Vertebrobasilar insufficiency other imaging findings
| Vertebrobasilar insufficiency
|
|
Differentiating Vertebrobasilar insufficiency from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Vertebrobasilar insufficiency other imaging findings On the Web |
|
American Roentgen Ray Society Images of Vertebrobasilar insufficiency other imaging findings |
|
Vertebrobasilar insufficiency other imaging findings in the news |
|
Directions to Hospitals Treating Vertebrobasilar insufficiency |
|
Risk calculators and risk factors for Vertebrobasilar insufficiency other imaging findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Other Imaging Findings
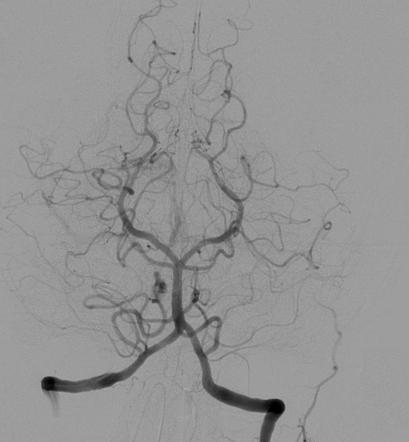
DSA
The digital subtraction angiography (DSA) is the gold stardard to diagnose the VBI. Neither MRA nor CTA reliably delineates the origins of the vertebral arteries, and hence, catheter-based angiography is typically required before revascularization for patients with symptomatic posterior cerebral ischemia.[1] Most cases are performed from a femoral approach, although the brachial route has also been used. The stenotic lesions are crossed and treated with 0.014- or 0.018-inch guidewires and small coronary diameter balloons and stents.The procedure can be performed under local anesthesia, enabling continuous neurological monitoring of the patient.[2]
2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease (DO NOT EDIT)[3]
Vascular Imaging in Patients with Vertebral Artery Disease (DO NOT EDIT)[3]
| Class I |
| "1. Noninvasive imaging by CTA or MRA for detection of vertebral artery disease should be part of the initial evaluation of patients with neurological symptoms referable to the posterior circulation and those with subclavian steal syndrome. (Level of Evidence: C)" |
| "2. Patients with asymptomatic bilateral carotid occlusions or unilateral carotid artery occlusion and incomplete circle of Willis should undergo noninvasive imaging for detection of vertebral artery obstructive disease. (Level of Evidence: C)" |
| "3. In patients whose symptoms suggest posterior cerebral or cerebellar ischemia, MRA or CTA is recommended rather than ultrasound imaging for evaluation of the vertebral arteries. (Level of Evidence: C)" |
| Class IIa |
| "1. In patients with symptoms of posterior cerebral or cerebellar ischemia, serial noninvasive imaging of the extracranial vertebral arteries is reasonable to assess the progression of atherosclerotic disease and exclude the development of new lesions. (Level of Evidence: C)" |
| "2. In patients with posterior cerebral or cerebellar ischemic symptoms who may be candidates for revascularization, catheter-based contrast angiography can be useful to define vertebral artery pathoanatomy when noninvasive imaging fails to define the location or severity of stenosis. (Level of Evidence: C)" |
| "3. In patients who have undergone vertebral artery revascularization, serial noninvasive imaging of the extracranial vertebral arteries is reasonable at intervals similar to those for carotid revascularization. (Level of Evidence: C)" |
References
- ↑ Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL et al. (2013) 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Developed in collaboration with the American Academy of Neurology and Society of Cardiovascular Computed Tomography. Catheter Cardiovasc Interv 81 (1):E76-123. DOI:10.1002/ccd.22983 PMID: 23281092
- ↑ Lee CJ, Morasch MD (2011) Treatment of vertebral disease: appropriate use of open and endovascular techniques. Semin Vasc Surg 24 (1):24-30. DOI:10.1053/j.semvascsurg.2011.03.003 PMID: 21718929
- ↑ 3.0 3.1 Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL; et al. (2011). "2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery". Circulation. 124 (4): 489–532. doi:10.1161/CIR.0b013e31820d8d78. PMID 21282505.