Traveller vaccination japanese encephalitis
To read more about Japanese encephalitis, click here.
|
Traveler Vaccination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]
Disease cause
Transmission
Pigs and various wild birds represent the natural reservoir of this virus, which is transmitted to new animal hosts and occasionally human beings by mosquitoes of the genus Culex.
Culex mosquitoes are primarily day-biting.
Nature of the disease
Mostly asymptomatic. Symptoms could be vary from mild infections that are characterized by febrile headache or aseptic meningitis followed by an uneventful recovery; severe cases have a rapid onset and progression with headache, high fever and meningeal signs.
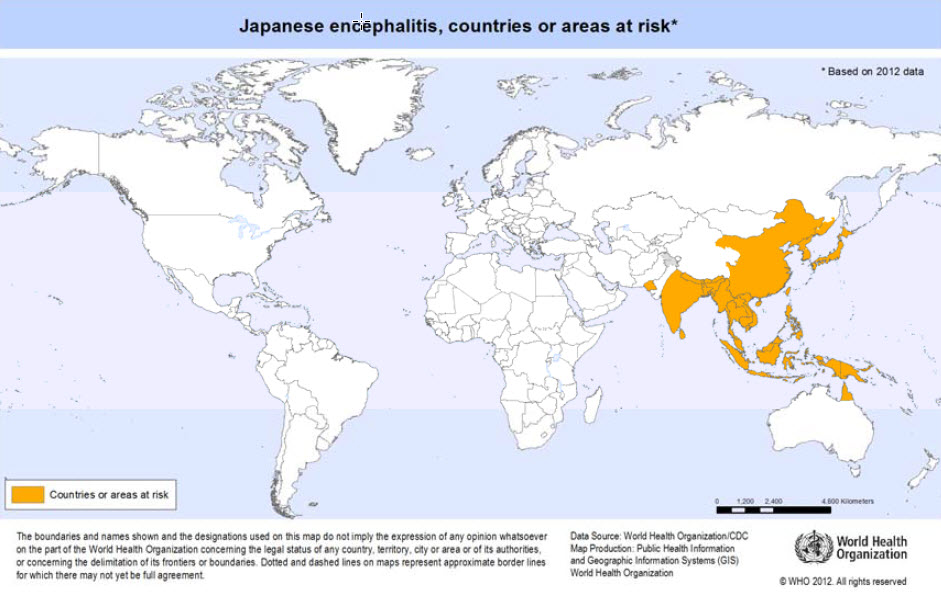
Geographical distribution
Japanese encephalitis virus is the leading cause of viral encephalitis in Asia and occurs in almost all Asian countries. Transmission occurs mainly during the rainy season in south-east Asia but may take place all year round, particularly in tropical climate zones.
Risk for travellers
The risk of japanese encephalitis is very low for most travellers to Asia, particularly for short-term visitors to urban areas. However, the risk varies according to season, destination, duration of travel and activities.
- Vaccination is recommended for travellers with extensive outdoor exposure (such as camping, hiking and working) during the transmission season, particularly in endemic countries or areas where farming involves flooding irrigation.
- Prevention is by avoidance of mosquito bites and by vaccination.
Vaccine
Inactivated Vero cell-derived, live attenuated and live recombinant vaccines are available. Vaccination against japanese encephalitis is recommended for travellers to endemic areas who will have extensive outdoor exposure during the transmission season.
Summary of vaccine data
| Considerations | |
|---|---|
| Type of vaccine and schedules | Japanese encephalitis vaccines fall into 3 classes: |
Inactivated Vero cell-derived vaccines:
| |
Live attenuated vaccines:
| |
Live recombinant (chimeric) vaccines:
| |
| Adverse reactions | Occasional mild local or systemic reactions. |
| Contraindications and precautions |
|