms.
Clinical Studies
- A phase 3, multi-center, three-arm, randomized, open-label study was conducted in previously untreated patients with advanced renal cell carcinoma (clear cell and non-clear cell histologies). The objectives were to compare Overall Survival (OS), Progression-Free Survival (PFS), Objective Response Rate (ORR), and safety in patients receiving IFN-α to those receiving Temsirolimus or Temsirolimus plus IFN-α.
- Patients in this study had 3 or more of 6 pre-selected prognostic risk factors (less than one year from time of initial renal cell carcinoma diagnosis to randomization, Karnofsky performance status of 60 or 70, hemoglobin less than the lower limit of normal, corrected calcium of greater than 10 mg/dL, lactate dehydrogenase >1.5 times the upper limit of normal, more than one metastatic organ site). Patients were stratified for prior nephrectomy status within three geographic regions and were randomly assigned (1:1:1) to receive IFN-α alone (n = 207), Temsirolimus alone (25 mg weekly; n = 209), or the combination arm (n = 210).
- The ITT population for this interim analysis included 626 patients. Demographics were comparable between the three treatment arms with regard to age, gender, and race. The mean age of all groups was 59 years (range 23–86). Sixty-nine percent were male and 31% were female. The racial distribution for all groups was 91% White, 4% Black, 2% Asian, and 3% other. Sixty-seven percent of patients had a history of prior nephrectomy.
- The median duration of treatment in the Temsirolimus arm was 17 weeks (range 1–126 weeks). The median duration of treatment on the IFN arm was 8 weeks (range 1–124 weeks).
- There was a statistically significant improvement in OS (time from randomization to death) in the Temsirolimus 25 mg arm compared to IFN-α. The combination of Temsirolimus 15 mg and IFN-α did not result in a significant increase in OS when compared with IFN-α alone. Figure 1 is a Kaplan-Meier plot of OS in this study. The evaluations of PFS (time from randomization to disease progression or death) and ORR, were based on blinded independent radiologic assessment of tumor response. Efficacy results are summarized in Table 4.
How Supplied
- NDC 0008-1179-01 Temsirolimus® (temsirolimus) injection, 25 mg/mL.
Storage
- Each kit is supplied in a single carton containing one single-use vial of 25 mg/mL of temsirolimus and one DILUENT vial which includes a deliverable volume of 1.8 mL, and must be stored at 2°–8° C (36°–46° F). Protect from light.
Images
Drug Images
{{#ask: Page Name::Temsirolimus |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
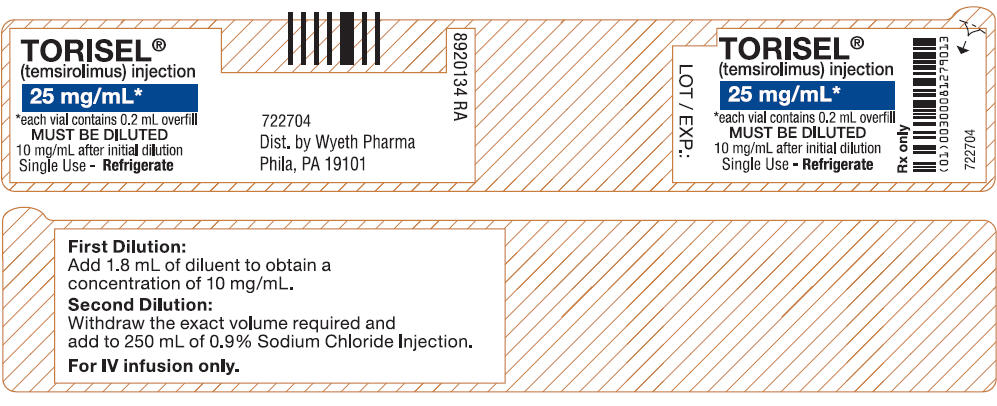

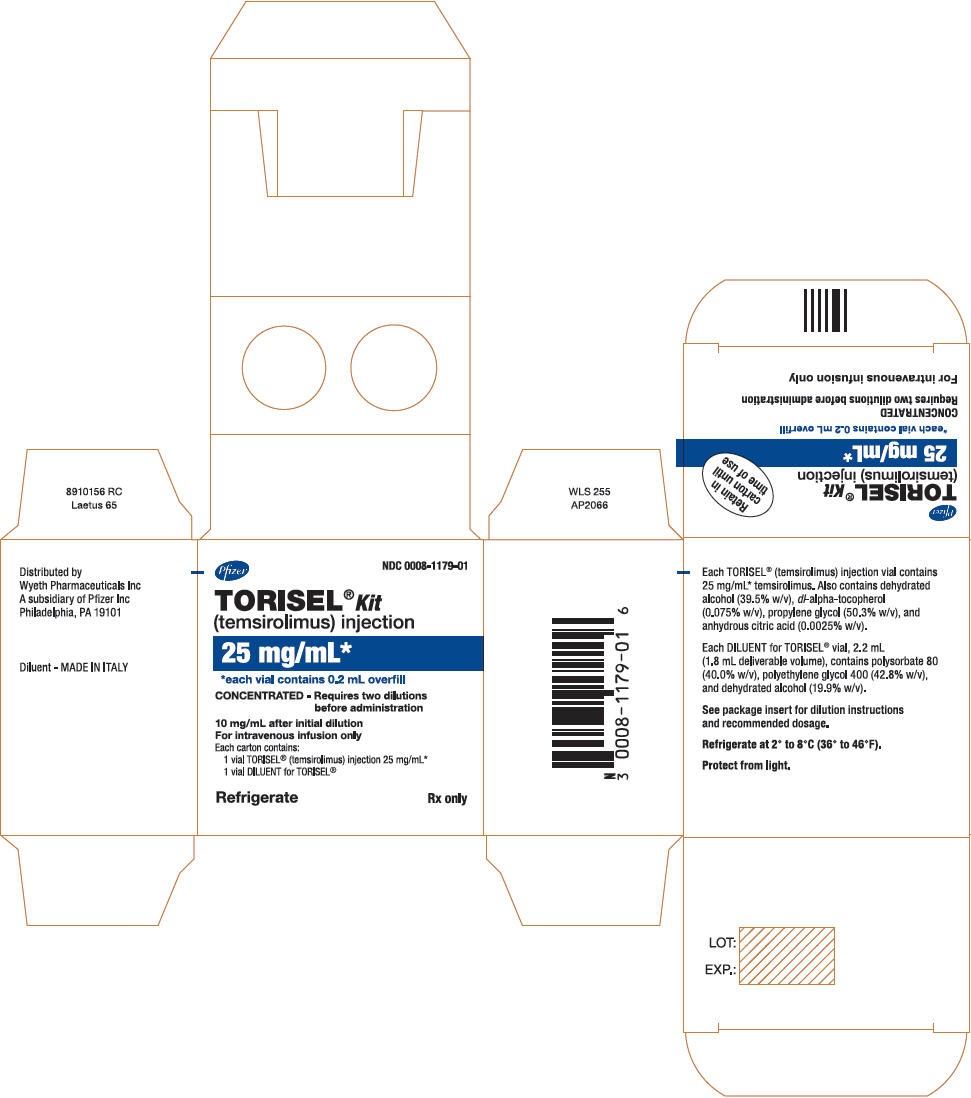
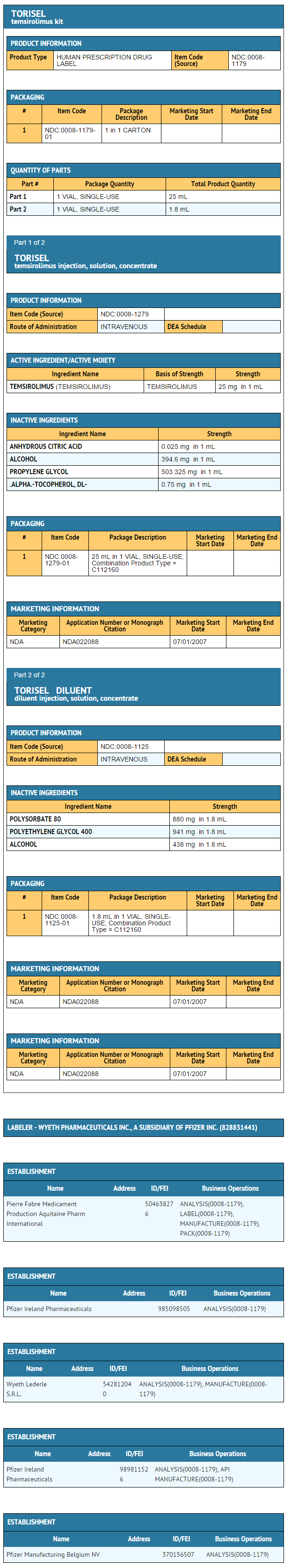
{{#ask: Label Page::Temsirolimus |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Each kit is supplied in a single carton containing one single-use vial of 25 mg/mL of temsirolimus and one DILUENT vial which includes a deliverable volume of 1.8 mL, and must be stored at 2°–8° C (36°–46° F). Protect from light.
Precautions with Alcohol
- Alcohol-Temsirolimus interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Temsirolimus ®[2]
Look-Alike Drug Names
There is limited information regarding Temsirolimus Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Hess G, Herbrecht R, Romaguera J, Verhoef G, Crump M, Gisselbrecht C; et al. (2009). "Phase III study to evaluate temsirolimus compared with investigator's choice therapy for the treatment of relapsed or refractory mantle cell lymphoma". J Clin Oncol. 27 (23): 3822–9. doi:10.1200/JCO.2008.20.7977. PMID 19581539 PMID: 19581539 Check
|pmid=value (help). - ↑ "Temsirolimus- temsirolimus".
{{#subobject:
|Label Page=Temsirolimus |Label Name=Tero06.jpg
}}
{{#subobject:
|Label Page=Temsirolimus |Label Name=Tero07.jpg
}}
{{#subobject:
|Label Page=Temsirolimus |Label Name=Tero08.jpg
}}
{{#subobject:
|Label Page=Temsirolimus |Label Name=Tero09.png
}}