Aspirin and dipyridamole: Difference between revisions
No edit summary |
No edit summary |
||
| (14 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{DrugProjectFormSinglePage | {{DrugProjectFormSinglePage | ||
|authorTag={{Ammu}} | |authorTag={{Ammu}} | ||
|genericName= | |genericName=Aspirin and dipyridamole | ||
|aOrAn=a | |aOrAn=a | ||
|drugClass=platelet aggregation inhibitor | |drugClass=[[platelet aggregation inhibitor]] | ||
|indicationType=prophylaxis | |indicationType=prophylaxis | ||
|indication=to reduce the risk of stroke in patients who have had transient ischemia of the brain or completed ischemic stroke due to thrombosis | |indication=to reduce the risk of [[stroke]] in patients who have had transient [[ischemia]] of the brain or completed [[ischemic stroke]] due to [[thrombosis]] | ||
|adverseReactions=abdominal pain, diarrhea, headache, arthralgia | |adverseReactions=[[abdominal pain]], [[diarrhea]], [[headache]], [[arthralgia]] | ||
|blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | |blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | |blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | ||
|fdaLIADAdult= | |fdaLIADAdult=* To reduce the risk of stroke in patients who have had [[transient ischemia]] of the brain or completed [[ischemic stroke]] due to [[thrombosis]]. | ||
* Aspirin and dipyridamole is not interchangeable with the individual components of [[aspirin]] and [[dipyridamole]] tablets. | |||
* The recommended dose of aspirin and dipyridamole is one capsule given orally twice daily, one in the morning and one in the evening. Swallow capsules whole without chewing. aspirin and dipyridamole can be administered with or without food. | |||
The recommended dose of | =====Alternative Regimen in Case of Intolerable Headaches===== | ||
* In the event of intolerable headaches during initial treatment, switch to one capsule at bedtime and low-dose [[aspirin]] in the morning. Because there are no outcome data with this regimen and headaches become less of a problem as treatment continues, patients should return to the usual regimen as soon as possible, usually within one week. | |||
In the event of intolerable headaches during initial treatment, switch to one capsule at bedtime and low-dose aspirin in the morning. Because there are no outcome data with this regimen and headaches become less of a problem as treatment continues, patients should return to the usual regimen as soon as possible, usually within one week. | |||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Aspirin and dipyridamole in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Aspirin and dipyridamole in adult patients. | ||
|offLabelAdultNoGuideSupport= | |offLabelAdultNoGuideSupport=* [[Hemodialysis]] - [[Thrombosis]]; Prophylaxis<ref name="pmidPMID: 19458364">{{cite journal| author=Dixon BS, Beck GJ, Vazquez MA, Greenberg A, Delmez JA, Allon M et al.| title=Effect of dipyridamole plus aspirin on hemodialysis graft patency. | journal=N Engl J Med | year= 2009 | volume= 360 | issue= 21 | pages= 2191-201 | pmid=PMID: 19458364 | doi=10.1056/NEJMoa0805840 | pmc=PMC3929400 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19458364 }} </ref> | ||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Aspirin and dipyridamole in pediatric patients. | |offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Aspirin and dipyridamole in pediatric patients. | ||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Aspirin and dipyridamole in pediatric patients. | |offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Aspirin and dipyridamole in pediatric patients. | ||
|contraindications= | |contraindications======Hypersensitivity===== | ||
* Aspirin and dipyridamole is contraindicated in patients with known hypersensitivity to any of the product components. | |||
=====Allergy===== | |||
* [[Aspirin]] is contraindicated in patients with known allergy to [[nonsteroidal anti-inflammatory drug]] products and in patients with the syndrome of [[asthma]], [[rhinitis]], and [[nasal polyps]]. [[Aspirin]] may cause severe [[urticaria]], [[angioedema]] or [[bronchospasm]]. | |||
Aspirin is contraindicated in patients with known allergy to nonsteroidal anti-inflammatory drug products and in patients with the syndrome of asthma, rhinitis, and nasal polyps. Aspirin may cause severe urticaria, angioedema or bronchospasm. | =====Reye Syndrome===== | ||
* Do not use [[aspirin]] in children or teenagers with [[viral infections]] because of the risk of [[Reye syndrome]]. | |||
|warnings======Hypersensitivity===== | |||
Do not use aspirin in children or teenagers with viral infections because of the risk of Reye syndrome. | * Aspirin and dipyridamole is contraindicated in patients with known [[hypersensitivity]] to any of the product components. | ||
|warnings= | =====Allergy===== | ||
* [[Aspirin]] is contraindicated in patients with known [[allergy]] to [[nonsteroidal anti-inflammatory drug]] products and in patients with the syndrome of [[asthma]], [[rhinitis]], and [[nasal polyps]]. [[Aspirin]] may cause severe [[urticaria]], [[angioedema]] or [[bronchospasm]]. | |||
=====Reye Syndrome===== | |||
* Do not use [[aspirin]] in children or teenagers with viral infections because of the risk of [[Reye syndrome]]. | |||
|clinicalTrials=* The following adverse reactions are discussed elsewhere in the labeling: | |||
:* [[Hypersensitivity]]. | |||
:* [[Allergy]]. | |||
Do not use aspirin in children or teenagers with viral infections because of the risk of Reye syndrome. | :* Risk of [[bleeding]]. | ||
|clinicalTrials=The following adverse reactions are discussed elsewhere in the labeling: | =====Clinical Trials Experience===== | ||
* Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |||
Hypersensitivity | * The efficacy and safety of aspirin and dipyridamole was established in the European Stroke Prevention Study-2 (ESPS2). ESPS2 was a double-blind, placebo controlled study that evaluated 6602 patients over the age of 18 years who had a previous ischemic stroke or transient ischemic attack within ninety days prior to entry. Patients were randomized to either aspirin and dipyridamole, aspirin, ER-DP, or placebo; primary endpoints included stroke (fatal or nonfatal) and death from all causes. | ||
Allergy | * This 24-month, multicenter, double-blind, randomized study (ESPS2) was conducted to compare the efficacy and safety of aspirin and dipyridamole with placebo, extended-release dipyridamole alone and aspirin alone. The study was conducted in a total of 6602 male and female patients who had experienced a previous ischemic stroke or transient ischemia of the [[brain]] within three months prior to randomization. | ||
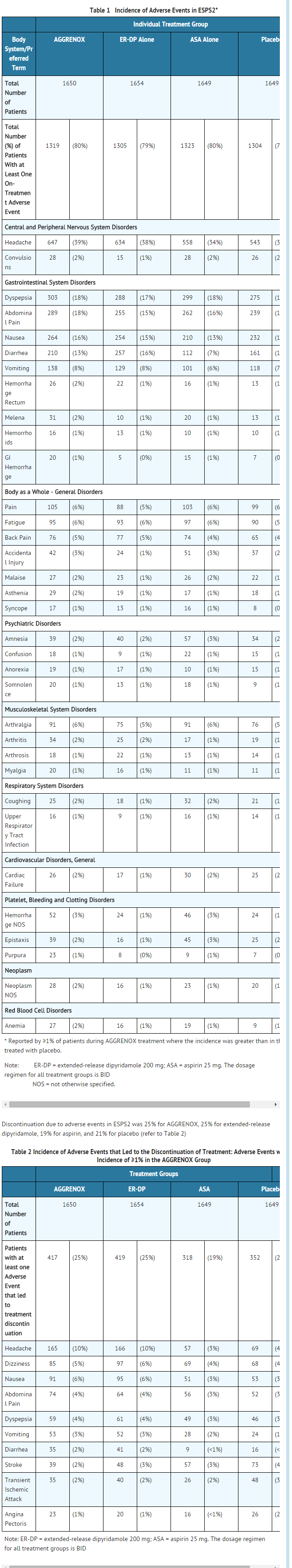
Risk of | * Table 1 presents the incidence of adverse events that occurred in 1% or more of patients treated with aspirin and dipyridamole where the incidence was also greater than in those patients treated with placebo. There is no clear benefit of the dipyridamole/aspirin combination over aspirin with respect to safety. | ||
: [[File:A & D Advere 04.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | * Headache was most notable in the first month of treatment. | ||
=====Other Adverse Events===== | |||
The efficacy and safety of | * Adverse reactions that occurred in less than 1% of patients treated with aspirin and dipyridamole in the ESPS2 study and that were medically judged to be possibly related to either dipyridamole or aspirin are listed below. | ||
* Body as a Whole | |||
This 24-month, multicenter, double-blind, randomized study (ESPS2) was conducted to compare the efficacy and safety of | :* Allergic reaction, [[fever]] | ||
* Cardiovascular | |||
Table 1 presents the incidence of adverse events that occurred in 1% or more of patients treated with | :* [[Hypotension]] | ||
: [[File: | * [[Central Nervous System]] | ||
Headache was most notable in the first month of treatment. | :* [[Coma]], [[dizziness]], [[paresthesia]], [[cerebral hemorrhage]], [[intracranial hemorrhage]], [[subarachnoid hemorrhage]] | ||
* [[Gastrointestinal]] | |||
Other Adverse Events | :* [[Gastritis]] ulceration and perforation | ||
Adverse reactions that occurred in less than 1% of patients treated with | * Hearing and Vestibular Disorders | ||
:* [[Tinnitus]], and [[deafness]]. Patients with high frequency hearing loss may have difficulty perceiving [[tinnitus]]. In these patients, tinnitus cannot be used as a clinical indicator of salicylism | |||
Body as a Whole: Allergic reaction, fever | * [[Heart rate]] and rhythm disorders | ||
:* [[Tachycardia]], [[palpitation]], [[arrhythmia]], [[supraventricular tachycardia]] | |||
* [[Liver]] and [[biliary system]] disorders | |||
:* [[Cholelithiasis]], [[jaundice]], hepatic function abnormal | |||
Central Nervous System: Coma, dizziness, paresthesia, cerebral hemorrhage, intracranial hemorrhage, subarachnoid hemorrhage | * Metabolic and Nutritional Disorders | ||
:* [[Hyperglycemia]], thirst | |||
* [[Platelet]], bleeding and clotting disorders | |||
:* [[Hematoma]], [[gingival bleeding]] | |||
Hearing and Vestibular Disorders: Tinnitus, and deafness. Patients with high frequency hearing loss may have difficulty perceiving tinnitus. In these patients, tinnitus cannot be used as a clinical indicator of salicylism | * Psychiatric disorders | ||
:* [[Agitation]] | |||
Heart | * Reproductive | ||
:* [[Uterine hemorrhage]] | |||
Liver and | * Respiratory | ||
:* [[Hyperpnea]], [[asthma]],[[bronchospasm]], [[hemoptysis]], [[pulmonary edema]] | |||
Metabolic and Nutritional Disorders: Hyperglycemia, thirst | * Special Senses Other Disorders | ||
:* [[Taste loss]] | |||
Platelet, | * [[Skin]] and appendages disorders | ||
:* [[Pruritus]], [[urticaria]] | |||
* [[Urogenital]] | |||
:* Renal insufficiency and failure, [[hematuria]] | |||
* Vascular (Extracardiac) Disorders | |||
:* [[Flushing]] | |||
=====Laboratory Changes===== | |||
* Over the course of the 24-month study (ESPS2), patients treated with aspirin and dipyridamole showed a decline (mean change from baseline) in hemoglobin of 0.25 g/dL, hematocrit of 0.75%, and erythrocyte count of 0.13x106/mm3. | |||
Special Senses Other Disorders: Taste loss | |postmarketing=* The following is a list of additional adverse reactions that have been reported either in the literature or are from post-marketing spontaneous reports for either [[dipyridamole]] or [[aspirin]]. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) strength of causal connection to aspirin and dipyridamole. | ||
* [[Body]] as a Whole | |||
Skin and | :* [[Hypothermia]], [[chest pain]] | ||
* Cardiovascular | |||
Urogenital: Renal insufficiency and failure, hematuria | :* [[Angina pectoris]] | ||
* Central Nervous System | |||
Vascular (Extracardiac) Disorders: Flushing | :* [[Cerebral edema]] | ||
* [[Fluid]] and [[electrolyte]] | |||
Laboratory Changes | :* [[Hyperkalemia]], [[metabolic acidosis]], [[respiratory alkalosis]], [[hypokalemia]] | ||
Over the course of the 24-month study (ESPS2), patients treated with | * Gastrointestinal | ||
|postmarketing=The following is a list of additional adverse reactions that have been reported either in the literature or are from post-marketing spontaneous reports for either dipyridamole or aspirin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) strength of causal connection to | :* [[Pancreatitis]], [[Reye syndrome]], [[hematemesis]] | ||
* Hearing and Vestibular Disorders | |||
Body as a Whole: Hypothermia, chest pain | :* [[Hearing loss]] | ||
* Immune System Disorders | |||
:* [[Hypersensitivity]], acute [[anaphylaxis]], [[laryngeal edema]] | |||
* [[Liver]] and Biliary System Disorders | |||
Central Nervous System: Cerebral edema | :* [[Hepatitis]], [[hepatic failure]] | ||
* Musculoskeletal | |||
Fluid and | :* [[Rhabdomyolysis]] | ||
* Metabolic and Nutritional Disorders | |||
:* [[Hypoglycemia]], [[dehydration]] | |||
* Platelet, Bleeding and Clotting Disorders | |||
Hearing and Vestibular Disorders: Hearing loss | :* Prolongation of the [[prothrombin time]], [[disseminated intravascular coagulation]], coagulopathy, [[thrombocytopenia]] | ||
* Reproductive | |||
Immune System Disorders: Hypersensitivity, acute anaphylaxis, laryngeal edema | :* Prolonged [[pregnancy]] and [[labor]], stillbirths, lower birth weight infants, antepartum and [[postpartum bleeding]] | ||
* Respiratory | |||
Liver and Biliary System Disorders: Hepatitis, hepatic failure | :* [[Tachypnea]], [[dyspnea]] | ||
* [[Skin]] and Appendages Disorders | |||
:* [[Rash]], [[alopecia]], [[angioedema]], [[Stevens-Johnson syndrome]], [[skin hemorrhages]] such as [[bruising]], [[ecchymosis]], and [[hematoma]] | |||
* [[Urogenital]] | |||
Metabolic and Nutritional Disorders: Hypoglycemia, dehydration | :* [[Interstitial nephritis]], [[papillary necrosis]], [[proteinuria]] | ||
* Vascular (Extracardiac Disorders) | |||
Platelet, Bleeding and Clotting Disorders: Prolongation of the prothrombin time, disseminated intravascular coagulation, coagulopathy, thrombocytopenia | :* [[Allergic vasculitis]] | ||
* Other Adverse Events | |||
:* [[Anorexia]], [[aplastic anemia]], [[migraine]], [[pancytopenia]], [[thrombocytosis]]. | |||
|drugInteractions======Drug Interaction Study Information Obtained From Literature===== | |||
* [[Adenosine]] | |||
:* [[Dipyridamole]] has been reported to increase the plasma levels and cardiovascular effects of [[adenosine]]. Adjustment of adenosine dosage may be necessary. | |||
Skin and Appendages Disorders: Rash, alopecia, angioedema, Stevens-Johnson syndrome, skin hemorrhages such as bruising, ecchymosis, and hematoma | =====Angiotensin Converting Enzyme (ACE) Inhibitors===== | ||
* Due to the indirect effect of aspirin on the renin-angiotensin conversion pathway, the hyponatremic and hypotensive effects of ACE inhibitors may be diminished by concomitant administration of aspirin. | |||
Urogenital: Interstitial nephritis, papillary necrosis, proteinuria | * [[Acetazolamide]] | ||
:* Concurrent use of aspirin and acetazolamide can lead to high serum concentrations of acetazolamide (and toxicity) due to competition at the renal tubule for secretion. | |||
Vascular (Extracardiac Disorders): Allergic vasculitis | =====Anticoagulants and Antiplatelets===== | ||
* Patients taking aspirin and dipyridamole in combination with anticoagulants, antiplatelets, or any substance impacting coagulation are at increased risk for bleeding. Aspirin can displace warfarin from protein binding sites, leading to prolongation of both the prothrombin time and the bleeding time. Aspirin can increase the anticoagulant activity of heparin, increasing bleeding risk. | |||
Other Adverse Events: | =====Anticonvulsants===== | ||
|drugInteractions= | * Salicylic acid can displace protein-bound phenytoin and valproic acid, leading to a decrease in the total concentration of phenytoin and an increase in serum [[valproic acid]] levels. | ||
Adenosine | =====Beta Blockers===== | ||
Dipyridamole has been reported to increase the plasma levels and cardiovascular effects of adenosine. Adjustment of adenosine dosage may be necessary. | * The hypotensive effects of [[beta blockers]] may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention. | ||
=====Cholinesterase Inhibitors===== | |||
Angiotensin Converting Enzyme (ACE) Inhibitors | * Dipyridamole may counteract the anticholinesterase effect of cholinesterase inhibitors, thereby potentially aggravating [[myasthenia gravis]]. | ||
Due to the indirect effect of aspirin on the renin-angiotensin conversion pathway, the hyponatremic and hypotensive effects of ACE inhibitors may be diminished by concomitant administration of aspirin. | =====Diuretics===== | ||
* The effectiveness of diuretics in patients with underlying renal or cardiovascular disease may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention. | |||
Acetazolamide | =====Methotrexate===== | ||
Concurrent use of aspirin and acetazolamide can lead to high serum concentrations of acetazolamide (and toxicity) due to competition at the renal tubule for secretion. | * Salicylate can inhibit renal clearance of methotrexate, leading to bone marrow toxicity, especially in the elderly or renal impaired. | ||
=====Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)===== | |||
Anticoagulants and Antiplatelets | * The concurrent use of aspirin with other NSAIDs may increase bleeding or lead to decreased renal function. | ||
Patients taking | =====Oral Hypoglycemics===== | ||
* Moderate doses of aspirin may increase the effectiveness of oral hypoglycemic drugs, leading to hypoglycemia. | |||
Anticonvulsants | =====Uricosuric Agents (probenecid and sulfinpyrazone)===== | ||
Salicylic acid can displace protein-bound phenytoin and valproic acid, leading to a decrease in the total concentration of phenytoin and an increase in serum valproic acid levels. | * Salicylates antagonize the uricosuric action of uricosuric agents. | ||
Beta Blockers | |||
The hypotensive effects of beta blockers may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention. | |||
Cholinesterase Inhibitors | |||
Dipyridamole may counteract the anticholinesterase effect of cholinesterase inhibitors, thereby potentially aggravating myasthenia gravis. | |||
Diuretics | |||
The effectiveness of diuretics in patients with underlying renal or cardiovascular disease may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention. | |||
Methotrexate | |||
Salicylate can inhibit renal clearance of methotrexate, leading to bone marrow toxicity, especially in the elderly or renal impaired. | |||
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) | |||
The concurrent use of aspirin with other NSAIDs may increase bleeding or lead to decreased renal function. | |||
Oral Hypoglycemics | |||
Moderate doses of aspirin may increase the effectiveness of oral hypoglycemic drugs, leading to hypoglycemia. | |||
Uricosuric Agents (probenecid and sulfinpyrazone) | |||
Salicylates antagonize the uricosuric action of uricosuric agents. | |||
|FDAPregCat=D | |FDAPregCat=D | ||
|useInLaborDelivery=Aspirin can result in excessive blood loss at delivery as well as prolonged gestation and prolonged labor. Because of these effects on the mother and because of adverse fetal effects seen with aspirin during the later stages of pregnancy | |useInLaborDelivery=* Aspirin can result in excessive blood loss at delivery as well as prolonged gestation and prolonged labor. Because of these effects on the mother and because of adverse fetal effects seen with aspirin during the later stages of pregnancy, avoid aspirin and dipyridamole in the third trimester of pregnancy and during labor and delivery. | ||
|useInNursing=Both dipyridamole and aspirin are excreted in human milk. Exercise caution when | |useInNursing=* Both [[dipyridamole]] and [[aspirin]] are excreted in human milk. Exercise caution when aspirin and dipyridamole capsules are administered to a nursing woman. | ||
|useInPed=Safety and effectiveness of | |useInPed=* Safety and effectiveness of aspirin and dipyridamole in pediatric patients have not been studied. Due to the aspirin component, use of this product in the pediatric population is not recommended | ||
|useInGeri=Of the total number of subjects in ESPS2, 61 percent were 65 and over, while 27 percent were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out | |useInGeri=* Of the total number of subjects in ESPS2, 61 percent were 65 and over, while 27 percent were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out | ||
|useInHepaticImpair= | |useInHepaticImpair=* aspirin and dipyridamole has not been studied in patients with hepatic or renal impairment. Avoid using aspirin containing products, such as aspirin and dipyridamole in patients with severe hepatic or severe renal (glomerular filtration rate < 10 mL/min) dysfunction | ||
|administration=* Oral | |administration=* [[Oral]] | ||
|monitoring=* Plasma electrolytes and pH should be monitored serially to promote alkaline diuresis of salicylate if renal function is normal. In patients with renal insufficiency or in cases of life-threatening intoxication, dialysis is usually required to treat salicylic overdose, however since dipyridamole is highly protein bound, dialysis is not likely to remove dipyridamole. | |monitoring=* Plasma [[electrolytes]] and pH should be monitored serially to promote alkaline diuresis of salicylate if renal function is normal. In patients with renal insufficiency or in cases of life-threatening intoxication, dialysis is usually required to treat salicylic overdose, however since [[dipyridamole]] is highly protein bound, [[dialysis]] is not likely to remove [[dipyridamole]]. | ||
|overdose=Because of the dose ratio of dipyridamole to aspirin, overdosage of | |overdose=* Because of the dose ratio of dipyridamole to aspirin, overdosage of aspirin and dipyridamole is likely to be dominated by signs and symptoms of dipyridamole overdose. In case of real or suspected overdose, seek medical attention or contact a Poison Control Center immediately. Careful medical management is essential. | ||
* Based upon the known hemodynamic effects of dipyridamole, symptoms such as warm feeling, flushes, sweating, restlessness, feeling of weakness and dizziness may occur. A drop in [[blood pressure]] and [[tachycardia]] might also be observed. | |||
Based upon the known hemodynamic effects of dipyridamole, symptoms such as warm feeling, flushes, sweating, restlessness, feeling of weakness and dizziness may occur. A drop in blood pressure and tachycardia might also be observed. | * Salicylate toxicity may result from acute ingestion (overdose) or chronic intoxication. Severity of aspirin intoxication is determined by measuring the blood salicylate level. The early signs of salicylic overdose (salicylism), including tinnitus (ringing in the ears), occur at plasma concentrations approaching 200 µg/mL. In severe cases, [[hyperthermia]] and [[hypovolemia]] are the major immediate threats to life. Plasma concentrations of aspirin above 300 µg/mL are clearly toxic. Severe toxic effects are associated with levels above 400 µg/mL. A single lethal dose of aspirin in adults is not known with certainty but death may be expected at 30 g. | ||
* Treatment of overdose consists primarily of supporting vital functions, increasing drug elimination, and correcting acid-base disturbances. Consider gastric emptying and/or lavage as soon as possible after ingestion, even if the patient has vomited spontaneously. After lavage and/or emesis, administration of activated charcoal as a slurry may be beneficial if less than 3 hours have passed since ingestion. Charcoal absorption should not be employed prior to emesis and lavage. Follow acid-base status closely with serial blood gas and serum pH measurements. Maintain fluid and electrolyte balance. Administer replacement fluid intravenously and augment with correction of acidosis. Treatment may require the use of a [[vasopressor]]. Infusion of glucose may be required to control hypoglycemia. | |||
Salicylate toxicity may result from acute ingestion (overdose) or chronic intoxication. Severity of aspirin intoxication is determined by measuring the blood salicylate level. The early signs of salicylic overdose (salicylism), including tinnitus (ringing in the ears), occur at plasma concentrations approaching 200 µg/mL. In severe cases, hyperthermia and hypovolemia are the major immediate threats to life. Plasma concentrations of aspirin above 300 µg/mL are clearly toxic. Severe toxic effects are associated with levels above 400 µg/mL. A single lethal dose of aspirin in adults is not known with certainty but death may be expected at 30 g. | * Administration of xanthine derivatives (e.g., aminophylline) may reverse the hemodynamic effects of dipyridamole overdose. Plasma electrolytes and pH should be monitored serially to promote alkaline diuresis of salicylate if renal function is normal. In patients with renal insufficiency or in cases of life-threatening intoxication, dialysis is usually required to treat salicylic overdose, however since [[dipyridamole]] is highly protein bound, dialysis is not likely to remove [[dipyridamole]]. Exchange transfusion may be indicated in infants and young children. | ||
|mechAction=* The antithrombotic action of aspirin and dipyridamole is the result of the additive antiplatelet effects of [[dipyridamole]] and [[aspirin]]. | |||
Treatment of overdose consists primarily of supporting vital functions, increasing drug elimination, and correcting acid-base disturbances. Consider gastric emptying and/or lavage as soon as possible after ingestion, even if the patient has vomited spontaneously. After lavage and/or emesis, administration of activated charcoal as a slurry may be beneficial if less than 3 hours have passed since ingestion. Charcoal absorption should not be employed prior to emesis and lavage. Follow acid-base status closely with serial blood gas and serum pH measurements. Maintain fluid and electrolyte balance. Administer replacement fluid intravenously and augment with correction of acidosis. Treatment may require the use of a vasopressor. Infusion of glucose may be required to control hypoglycemia. | =====Dipyridamole===== | ||
* Dipyridamole inhibits the uptake of adenosine into platelets, [[endothelial cells]] and [[erythrocytes]] in vitro and in vivo; the inhibition occurs in a dose-dependent manner at therapeutic concentrations (0.5–1.9 µg/mL). This inhibition results in an increase in local concentrations of adenosine which acts on the platelet A2-receptor thereby stimulating platelet adenylate cyclase and increasing platelet cyclic-3',5'-adenosine monophosphate (cAMP) levels. Via this mechanism, platelet aggregation is inhibited in response to various stimuli such as platelet activating factor (PAF), collagen and adenosine diphosphate (ADP). | |||
Administration of xanthine derivatives (e.g., aminophylline) may reverse the hemodynamic effects of dipyridamole overdose. Plasma electrolytes and pH should be monitored serially to promote alkaline diuresis of salicylate if renal function is normal. In patients with renal insufficiency or in cases of life-threatening intoxication, dialysis is usually required to treat salicylic overdose, however since dipyridamole is highly protein bound, dialysis is not likely to remove dipyridamole. Exchange transfusion may be indicated in infants and young children. | * Dipyridamole inhibits phosphodiesterase (PDE) in various tissues. While the inhibition of cAMP-PDE is weak, therapeutic levels of dipyridamole inhibit cyclic-3',5'-guanosine monophosphate-PDE (cGMP-PDE), thereby augmenting the increase in cGMP produced by EDRF (endothelium-derived relaxing factor, now identified as nitric oxide). | ||
|mechAction=The antithrombotic action of | =====Aspirin===== | ||
* [[Aspirin]] inhibits platelet aggregation by irreversible inhibition of platelet cyclooxygenase and thus inhibits the generation of [[thromboxane A2]], a powerful inducer of platelet aggregation and [[vasoconstriction]]. | |||
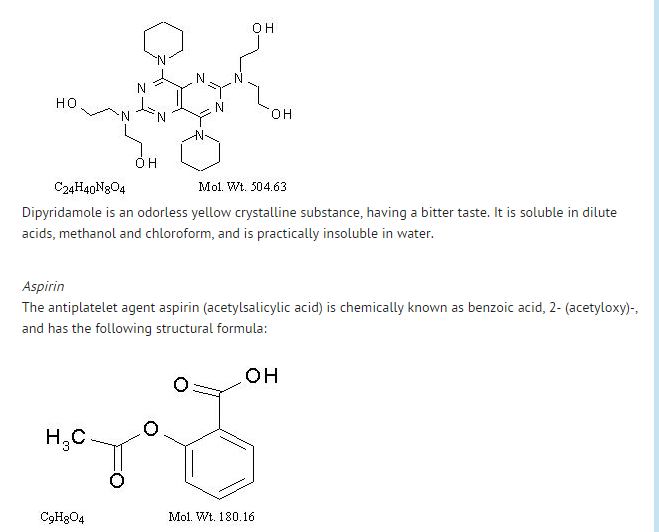
Dipyridamole | |structure=* aspirin and dipyridamole is a combination antiplatelet agent intended for oral administration. Each hard gelatin capsule contains 200 mg dipyridamole in an extended-release form and 25 mg aspirin, as an immediate-release sugar-coated tablet. In addition, each capsule contains the following inactive ingredients: acacia, aluminum stearate, colloidal silicon dioxide, corn starch, dimethicone, hypromellose, hypromellose phthalate, lactose monohydrate, methacrylic acid copolymer, microcrystalline cellulose, povidone, stearic acid, sucrose, talc, tartaric acid, titanium dioxide and triacetin. | ||
Dipyridamole inhibits the uptake of adenosine into platelets, endothelial cells and erythrocytes in vitro and in vivo; the inhibition occurs in a dose-dependent manner at therapeutic concentrations (0.5–1.9 µg/mL). This inhibition results in an increase in local concentrations of adenosine which acts on the platelet A2-receptor thereby stimulating platelet adenylate cyclase and increasing platelet cyclic-3',5'-adenosine monophosphate (cAMP) levels. Via this mechanism, platelet aggregation is inhibited in response to various stimuli such as platelet activating factor (PAF), collagen and adenosine diphosphate (ADP). | * Each capsule shell contains gelatin, red iron oxide and yellow iron oxide, titanium dioxide and water. | ||
=====Dipyridamole===== | |||
Dipyridamole inhibits phosphodiesterase (PDE) in various tissues. While the inhibition of cAMP-PDE is weak, therapeutic levels of dipyridamole inhibit cyclic-3',5'-guanosine monophosphate-PDE (cGMP-PDE), thereby augmenting the increase in cGMP produced by EDRF (endothelium-derived relaxing factor, now identified as nitric oxide). | : [[File:A & D 06 Structure.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
|PD=* The effect of either agent on the other's inhibition of platelet reactivity has not been evaluated. | |||
Aspirin | |PK=* There are no significant interactions between aspirin and dipyridamole. The kinetics of the components are unchanged by their co-administration as aspirin and dipyridamole. | ||
Aspirin inhibits platelet aggregation by irreversible inhibition of platelet cyclooxygenase and thus inhibits the generation of thromboxane A2, a powerful inducer of platelet aggregation and vasoconstriction. | =====Dipyridamole===== | ||
| | ======Absorption====== | ||
* Peak plasma levels of dipyridamole are achieved 2 hours (range 1–6 hours) after administration of a daily dose of 400 mg aspirin and dipyridamole (given as 200 mg BID). The peak plasma concentration at steady-state is 1.98 µg/mL (1.01–3.99 µg/mL) and the steady-state trough concentration is 0.53 µg/mL (0.18–1.01 µg/mL). | |||
=====Effect of Food===== | |||
* When aspirin and dipyridamole capsules were taken with a high fat meal, dipyridamole peak plasma levels (Cmax) and total absorption (AUC) were decreased at steady-state by 20-30% compared to fasting. Due to the similar degree of inhibition of adenosine uptake at these plasma concentrations, this food effect is not considered clinically relevant. | |||
=====Distribution===== | |||
* Dipyridamole is highly lipophilic (log P=3.71, pH=7); however, it has been shown that the drug does not cross the blood-brain barrier to any significant extent in animals. The steady-state volume of distribution of dipyridamole is about 92 L. Approximately 99% of dipyridamole is bound to plasma proteins, predominantly to alpha 1-acid glycoprotein and albumin. | |||
=====Metabolism and Elimination===== | |||
* Dipyridamole is metabolized in the liver, primarily by conjugation with glucuronic acid, of which monoglucuronide which has low pharmacodynamic activity is the primary metabolite. In plasma, about 80% of the total amount is present as parent compound and 20% as monoglucuronide. Most of the glucuronide metabolite (about 95%) is excreted via bile into the feces, with some evidence of enterohepatic circulation. Renal excretion of parent compound is negligible and urinary excretion of the glucuronide metabolite is low (about 5%). With intravenous (i.v.) treatment of dipyridamole, a triphasic profile is obtained: a rapid alpha phase, with a half-life of about 3.4 minutes, a beta phase, with a half-life of about 39 minutes, (which, together with the alpha phase accounts for about 70% of the total area under the curve, AUC) and a prolonged elimination phase λz with a half-life of about 15.5 hours. Due to the extended absorption phase of the dipyridamole component, only the terminal phase is apparent from oral treatment with aspirin and dipyridamole which, in Trial 9.123 was 13.6 hours. | |||
=====Special Populations===== | |||
* Geriatric Patients | |||
:* In ESPS2, plasma concentrations (determined as AUC) of dipyridamole in healthy elderly subjects (>65 years) were about 40% higher than in subjects younger than 55 years receiving treatment with aspirin and dipyridamole. | |||
* Hepatic Dysfunction | |||
:* No study has been conducted with aspirin and dipyridamole in patients with hepatic dysfunction. | |||
* In a study conducted with an intravenous formulation of dipyridamole, patients with mild to severe hepatic insufficiency showed no change in plasma concentrations of dipyridamole but showed an increase in the pharmacologically inactive monoglucuronide metabolite. Dipyridamole can be dosed without restriction as long as there is no evidence of hepatic failure. | |||
* Renal Dysfunction | |||
:* No study has been conducted with aspirin and dipyridamole in patients with renal dysfunction. | |||
* In ESPS2 patients, with creatinine clearances ranging from about 15 mL/min to >100 mL/min, no changes were observed in the pharmacokinetics of dipyridamole or its glucuronide metabolite if data were corrected for differences in age. | |||
=====Aspirin===== | |||
======Absorption====== | |||
* Peak plasma levels of aspirin are achieved 0.63 hours (0.5–1 hour) after administration of a 50 mg aspirin daily dose from aspirin and dipyridamole (given as 25 mg BID). The peak plasma concentration at steady-state is 319 ng/mL (175–463 ng/mL). Aspirin undergoes moderate hydrolysis to salicylic acid in the liver and the gastrointestinal wall, with 50%–75% of an administered dose reaching the systemic circulation as intact aspirin. | |||
=====Effect of Food===== | |||
* When aspirin and dipyridamole capsules were taken with a high fat meal, there was no difference for aspirin in AUC at steady-state, and the approximately 50% decrease in Cmax was not considered clinically relevant based on a similar degree of cyclooxygenase inhibition comparing the fed and fasted state. | |||
=====Distribution===== | |||
* Aspirin is poorly bound to plasma proteins and its apparent volume of distribution is low (10 L). Its metabolite, salicylic acid, is highly bound to plasma proteins, but its binding is concentration-dependent (nonlinear). At low concentrations (<100 µg/mL), approximately 90% of salicylic acid is bound to albumin. Salicylic acid is widely distributed to all tissues and fluids in the body, including the central nervous system, breast milk, and fetal tissues. Early signs of salicylate overdose (salicylism), including tinnitus (ringing in the ears), occur at plasma concentrations approximating 200 µg/mL. | |||
=====Metabolism and Elimination===== | |||
* Aspirin is rapidly hydrolyzed in plasma to salicylic acid, with a half-life of 20 minutes. Plasma levels of aspirin are essentially undetectable 2–2.5 hours after dosing and peak salicylic acid concentrations occur 1 hour (range: 0.5–2 hours) after administration of aspirin. Salicylic acid is primarily conjugated in the liver to form salicyluric acid, a phenolic glucuronide, an acyl glucuronide, and a number of minor metabolites. Salicylate metabolism is saturable and total body clearance decreases at higher serum concentrations due to the limited ability of the liver to form both salicyluric acid and phenolic glucuronide. Following toxic doses (10–20 g), the plasma half-life may be increased to over 20 hours. | |||
* The elimination of acetylsalicylic acid follows first-order kinetics with aspirin and dipyridamole and has a half-life of 0.33 hours. The half-life of salicylic acid is 1.71 hours. Both values correspond well with data from the literature at lower doses which state a resultant half-life of approximately 2–3 hours. At higher doses, the elimination of salicylic acid follows zero-order kinetics (i.e., the rate of elimination is constant in relation to plasma concentration), with an apparent half-life of 6 hours or higher. Renal excretion of unchanged drug depends upon urinary pH. As urinary pH rises above 6.5, the renal clearance of free salicylate increases from <5% to >80%. Alkalinization of the urine is a key concept in the management of salicylate overdose. Following therapeutic doses, about 10% is excreted as salicylic acid and 75% as salicyluric acid, as the phenolic and acyl glucuronides, in urine. | |||
=====Special Populations===== | |||
* Hepatic Dysfunction | |||
:* Avoid aspirin in patients with severe hepatic insufficiency. | |||
* Renal Dysfunction | |||
:* Avoid aspirin in patients with severe renal failure (glomerular filtration rate less than 10 mL/min). | |||
=====Aspirin and dipyridamole===== | |||
======Drug Interaction====== | |||
* A dedicated drug interaction study was conducted in 60 healthy volunteers to evaluate the effects of omeprazole 80 mg administered once daily on the pharmacokinetics (PK) of dipyridamole and the pharmacodynamics (PD) of acetylsalicylic acid when co-administered with aspirin and dipyridamole twice daily. Dipyridamole exposure (Cmax and AUC) at steady-state were similar with or without omeprazole co-administration. The pharmacokinetics of acetylsalicylic acid was not characterized. However, the antiplatelet activity as measured by arachidonic acid induced platelet aggregation was similar between the treatment arms at steady-state. | |||
|nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | |||
* In studies in which dipyridamole was administered in the feed to mice (up to 111 weeks in males and females) and rats (up to 128 weeks in males and up to 142 weeks in females), there was no evidence of drug-related carcinogenesis. The highest dose administered in these studies (75 mg/kg/day) was, on a mg/m2 basis, about equivalent to the maximum recommended daily human oral dose (MRHD) in mice and about twice the MRHD in rats. | |||
* Combinations of dipyridamole and aspirin (1:5 ratio) tested negative in the Ames test, in vivo chromosome aberration tests (in mice and hamsters), oral micronucleus tests (in mice and hamsters) and oral dominant lethal test (in mice). Aspirin, alone, induced chromosome aberrations in cultured human fibroblasts. Mutagenicity tests of dipyridamole alone with bacterial and mammalian cell systems were negative. | |||
* Combinations of dipyridamole and aspirin have not been evaluated for effects on fertility and reproductive performance. There was no evidence of impaired fertility when [[dipyridamole]] was administered to male and female rats at oral doses up to 500 mg/kg/day (about 12 times the MRHD on a mg/m2 basis). A significant reduction in number of [[corpora lutea]] with consequent reduction in implantations and live fetuses was, however, observed at 1250 mg/kg (more than 30 times the MRHD on a mg/m2 basis). Aspirin inhibits ovulation in rats. | |||
Aspirin is | |clinicalStudies=* ESPS2 (European Stroke Prevention Study 2) was a double-blind, placebo-controlled, 24-month study in which 6602 patients over the age of 18 years had an ischemic stroke (76%) or transient ischemic attack (TIA, 24%) within three months prior to entry. Patients were enrolled in 13 European countries between February 1989 and May 1995 and were randomized to one of four treatment groups: aspirin and dipyridamole (aspirin/extended-release dipyridamole) 25 mg/200 mg; extended-release dipyridamole (ER-DP) 200 mg alone; aspirin (ASA) 25 mg alone; or placebo. The mean age in this population was 66.7 years with 58% of them being males. Patients received one capsule twice daily (morning and evening). Efficacy assessments included analyses of stroke (fatal or nonfatal) and death (from all causes) as confirmed by a blinded morbidity and mortality assessment group. There were no differences with regard to efficacy based on age or gender; patients who were older had a trend towards more events. | ||
=====Stroke Endpoint===== | |||
* Aspirin and dipyridamole reduced the risk of stroke by 22.1% compared to aspirin 50 mg/day alone (p = 0.008) and reduced the risk of stroke by 24.4% compared to extended-release dipyridamole 400 mg/day alone (p = 0.002) (Table 3). aspirin and dipyridamole reduced the risk of stroke by 36.8% compared to placebo (p <0.001) | |||
: [[File:A & D Clinical 05.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
=====Combined Stroke or Death Endpoint===== | |||
* In ESPS2, aspirin and dipyridamole reduced the risk of stroke or death by 12.1% compared to aspirin alone and by 10.3% compared to extended-release dipyridamole alone. These results were not statistically significant. aspirin and dipyridamole reduced the risk of stroke or death by 24.2% compared to placebo. | |||
=====Death Endpoint===== | |||
* The incidence rate of all cause mortality was 11.3% for aspirin and dipyridamole, 11.0% for aspirin alone, 11.4% for extended-release dipyridamole alone and 12.3% for placebo alone. The differences between the aspirin and dipyridamole, aspirin alone and extended-release [[dipyridamole]] alone treatment groups were not statistically significant. These incidence rates for aspirin and dipyridamole and aspirin alone are consistent with previous [[aspirin]] studies in stroke and TIA patients. | |||
|howSupplied=* aspirin and dipyridamole capsules are available as a hard gelatin capsule, with a red cap and an ivory-colored body, containing yellow extended-release pellets incorporating dipyridamole and a round white tablet incorporating immediate-release [[aspirin]]. The capsule body is imprinted in red with the Boehringer Ingelheim logo and with "01A". | |||
* Aspirin and dipyridamole capsules are supplied in unit-of-use bottles of 60 capsules (NDC 0597-0001-60). | |||
|storage=* Store at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F). Protect from excessive moisture. | |||
|packLabel=[[File:A & D 01.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
[[File:A & D 02.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
In studies in which dipyridamole was administered in the feed to mice (up to 111 weeks in males and females) and rats (up to 128 weeks in males and up to 142 weeks in females), there was no evidence of drug-related carcinogenesis. The highest dose administered in these studies (75 mg/kg/day) was, on a mg/m2 basis, about equivalent to the maximum recommended daily human oral dose (MRHD) in mice and about twice the MRHD in rats. | [[File:A & D 04.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
|fdaPatientInfo======Risk of Bleeding===== | |||
Combinations of dipyridamole and aspirin (1:5 ratio) tested negative in the Ames test, in vivo chromosome aberration tests (in mice and hamsters), oral micronucleus tests (in mice and hamsters) and oral dominant lethal test (in mice). Aspirin, alone, induced chromosome aberrations in cultured human fibroblasts. Mutagenicity tests of dipyridamole alone with bacterial and mammalian cell systems were negative. | * Inform patients that as with other [[antiplatelet agents]], there is a general risk of bleeding including intracranial and gastrointestinal bleeding. Inform patients about the signs and symptoms of bleeding, including occult bleeding. Tell patients to notify their physician if they are prescribed any drug which may increase risk of bleeding. | ||
* Counsel patients who consume three or more alcoholic drinks daily about the bleeding risks involved with chronic, heavy alcohol use while taking aspirin. | |||
Combinations of dipyridamole and aspirin have not been evaluated for effects on fertility and reproductive performance. There was no evidence of impaired fertility when dipyridamole was administered to male and female rats at oral doses up to 500 mg/kg/day (about 12 times the MRHD on a mg/m2 basis). A significant reduction in number of corpora lutea with consequent reduction in implantations and live fetuses was, however, observed at 1250 mg/kg (more than 30 times the MRHD on a mg/m2 basis). Aspirin inhibits ovulation in rats. | =====Pregnancy===== | ||
|clinicalStudies=ESPS2 (European Stroke Prevention Study 2) was a double-blind, placebo-controlled, 24-month study in which 6602 patients over the age of 18 years had an ischemic stroke (76%) or transient ischemic attack (TIA, 24%) within three months prior to entry. Patients were enrolled in 13 European countries between February 1989 and May 1995 and were randomized to one of four treatment groups: | * Inform patients that aspirin is known to be harmful to fetuses and ask the patient to notify them if they are or become pregnant. | ||
=====Headaches===== | |||
Stroke Endpoint | * Some patients may experience headaches upon treatment initiation; these are usually transient. In case of intolerable headaches, tell the patient to contact their physician. | ||
=====Dosage and Administration===== | |||
: [[File: | * Tell patients that aspirin and dipyridamole capsules should be swallowed whole, and not chewed or crushed. If you miss a dose, continue with your next dose on your regular schedule. Do not take a double dose. | ||
=====Storage===== | |||
In ESPS2, | * Inform patients to protect aspirin and dipyridamole from moisture. | ||
|alcohol=* Alcohol-Aspirin and dipyridamole interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |||
Death Endpoint | |brandNames=* AGGRENOX ®<ref>{{Cite web | title = AGGRENOX- aspirin and dipyridamole capsule | url =http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=938ab0b5-8377-404a-8f61-5c630bda5932 }}</ref> | ||
The incidence rate of all cause mortality was 11.3% for | |||
|howSupplied= | |||
|storage=Store at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F) | |||
| | |||
Inform patients that | |||
Inform patients to protect | |||
|alcohol=Alcohol-Aspirin and dipyridamole interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |||
|brandNames=*AGGRENOX ®<ref>{{Cite web | title = | |||
<!--Look-Alike Drug Names--> | |||
}} | }} | ||
[[Category:drugs]] | |||
Latest revision as of 03:59, 9 March 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Aspirin and dipyridamole is a platelet aggregation inhibitor that is FDA approved for the prophylaxis of to reduce the risk of stroke in patients who have had transient ischemia of the brain or completed ischemic stroke due to thrombosis. Common adverse reactions include abdominal pain, diarrhea, headache, arthralgia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- To reduce the risk of stroke in patients who have had transient ischemia of the brain or completed ischemic stroke due to thrombosis.
- Aspirin and dipyridamole is not interchangeable with the individual components of aspirin and dipyridamole tablets.
- The recommended dose of aspirin and dipyridamole is one capsule given orally twice daily, one in the morning and one in the evening. Swallow capsules whole without chewing. aspirin and dipyridamole can be administered with or without food.
Alternative Regimen in Case of Intolerable Headaches
- In the event of intolerable headaches during initial treatment, switch to one capsule at bedtime and low-dose aspirin in the morning. Because there are no outcome data with this regimen and headaches become less of a problem as treatment continues, patients should return to the usual regimen as soon as possible, usually within one week.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Aspirin and dipyridamole in adult patients.
Non–Guideline-Supported Use
- Hemodialysis - Thrombosis; Prophylaxis[1]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Aspirin and dipyridamole FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Aspirin and dipyridamole in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Aspirin and dipyridamole in pediatric patients.
Contraindications
Hypersensitivity
- Aspirin and dipyridamole is contraindicated in patients with known hypersensitivity to any of the product components.
Allergy
- Aspirin is contraindicated in patients with known allergy to nonsteroidal anti-inflammatory drug products and in patients with the syndrome of asthma, rhinitis, and nasal polyps. Aspirin may cause severe urticaria, angioedema or bronchospasm.
Reye Syndrome
- Do not use aspirin in children or teenagers with viral infections because of the risk of Reye syndrome.
Warnings
Hypersensitivity
- Aspirin and dipyridamole is contraindicated in patients with known hypersensitivity to any of the product components.
Allergy
- Aspirin is contraindicated in patients with known allergy to nonsteroidal anti-inflammatory drug products and in patients with the syndrome of asthma, rhinitis, and nasal polyps. Aspirin may cause severe urticaria, angioedema or bronchospasm.
Reye Syndrome
- Do not use aspirin in children or teenagers with viral infections because of the risk of Reye syndrome.
Adverse Reactions
Clinical Trials Experience
- The following adverse reactions are discussed elsewhere in the labeling:
- Hypersensitivity.
- Allergy.
- Risk of bleeding.
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The efficacy and safety of aspirin and dipyridamole was established in the European Stroke Prevention Study-2 (ESPS2). ESPS2 was a double-blind, placebo controlled study that evaluated 6602 patients over the age of 18 years who had a previous ischemic stroke or transient ischemic attack within ninety days prior to entry. Patients were randomized to either aspirin and dipyridamole, aspirin, ER-DP, or placebo; primary endpoints included stroke (fatal or nonfatal) and death from all causes.
- This 24-month, multicenter, double-blind, randomized study (ESPS2) was conducted to compare the efficacy and safety of aspirin and dipyridamole with placebo, extended-release dipyridamole alone and aspirin alone. The study was conducted in a total of 6602 male and female patients who had experienced a previous ischemic stroke or transient ischemia of the brain within three months prior to randomization.
- Table 1 presents the incidence of adverse events that occurred in 1% or more of patients treated with aspirin and dipyridamole where the incidence was also greater than in those patients treated with placebo. There is no clear benefit of the dipyridamole/aspirin combination over aspirin with respect to safety.
- Headache was most notable in the first month of treatment.
Other Adverse Events
- Adverse reactions that occurred in less than 1% of patients treated with aspirin and dipyridamole in the ESPS2 study and that were medically judged to be possibly related to either dipyridamole or aspirin are listed below.
- Body as a Whole
- Allergic reaction, fever
- Cardiovascular
- Gastritis ulceration and perforation
- Hearing and Vestibular Disorders
- Heart rate and rhythm disorders
- Liver and biliary system disorders
- Cholelithiasis, jaundice, hepatic function abnormal
- Metabolic and Nutritional Disorders
- Hyperglycemia, thirst
- Platelet, bleeding and clotting disorders
- Psychiatric disorders
- Reproductive
- Respiratory
- Special Senses Other Disorders
- Skin and appendages disorders
- Renal insufficiency and failure, hematuria
- Vascular (Extracardiac) Disorders
Laboratory Changes
- Over the course of the 24-month study (ESPS2), patients treated with aspirin and dipyridamole showed a decline (mean change from baseline) in hemoglobin of 0.25 g/dL, hematocrit of 0.75%, and erythrocyte count of 0.13x106/mm3.
Postmarketing Experience
- The following is a list of additional adverse reactions that have been reported either in the literature or are from post-marketing spontaneous reports for either dipyridamole or aspirin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) strength of causal connection to aspirin and dipyridamole.
- Body as a Whole
- Cardiovascular
- Central Nervous System
- Fluid and electrolyte
- Gastrointestinal
- Hearing and Vestibular Disorders
- Immune System Disorders
- Liver and Biliary System Disorders
- Musculoskeletal
- Metabolic and Nutritional Disorders
- Platelet, Bleeding and Clotting Disorders
- Prolongation of the prothrombin time, disseminated intravascular coagulation, coagulopathy, thrombocytopenia
- Reproductive
- Prolonged pregnancy and labor, stillbirths, lower birth weight infants, antepartum and postpartum bleeding
- Respiratory
- Skin and Appendages Disorders
- Rash, alopecia, angioedema, Stevens-Johnson syndrome, skin hemorrhages such as bruising, ecchymosis, and hematoma
- Vascular (Extracardiac Disorders)
- Other Adverse Events
Drug Interactions
Drug Interaction Study Information Obtained From Literature
- Dipyridamole has been reported to increase the plasma levels and cardiovascular effects of adenosine. Adjustment of adenosine dosage may be necessary.
Angiotensin Converting Enzyme (ACE) Inhibitors
- Due to the indirect effect of aspirin on the renin-angiotensin conversion pathway, the hyponatremic and hypotensive effects of ACE inhibitors may be diminished by concomitant administration of aspirin.
- Acetazolamide
- Concurrent use of aspirin and acetazolamide can lead to high serum concentrations of acetazolamide (and toxicity) due to competition at the renal tubule for secretion.
Anticoagulants and Antiplatelets
- Patients taking aspirin and dipyridamole in combination with anticoagulants, antiplatelets, or any substance impacting coagulation are at increased risk for bleeding. Aspirin can displace warfarin from protein binding sites, leading to prolongation of both the prothrombin time and the bleeding time. Aspirin can increase the anticoagulant activity of heparin, increasing bleeding risk.
Anticonvulsants
- Salicylic acid can displace protein-bound phenytoin and valproic acid, leading to a decrease in the total concentration of phenytoin and an increase in serum valproic acid levels.
Beta Blockers
- The hypotensive effects of beta blockers may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention.
Cholinesterase Inhibitors
- Dipyridamole may counteract the anticholinesterase effect of cholinesterase inhibitors, thereby potentially aggravating myasthenia gravis.
Diuretics
- The effectiveness of diuretics in patients with underlying renal or cardiovascular disease may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention.
Methotrexate
- Salicylate can inhibit renal clearance of methotrexate, leading to bone marrow toxicity, especially in the elderly or renal impaired.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- The concurrent use of aspirin with other NSAIDs may increase bleeding or lead to decreased renal function.
Oral Hypoglycemics
- Moderate doses of aspirin may increase the effectiveness of oral hypoglycemic drugs, leading to hypoglycemia.
Uricosuric Agents (probenecid and sulfinpyrazone)
- Salicylates antagonize the uricosuric action of uricosuric agents.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): D
There is no FDA guidance on usage of Aspirin and dipyridamole in women who are pregnant.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Aspirin and dipyridamole in women who are pregnant.
Labor and Delivery
- Aspirin can result in excessive blood loss at delivery as well as prolonged gestation and prolonged labor. Because of these effects on the mother and because of adverse fetal effects seen with aspirin during the later stages of pregnancy, avoid aspirin and dipyridamole in the third trimester of pregnancy and during labor and delivery.
Nursing Mothers
- Both dipyridamole and aspirin are excreted in human milk. Exercise caution when aspirin and dipyridamole capsules are administered to a nursing woman.
Pediatric Use
- Safety and effectiveness of aspirin and dipyridamole in pediatric patients have not been studied. Due to the aspirin component, use of this product in the pediatric population is not recommended
Geriatic Use
- Of the total number of subjects in ESPS2, 61 percent were 65 and over, while 27 percent were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out
Gender
There is no FDA guidance on the use of Aspirin and dipyridamole with respect to specific gender populations.
Race
There is no FDA guidance on the use of Aspirin and dipyridamole with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Aspirin and dipyridamole in patients with renal impairment.
Hepatic Impairment
- aspirin and dipyridamole has not been studied in patients with hepatic or renal impairment. Avoid using aspirin containing products, such as aspirin and dipyridamole in patients with severe hepatic or severe renal (glomerular filtration rate < 10 mL/min) dysfunction
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Aspirin and dipyridamole in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Aspirin and dipyridamole in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
- Plasma electrolytes and pH should be monitored serially to promote alkaline diuresis of salicylate if renal function is normal. In patients with renal insufficiency or in cases of life-threatening intoxication, dialysis is usually required to treat salicylic overdose, however since dipyridamole is highly protein bound, dialysis is not likely to remove dipyridamole.
IV Compatibility
There is limited information regarding the compatibility of Aspirin and dipyridamole and IV administrations.
Overdosage
- Because of the dose ratio of dipyridamole to aspirin, overdosage of aspirin and dipyridamole is likely to be dominated by signs and symptoms of dipyridamole overdose. In case of real or suspected overdose, seek medical attention or contact a Poison Control Center immediately. Careful medical management is essential.
- Based upon the known hemodynamic effects of dipyridamole, symptoms such as warm feeling, flushes, sweating, restlessness, feeling of weakness and dizziness may occur. A drop in blood pressure and tachycardia might also be observed.
- Salicylate toxicity may result from acute ingestion (overdose) or chronic intoxication. Severity of aspirin intoxication is determined by measuring the blood salicylate level. The early signs of salicylic overdose (salicylism), including tinnitus (ringing in the ears), occur at plasma concentrations approaching 200 µg/mL. In severe cases, hyperthermia and hypovolemia are the major immediate threats to life. Plasma concentrations of aspirin above 300 µg/mL are clearly toxic. Severe toxic effects are associated with levels above 400 µg/mL. A single lethal dose of aspirin in adults is not known with certainty but death may be expected at 30 g.
- Treatment of overdose consists primarily of supporting vital functions, increasing drug elimination, and correcting acid-base disturbances. Consider gastric emptying and/or lavage as soon as possible after ingestion, even if the patient has vomited spontaneously. After lavage and/or emesis, administration of activated charcoal as a slurry may be beneficial if less than 3 hours have passed since ingestion. Charcoal absorption should not be employed prior to emesis and lavage. Follow acid-base status closely with serial blood gas and serum pH measurements. Maintain fluid and electrolyte balance. Administer replacement fluid intravenously and augment with correction of acidosis. Treatment may require the use of a vasopressor. Infusion of glucose may be required to control hypoglycemia.
- Administration of xanthine derivatives (e.g., aminophylline) may reverse the hemodynamic effects of dipyridamole overdose. Plasma electrolytes and pH should be monitored serially to promote alkaline diuresis of salicylate if renal function is normal. In patients with renal insufficiency or in cases of life-threatening intoxication, dialysis is usually required to treat salicylic overdose, however since dipyridamole is highly protein bound, dialysis is not likely to remove dipyridamole. Exchange transfusion may be indicated in infants and young children.
Pharmacology
There is limited information regarding Aspirin and dipyridamole Pharmacology in the drug label.
Mechanism of Action
- The antithrombotic action of aspirin and dipyridamole is the result of the additive antiplatelet effects of dipyridamole and aspirin.
Dipyridamole
- Dipyridamole inhibits the uptake of adenosine into platelets, endothelial cells and erythrocytes in vitro and in vivo; the inhibition occurs in a dose-dependent manner at therapeutic concentrations (0.5–1.9 µg/mL). This inhibition results in an increase in local concentrations of adenosine which acts on the platelet A2-receptor thereby stimulating platelet adenylate cyclase and increasing platelet cyclic-3',5'-adenosine monophosphate (cAMP) levels. Via this mechanism, platelet aggregation is inhibited in response to various stimuli such as platelet activating factor (PAF), collagen and adenosine diphosphate (ADP).
- Dipyridamole inhibits phosphodiesterase (PDE) in various tissues. While the inhibition of cAMP-PDE is weak, therapeutic levels of dipyridamole inhibit cyclic-3',5'-guanosine monophosphate-PDE (cGMP-PDE), thereby augmenting the increase in cGMP produced by EDRF (endothelium-derived relaxing factor, now identified as nitric oxide).
Aspirin
- Aspirin inhibits platelet aggregation by irreversible inhibition of platelet cyclooxygenase and thus inhibits the generation of thromboxane A2, a powerful inducer of platelet aggregation and vasoconstriction.
Structure
- aspirin and dipyridamole is a combination antiplatelet agent intended for oral administration. Each hard gelatin capsule contains 200 mg dipyridamole in an extended-release form and 25 mg aspirin, as an immediate-release sugar-coated tablet. In addition, each capsule contains the following inactive ingredients: acacia, aluminum stearate, colloidal silicon dioxide, corn starch, dimethicone, hypromellose, hypromellose phthalate, lactose monohydrate, methacrylic acid copolymer, microcrystalline cellulose, povidone, stearic acid, sucrose, talc, tartaric acid, titanium dioxide and triacetin.
- Each capsule shell contains gelatin, red iron oxide and yellow iron oxide, titanium dioxide and water.
Dipyridamole
Pharmacodynamics
- The effect of either agent on the other's inhibition of platelet reactivity has not been evaluated.
Pharmacokinetics
- There are no significant interactions between aspirin and dipyridamole. The kinetics of the components are unchanged by their co-administration as aspirin and dipyridamole.
Dipyridamole
Absorption
- Peak plasma levels of dipyridamole are achieved 2 hours (range 1–6 hours) after administration of a daily dose of 400 mg aspirin and dipyridamole (given as 200 mg BID). The peak plasma concentration at steady-state is 1.98 µg/mL (1.01–3.99 µg/mL) and the steady-state trough concentration is 0.53 µg/mL (0.18–1.01 µg/mL).
Effect of Food
- When aspirin and dipyridamole capsules were taken with a high fat meal, dipyridamole peak plasma levels (Cmax) and total absorption (AUC) were decreased at steady-state by 20-30% compared to fasting. Due to the similar degree of inhibition of adenosine uptake at these plasma concentrations, this food effect is not considered clinically relevant.
Distribution
- Dipyridamole is highly lipophilic (log P=3.71, pH=7); however, it has been shown that the drug does not cross the blood-brain barrier to any significant extent in animals. The steady-state volume of distribution of dipyridamole is about 92 L. Approximately 99% of dipyridamole is bound to plasma proteins, predominantly to alpha 1-acid glycoprotein and albumin.
Metabolism and Elimination
- Dipyridamole is metabolized in the liver, primarily by conjugation with glucuronic acid, of which monoglucuronide which has low pharmacodynamic activity is the primary metabolite. In plasma, about 80% of the total amount is present as parent compound and 20% as monoglucuronide. Most of the glucuronide metabolite (about 95%) is excreted via bile into the feces, with some evidence of enterohepatic circulation. Renal excretion of parent compound is negligible and urinary excretion of the glucuronide metabolite is low (about 5%). With intravenous (i.v.) treatment of dipyridamole, a triphasic profile is obtained: a rapid alpha phase, with a half-life of about 3.4 minutes, a beta phase, with a half-life of about 39 minutes, (which, together with the alpha phase accounts for about 70% of the total area under the curve, AUC) and a prolonged elimination phase λz with a half-life of about 15.5 hours. Due to the extended absorption phase of the dipyridamole component, only the terminal phase is apparent from oral treatment with aspirin and dipyridamole which, in Trial 9.123 was 13.6 hours.
Special Populations
- Geriatric Patients
- In ESPS2, plasma concentrations (determined as AUC) of dipyridamole in healthy elderly subjects (>65 years) were about 40% higher than in subjects younger than 55 years receiving treatment with aspirin and dipyridamole.
- Hepatic Dysfunction
- No study has been conducted with aspirin and dipyridamole in patients with hepatic dysfunction.
- In a study conducted with an intravenous formulation of dipyridamole, patients with mild to severe hepatic insufficiency showed no change in plasma concentrations of dipyridamole but showed an increase in the pharmacologically inactive monoglucuronide metabolite. Dipyridamole can be dosed without restriction as long as there is no evidence of hepatic failure.
- Renal Dysfunction
- No study has been conducted with aspirin and dipyridamole in patients with renal dysfunction.
- In ESPS2 patients, with creatinine clearances ranging from about 15 mL/min to >100 mL/min, no changes were observed in the pharmacokinetics of dipyridamole or its glucuronide metabolite if data were corrected for differences in age.
Aspirin
Absorption
- Peak plasma levels of aspirin are achieved 0.63 hours (0.5–1 hour) after administration of a 50 mg aspirin daily dose from aspirin and dipyridamole (given as 25 mg BID). The peak plasma concentration at steady-state is 319 ng/mL (175–463 ng/mL). Aspirin undergoes moderate hydrolysis to salicylic acid in the liver and the gastrointestinal wall, with 50%–75% of an administered dose reaching the systemic circulation as intact aspirin.
Effect of Food
- When aspirin and dipyridamole capsules were taken with a high fat meal, there was no difference for aspirin in AUC at steady-state, and the approximately 50% decrease in Cmax was not considered clinically relevant based on a similar degree of cyclooxygenase inhibition comparing the fed and fasted state.
Distribution
- Aspirin is poorly bound to plasma proteins and its apparent volume of distribution is low (10 L). Its metabolite, salicylic acid, is highly bound to plasma proteins, but its binding is concentration-dependent (nonlinear). At low concentrations (<100 µg/mL), approximately 90% of salicylic acid is bound to albumin. Salicylic acid is widely distributed to all tissues and fluids in the body, including the central nervous system, breast milk, and fetal tissues. Early signs of salicylate overdose (salicylism), including tinnitus (ringing in the ears), occur at plasma concentrations approximating 200 µg/mL.
Metabolism and Elimination
- Aspirin is rapidly hydrolyzed in plasma to salicylic acid, with a half-life of 20 minutes. Plasma levels of aspirin are essentially undetectable 2–2.5 hours after dosing and peak salicylic acid concentrations occur 1 hour (range: 0.5–2 hours) after administration of aspirin. Salicylic acid is primarily conjugated in the liver to form salicyluric acid, a phenolic glucuronide, an acyl glucuronide, and a number of minor metabolites. Salicylate metabolism is saturable and total body clearance decreases at higher serum concentrations due to the limited ability of the liver to form both salicyluric acid and phenolic glucuronide. Following toxic doses (10–20 g), the plasma half-life may be increased to over 20 hours.
- The elimination of acetylsalicylic acid follows first-order kinetics with aspirin and dipyridamole and has a half-life of 0.33 hours. The half-life of salicylic acid is 1.71 hours. Both values correspond well with data from the literature at lower doses which state a resultant half-life of approximately 2–3 hours. At higher doses, the elimination of salicylic acid follows zero-order kinetics (i.e., the rate of elimination is constant in relation to plasma concentration), with an apparent half-life of 6 hours or higher. Renal excretion of unchanged drug depends upon urinary pH. As urinary pH rises above 6.5, the renal clearance of free salicylate increases from <5% to >80%. Alkalinization of the urine is a key concept in the management of salicylate overdose. Following therapeutic doses, about 10% is excreted as salicylic acid and 75% as salicyluric acid, as the phenolic and acyl glucuronides, in urine.
Special Populations
- Hepatic Dysfunction
- Avoid aspirin in patients with severe hepatic insufficiency.
- Renal Dysfunction
- Avoid aspirin in patients with severe renal failure (glomerular filtration rate less than 10 mL/min).
Aspirin and dipyridamole
Drug Interaction
- A dedicated drug interaction study was conducted in 60 healthy volunteers to evaluate the effects of omeprazole 80 mg administered once daily on the pharmacokinetics (PK) of dipyridamole and the pharmacodynamics (PD) of acetylsalicylic acid when co-administered with aspirin and dipyridamole twice daily. Dipyridamole exposure (Cmax and AUC) at steady-state were similar with or without omeprazole co-administration. The pharmacokinetics of acetylsalicylic acid was not characterized. However, the antiplatelet activity as measured by arachidonic acid induced platelet aggregation was similar between the treatment arms at steady-state.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- In studies in which dipyridamole was administered in the feed to mice (up to 111 weeks in males and females) and rats (up to 128 weeks in males and up to 142 weeks in females), there was no evidence of drug-related carcinogenesis. The highest dose administered in these studies (75 mg/kg/day) was, on a mg/m2 basis, about equivalent to the maximum recommended daily human oral dose (MRHD) in mice and about twice the MRHD in rats.
- Combinations of dipyridamole and aspirin (1:5 ratio) tested negative in the Ames test, in vivo chromosome aberration tests (in mice and hamsters), oral micronucleus tests (in mice and hamsters) and oral dominant lethal test (in mice). Aspirin, alone, induced chromosome aberrations in cultured human fibroblasts. Mutagenicity tests of dipyridamole alone with bacterial and mammalian cell systems were negative.
- Combinations of dipyridamole and aspirin have not been evaluated for effects on fertility and reproductive performance. There was no evidence of impaired fertility when dipyridamole was administered to male and female rats at oral doses up to 500 mg/kg/day (about 12 times the MRHD on a mg/m2 basis). A significant reduction in number of corpora lutea with consequent reduction in implantations and live fetuses was, however, observed at 1250 mg/kg (more than 30 times the MRHD on a mg/m2 basis). Aspirin inhibits ovulation in rats.
Clinical Studies
- ESPS2 (European Stroke Prevention Study 2) was a double-blind, placebo-controlled, 24-month study in which 6602 patients over the age of 18 years had an ischemic stroke (76%) or transient ischemic attack (TIA, 24%) within three months prior to entry. Patients were enrolled in 13 European countries between February 1989 and May 1995 and were randomized to one of four treatment groups: aspirin and dipyridamole (aspirin/extended-release dipyridamole) 25 mg/200 mg; extended-release dipyridamole (ER-DP) 200 mg alone; aspirin (ASA) 25 mg alone; or placebo. The mean age in this population was 66.7 years with 58% of them being males. Patients received one capsule twice daily (morning and evening). Efficacy assessments included analyses of stroke (fatal or nonfatal) and death (from all causes) as confirmed by a blinded morbidity and mortality assessment group. There were no differences with regard to efficacy based on age or gender; patients who were older had a trend towards more events.
Stroke Endpoint
- Aspirin and dipyridamole reduced the risk of stroke by 22.1% compared to aspirin 50 mg/day alone (p = 0.008) and reduced the risk of stroke by 24.4% compared to extended-release dipyridamole 400 mg/day alone (p = 0.002) (Table 3). aspirin and dipyridamole reduced the risk of stroke by 36.8% compared to placebo (p <0.001)
Combined Stroke or Death Endpoint
- In ESPS2, aspirin and dipyridamole reduced the risk of stroke or death by 12.1% compared to aspirin alone and by 10.3% compared to extended-release dipyridamole alone. These results were not statistically significant. aspirin and dipyridamole reduced the risk of stroke or death by 24.2% compared to placebo.
Death Endpoint
- The incidence rate of all cause mortality was 11.3% for aspirin and dipyridamole, 11.0% for aspirin alone, 11.4% for extended-release dipyridamole alone and 12.3% for placebo alone. The differences between the aspirin and dipyridamole, aspirin alone and extended-release dipyridamole alone treatment groups were not statistically significant. These incidence rates for aspirin and dipyridamole and aspirin alone are consistent with previous aspirin studies in stroke and TIA patients.
How Supplied
- aspirin and dipyridamole capsules are available as a hard gelatin capsule, with a red cap and an ivory-colored body, containing yellow extended-release pellets incorporating dipyridamole and a round white tablet incorporating immediate-release aspirin. The capsule body is imprinted in red with the Boehringer Ingelheim logo and with "01A".
- Aspirin and dipyridamole capsules are supplied in unit-of-use bottles of 60 capsules (NDC 0597-0001-60).
Storage
- Store at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F). Protect from excessive moisture.
Images
Drug Images
{{#ask: Page Name::Aspirin and dipyridamole |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
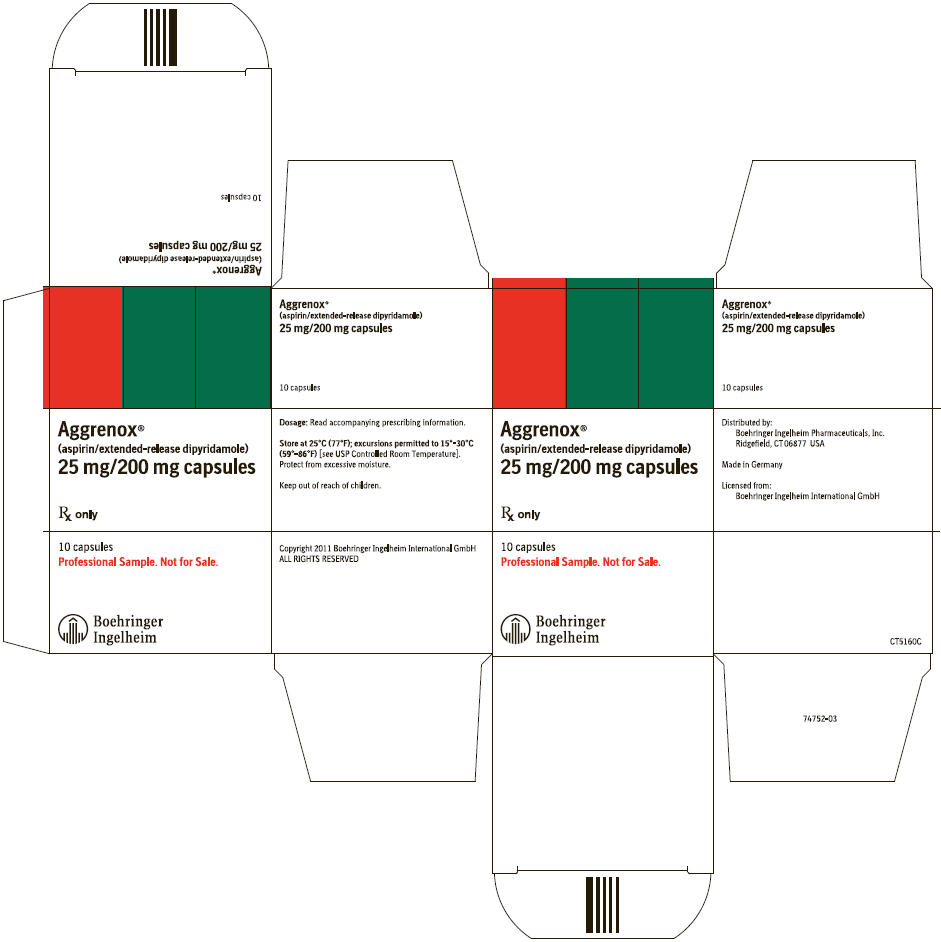
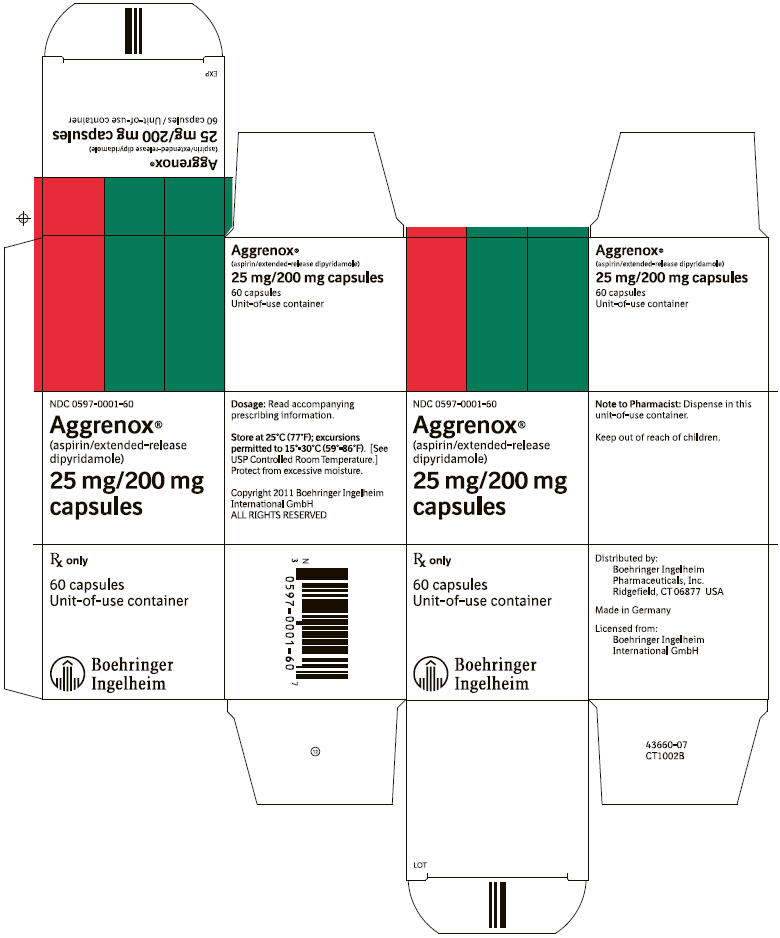
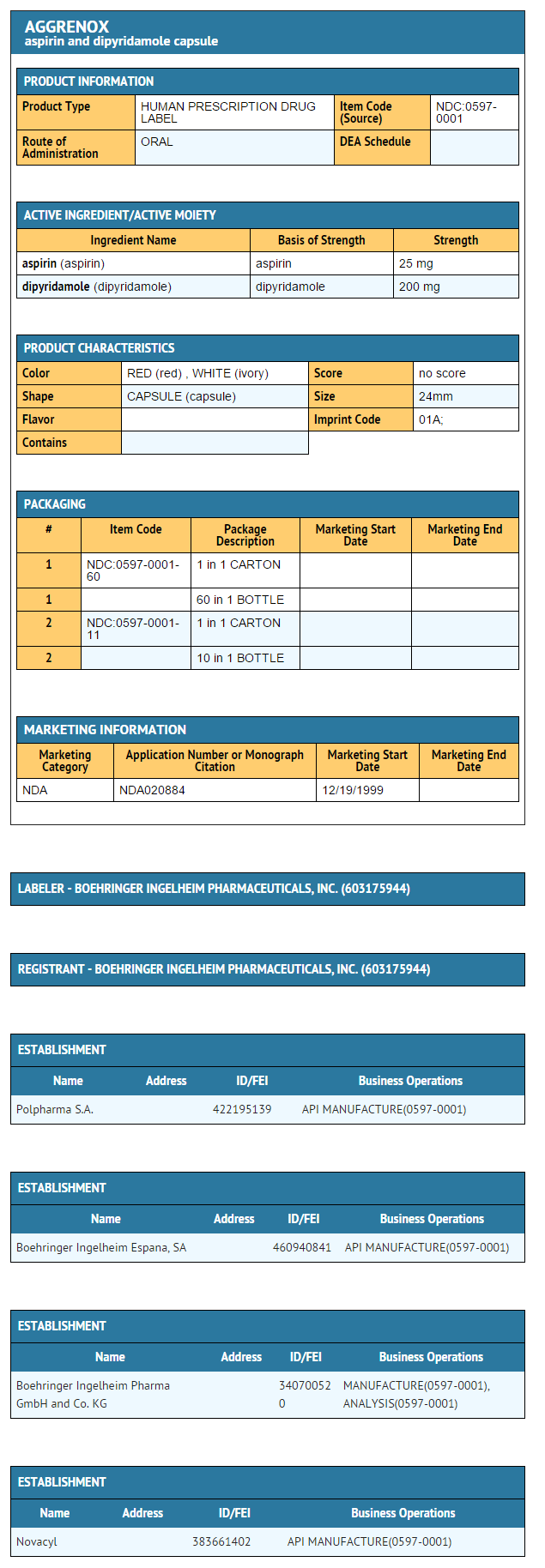
{{#ask: Label Page::Aspirin and dipyridamole |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Risk of Bleeding
- Inform patients that as with other antiplatelet agents, there is a general risk of bleeding including intracranial and gastrointestinal bleeding. Inform patients about the signs and symptoms of bleeding, including occult bleeding. Tell patients to notify their physician if they are prescribed any drug which may increase risk of bleeding.
- Counsel patients who consume three or more alcoholic drinks daily about the bleeding risks involved with chronic, heavy alcohol use while taking aspirin.
Pregnancy
- Inform patients that aspirin is known to be harmful to fetuses and ask the patient to notify them if they are or become pregnant.
Headaches
- Some patients may experience headaches upon treatment initiation; these are usually transient. In case of intolerable headaches, tell the patient to contact their physician.
Dosage and Administration
- Tell patients that aspirin and dipyridamole capsules should be swallowed whole, and not chewed or crushed. If you miss a dose, continue with your next dose on your regular schedule. Do not take a double dose.
Storage
- Inform patients to protect aspirin and dipyridamole from moisture.
Precautions with Alcohol
- Alcohol-Aspirin and dipyridamole interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- AGGRENOX ®[2]
Look-Alike Drug Names
There is limited information regarding Aspirin and dipyridamole Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Dixon BS, Beck GJ, Vazquez MA, Greenberg A, Delmez JA, Allon M; et al. (2009). "Effect of dipyridamole plus aspirin on hemodialysis graft patency". N Engl J Med. 360 (21): 2191–201. doi:10.1056/NEJMoa0805840. PMC 3929400. PMID 19458364 PMID: 19458364 Check
|pmid=value (help). - ↑ "AGGRENOX- aspirin and dipyridamole capsule".